Airway management is a pivotal skill of an anaes-thesiologist and is a critical step in the administration of general anaesthesia. The surest method to secure the airway of a patient is via endotracheal intubation, but as the field has advanced, anaesthesiologists have several non-invasive and less difficult devices and techniques at their disposal to facilitate airway management [1].
Laryngeal mask airway blockbuster (LMA-BT) is a relatively new device in the supraglottic airway devices (SGAD) armamentarium introduced in 2015 and patented in 2016. The manufacturers of LMA-BT claim that LMA-BT has a superior ventilation capability and a better route for intubation via the trachea. The LMA-BT is made of malleable soft silicone which causes minimal oropharyngeal trauma. The airway tube is short and angulated at over 95 degrees to conform to the oropharyngeal curve, making insertion easier and less painful. The curve of LMA-BT, specially designed for rapid blind intubation, allows the endotracheal tube (ETT) to be directed at a 30-degree angle towards the laryngeal opening, increasing the success rate of blind intubation. In addition, the LMA-BT also provides better airway sealing pressures at lower volumes. Further, it also has a gastric port, and the entrance and outflow of this gastric port are designed in such a way to make Ryle’s tube insertion easier [2, 3].
I-Gel LMA is a polyvinyl chloride (PVC) and latex-free second-generation SGAD composed of a thermoplastic elastomer. It has a non-inflating cuff, an integrated biting block, and a gastric port. Just above the distal opening, there is an epiglottic rest/ridge. The ‘buccal cavity stabilizer,’ which refers to the expanded part of the body, eases the insertion and prevents inadvertent rotation once in place. The insertion depth is shown by a horizontal bar indicator at the proximal end. It is quick, easy, and reliable to insert and has widely gained popularity as a conduit for endotracheal intubation. In this regard, several studies have reported successful blind or fibre-optic-guided intubation through I-Gel [4–6].
In a preliminary literature review of the Medline & Scopus databases, no systematic reviews or meta-analyses on LMA-BT were found. Of the existing data, only a few studies are present on LMA-BT, which were carried out on the Indian population. To our knowledge, this is the first study to compare LMA-BT with I-Gel LMA for blind tracheal intubation.
The primary aim of this study was to evaluate the first-pass success rate of blind tracheal intubation through LMA-BT and I-Gel LMA. To guide clinical practice, it is imperative to understand the comparative effectiveness of the 2 supraglottic airway devices used in our study for blind tracheal intubation. Hence, this study was based on the hypothesis that use of LMA-BT as an airway device for blind tracheal intubation results in improved outcomes in terms of first-pass success rate of blind tracheal intubation.
METHODS
We conducted this single-blind, prospective study in a tertiary care hospital in Western Uttar Pradesh from September 2021 to March 2022. After ethical approval from the institutional ethical committee, (GIMS/IEC/HR/2021/23) the study was registered with ctri.nic.in. (CTRI/2021/09/036798). The study adheres to the Consolidated Standard of Reporting Trials (CONSORT) [7] statement depicted in the flowchart (Figure 1). Written informed consent was obtained and 100 patients were included We included patients with ASA grade I–III, between the age group of 18 to 60 years, undergoing elective surgery under general anaesthesia with endotracheal intubation. Patients with an ASA status IV or V, who needed rapid sequence intubation (pregnancy, symptomatic gastroesophageal reflux disease), or had known challenging ventilation or intubation parameters (Inter-incisor gap < 3 cm, Mallampati grade ≥ 3, restricted neck movement), patients with obesity (body mass index > 35 kg m–2), significant pulmonary comorbidity, and patients who refused to participate were excluded from the study.
We randomised the patients into 2 groups using computer-generated random numbers. In group 1 (n = 50) blind tracheal intubation was performed through LMA-BT, and in group 2 (n = 50) blind tracheal intubation was done through I-Gel. Allocation concealment was done using the sealed envelope technique. The blind tracheal intubation with either of the LMAs was performed only by anaesthesiologists with experience of over 25 successful insertions and intubations through the study devices. Observation and data collection was done by an independent anaesthesiologist, who was not part of the study.
All the patients were nil per oral (NPO) overnight and given oral alprazolam 0.25 mg the night before and on the morning of the operation. Routine monitoring of 5-lead electrocardiogram (ECG), heart rate (HR), oxygen saturation (SpO2), and non-invasive blood pressure (NIBP) were performed upon arrival in the operating room. We administered ringer lactate after securing intravenous 18/20 G access. After 3-minute pre-oxygenation with 100% oxygen, anaesthesia induction was done with the administration of intravenous glycopyrrolate 0.2 mg, fentanyl 2 µg kg–1, and propofol 2 mg kg–1, followed by neuromuscular blockade with an injection of vecuronium 0.1 mg kg–1 after confirming adequate mask ventilation. Patients were ventilated for 3 minutes with a mixture of oxygen and a 2% end-tidal concentration of sevoflurane, followed by insertion of the appropriate size LMA, as per the manufacturer’s guidelines [2, 4].
LMA insertion
We inserted the LMA in a neutral neck position after lubrication with a water-soluble jelly in both the groups. The cuff of LMA-BT was inflated as per recommendations to 60 cm H2O pressure [2].
Bilateral equal chest rise, and square-wave capnography confirmed the adequacy of ventilation through LMA. The number of attempts required for LMA insertion was noted, and insertion was labelled as failed in cases of unsuccessful ventilation after 3 attempts. In such cases, the patient’s trachea was intubated. The ease of LMA placement was assessed using a subjective scale ranging from 1 to 4 (1 = no resistance, 2 = mild resistance, 3 = moderate resistance, 4 = inability to place the device) [8]. We defined the insertion time for LMA as the time from the opening of the patient’s mouth for LMA insertion to the appearance of the first square wave capnography curve on the monitor. The airway leak pressure of each of the LMA was measured with the expiratory valve fully closed and a fresh gas flow set at 3 L min–1. The pressure at which equilibrium was seen on the pressure gauge was noted as the airway leak pressure (not allowed to exceed 40 cm H2O) [9]. A well-lubricated nasogastric tube (NGT) was inserted through the provided gastric port through each of the LMAs, and its position was confirmed by auscultation over the epigastrium. We categorised the insertion of NGT as easy or difficult. Insertion with one attempt was labelled as easy, greater than one as difficult, and failure to insert after 3 attempts as failed.
The position of LMA in reference to the laryngeal opening was determined by the insertion of a flexible intubation video endoscope (KARL STORZ with C-MAC monitor, Tuttlingen, Germany). The glottic view through the LMA, just proximal to the ventilating orifice, was graded as follows: grade 1 – vocal cords entirely visible, grade 2 – vocal cords/arytenoids partially visible, grade 3 – epiglottis only visible, grade 4 – no laryngeal structure visible [10, 11].
Tracheal intubation
After the laryngeal grading, the flexible video endoscope was withdrawn, and patients were ventilated for 1 min through the LMA. We attempted blind tracheal intubation through LMA-BT in group 1 and through I-Gel LMA in group 2. For LMA-BT, blind tracheal intubation was done according to the manufacturer’s guidelines [2]. For I-Gel, we inserted the tracheal tube according to the manoeuvre suggested by Halgawi et al. [5] (rotation of ETT through 90 degrees counterclockwise before insertion to point the tube’s bevel posteriorly). If we encountered resistance during intubation in either of the devices, we performed the following manoeuvres.
Twisting of ETT and gentle up and down movement of the tube inside LMA.
Application of external laryngeal manipulation by applying backward pressure on thyroid cartilage.
In both groups, we used standard cuffed PVC tubes for endotracheal intubation. A size 7 ETT was inserted through size 3 LMAs, and size 7.5 through size 4 LMAs.
The number of attempts of blind intubation was noted, and a maximum of 3 attempts were allowed. In case of failure of blind intubation through LMA, surgery was continued with the LMA in place or intubation by direct laryngoscopy. We confirmed the correct placement of ETT by chest rise, bilateral equal breath sounds on auscultation, and square wave capnography. We defined the insertion time of ETT through LMA as the time elapsed since disconnecting the breathing circuit from the LMA to the successful appearance of the capnographic curve after the connection of ETT to the circuit. The insertion time of only the successful attempt at blind tracheal intubation was recorded. This was followed by the removal of LMA as per the manufacturer’s recommendations using the stabilising rod provided with LMA-BT in both the groups for LMA removal. Time of removal of LMA after intubation was defined as the time elapsed from disconnection of the breathing circuit to the reappearance of the capnographic curve on the monitor. In case of accidental extubation at the time of LMA removal, the patient was re-intubated with direct laryngoscopy, and the case was excluded from the study.
Intraoperatively haemodynamic parameters – HR, ECG, SpO2, NIBP, and end-tidal carbon dioxide concentration (EtCO2) – were noted every minute for the first 10 minutes followed by every 10 minutes umtil the end of surgery.
At the end of the surgery, following the reversal of neuromuscular blockade, the patient was extubated after adequate recovery and responsiveness. We observed the LMAs and ETT tubes for any visible soiling with blood or blood-tinged secretions. Patients were assessed for sore throat, hoarseness of voice, and cough on arrival in the postoperative care unit (PACU) and at 24 hours by an investigator who was blinded to the device used. A day prior to surgery, patients were told how to score the severity of postoperative sore throat, hoarseness of voice, and cough [12–14]. The scoring system for the assessment of sore throat, hoarseness of voice, and cough was used as described by Harding et al. [12] (Table 1).
TABLE 1
Postoperative sore throat, hoarseness of voice, and cough scoring [10]
Outcome
The primary aim of this study was to evaluate the first-pass success rate of blind tracheal intubation through LMA-BT and I-Gel LMA. The secondary objectives noted were as follows: attempts of LMA insertion, ease of LMA insertion, total time taken for LMA insertion, airway seal pressure of LMA, ease of NGT insertion through LMA, fibre-optic grading of laryngeal view through LMA, the overall success rate of intubation through LMA, insertion time for ETT, time for LMA removal after intubation, haemodynamic parameters, and complications, if any.
Sampling and statistical analysis
Sample size was calculated using open Epi software version 2.3.1 at a confidence level of 95% and 80% power of the study. Endigeri et al. [3] conducted a study comparing the success rate of Blockbuster vs. Fastrach LMA as a conduit for blind endotracheal intubation. In their study, the success rate of first pass intubation was 90% in the blockbuster group and 66% in the I-Gel LMA Fastrach group. Based on this study, the first-pass success rate for intubation through LMA was chosen for calculation of sample size. The sample size calculated was 47 patients in each group. We recruited 50 patients in each group to increase the power of the study.
We performed statistical analysis using SPSS for Windows, version 24.0 (IBM Corp., USA). The one-sample Kolmogorov-Smirnov test was used to evaluate the normal distribution of data. Continuous variables were reported as mean and standard deviation and were compared across the groups using Student’s t-test. Age distribution was also analysed using Student’s t-test. Categorical variables were reported as count and frequency/percentage and associations and, were tested using the χ2 test. Effect size was measured as relative risk (RR). The a level was set at 0.05 for statistical significance.
RESULTS
In this study, we randomly divided 100 patients into 2 groups. The groups were comparable regarding baseline demographic parameters like age, gender, BMI, ASA grading, Mallampati scoring, and duration of surgery (Table 2).
TABLE 2
Demographic parameters and duration of surgery
The 2 groups showed a statistically significant difference in a comparison of the first-pass success rate of blind tracheal intubation (P < 0.019) (Table 3). In group 1, the first-pass success rate was 80% with LMA-BT compared to 58% with I-Gel (RR = 0.476 [0.25–0.905]). The overall success rate of intubation was 94% with LMA-BT and 68% with I-Gel (P < 0.005) (Table 3). In group 1, only 3 patients required direct laryngoscopy for intubation (6%) while 16 patients (32%) failed to get intubated through I-Gel LMA. In a comparison of time for intubation in both groups, the results showed that with LMA-BT the intubation time was significantly shorter than in the I-Gel group (19.36 ± 1.72 vs. 23.11 ± 1.75) (P < 0.001) (Table 3).
TABLE 3
Comparison of the first-pass success rate of blind tracheal intubation through LMA-BT (group 1) and I-Gel LMA (group 2)
The number of insertion attempts required for successful LMA placement was comparable among the groups (P = 0.202) (Table 4). Although the first attempt success insertion rate of LMA was higher in group 2 as compared to group 1 (98% vs. 92%), the difference was statistically insignificant (RR = 4.00 [0.46–34.54]). Similarly, the ease of placement of LMA was higher in the I-Gel group as compared to the LMA-BT group, but the comparison was again statistically insignificant (P = 0.330). The time required for LMA placement was comparable in both groups (25.63 ± 4.11 vs. 24.44 ± 3.92) (P = 0.141), as was the time for LMA removal after intubation (20.37 ± 1.85 vs. 19.67 ± 2.19) (P = 0.087). There was no incidence of accidental extubation at the time of LMA removal in either of the groups. The airway seal pressure achieved with LMA-BT was significantly higher (28.67 ± 0.48) as compared to I-Gel LMA (24.33 ± 1.06) (P < 0.001) (Table 4).
TABLE 4
Comparison of SGAD parameters
On the assessment of the laryngeal grading by a flexible video endoscope, we observed that the view was grade 1 in 56% (28 patients) and grade 2 in 24% of cases (12 patients) in the LMA-BT group. In group 2, 30% of cases had a grade 1 (15 patients) laryngeal view, and a grade 2 view was seen in 34% of cases (17 patients) (Table 4). On comparing the ease of insertion of NGT between the 2 groups, it was easy in 84% of patients in group 1 and in 80% of patients in group 2.
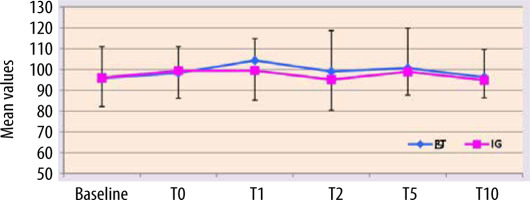
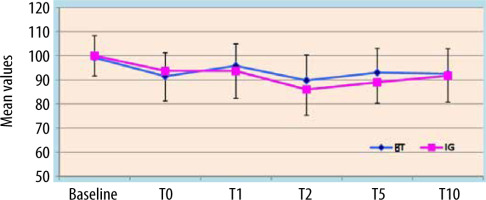
Post-operative interviews revealed a higher incidence of sore throat in group 2 immediately after arrival in PACU (P = 0.031) (Table 5). In the comparison of cough, hoarseness of voice, and device soiling between the groups, no statistically significant difference was noted (Table 5). The haemodynamic parameters were comparable between the 2 groups (Figures 2 and 3).
TABLE 5
Postoperative complications
DISCUSSION
Our study revealed that the first attempt success rate of blind tracheal intubation was 80% with LMA-BT and 58% with I-Gel LMA, and the difference was statistically significant. Edingeri et al. [3] also reported a higher (90%) success rate of blind tracheal intubation in the first attempt with LMA-BT as compared to LMA Fastrach. Although the first-pass success rate of blind intubation through LMA-BT in their study was slightly higher than ours (90% vs. 80%); this difference can be attributed to the different ETT used in the 2 studies. We used PVC ETT for intubation in both groups because it is widely and easily available across all set-ups in the country.
Although I-Gel has been designed for fibre-optic-guided intubation, there are several studies evaluating its use as a conduit for blind tracheal intubation [15, 16]. The success rate of I-Gel intubation in our study is like that obtained by Sameer et al. [15], in which intubation through I-Gel was compared with LMA Fastrach. In contrast, other researchers [17–19] reported a lesser (around 36.6%) first-pass rate with I-Gel. The application of external laryngeal manipulation and 90-degree counter- rotation of ETT during insertion (as suggested by Halgawi et al.) [5] for the optimal alignment of ETT with the glottis opening could have resulted in a better success rate in our study.
In our study, LMA-BT was found to be a better intubating device than I-Gel LMA as the overall success rate of blind intubation, insertion time for endotracheal tube, and fiberoptic view of larynx were significantly better in the LMA-BT group. Our findings are like previous studies done on individual devices [3, 15, 16, 19–21]. The higher success rate of intubation in the first attempt with the use of LMA-BT can be because of its angulated design (95-degree angulation of the airway tube). This may cause better alignment of the LMA with the hypopharynx. The presence of a special ridge in LMA-BT may also enhance the success rate of endotracheal intubation as it directs the ETT towards the laryngeal opening at an angle of 30 degrees [2]. However, when compared to other non-intubating LMAs, I-Gel LMA allows passage of larger size ETT. However, the lesser curvature of its airway tube directs the ETT posteriorly, which increases the risk of oesophageal intubation or impingement on arytenoids [5].
The airway seal pressure is useful in quantifying the airway sealing by LMAs to decrease the aspiration risk. The airway seal pressure of LMA-BT was significantly greater than that of I-Gel. We can attribute this to a larger capacity of the cuff of the device, resulting in better airway seal pressures and contouring with the laryngeal and pharyngeal walls of the patient [3, 21]. LMA-BT also gives the advantage of allowing passage of a larger size NGT as compared to I-Gel. The size of the NGT inserted was 12 F and 14 F through 3 and 4 sizes of I-Gel, respectively. It was possible to insert 14 F NGT through both sizes 3 and 4 of LMA-BT. This might have a bearing on hastening the return of bowel function and diminish the risk of anastomotic leakage after abdominal surgery [22].
In both groups, there was a low incidence of post-operative problems. The most common complication reported in both groups was sore throat. The incidence of sore throat was statistically higher in the I-Gel group after arrival in PACU (P = 0.031). We observed no significant differences among the 2 groups with regards to cough, hoarseness of voice, and the soiling of airway devices. All the complications reported were self-limiting, requiring no intervention. Similar results have also been reported by other studies [3, 15, 21].
There were few limitations of our study. Firstly, it was a single-centre, single-blind study. To reduce the observer bias, we tried to restrict the number of subjective parameters and include most of the parameters that were objective in nature. For assessment of subjective parameters standardised scales were used. Next, we excluded patients with predicted difficult airway as defined by the pre-set criteria of the study. Further studies to evaluate the usefulness of LMA-BT for blind intubation in patients with difficult airway need to be carried out.
The results of the present study showed that LMA-BT has an advantage over I-Gel LMA as it proved to be a faster and predictable device for securing the airway with greater first pass endotracheal intubation rate and better sealing pressure. This study is intended to present practical values to the airway managers for blind tracheal intubation of patients.
CONCLUSIONS
LMA-BT is a superior device as compared to I-Gel as a conduit for blind endotracheal intubation (80% vs. 58%, respectively). It also results in faster (19.36 ± 1.72 vs. 23.11 ± 1.75 seconds) and smoother intubation as compared to I-Gel, and it maintains higher airway seal pressure with lesser incidence of postoperative sore throat. Further studies comparing various intubating devices with LMA-BT are recommended.