To the Editor,
The infraclavicular approach (subclavian approach) to the central vein is most often selected for implantation of a tunnelled Hickman/Broviac cathe-ter because central venous catheter (CVC) insertion into the upper body is optimal considering patient comfort as well as the risk of infection [1] and intravenous thrombosis [2, 3]. How-ever, the actual puncture site for a real-time ultrasound-guided infraclavicular axillary vein approach is at the level of the axillary vein in a much more lateral location than that for the traditional landmark infraclavicular approach to the subclavian vein. This is because an optimal view of the subclavian vein is difficult to obtain with a real-time ultrasound-guided technique, as the ultrasound beam is restricted by the clavicle [4]; the younger the patient, the greater would be its influence because of the width of the ultrasound probe. As a result, Hickman/Broviac catheter bending due to a sharply curved angle in the subcutaneous tunnel may occur when the subcutaneous tunnel exit needs to be created inside the patient’s nipple to obtain sufficient tunnel length, especially in young paediatric patients. When the internal jugular vein is chosen as an alternative puncture site, adverse events of catheter bending and occlusion may occur because the puncture direction to the target vein and the direction of the subcutaneous tunnel become very steep [5].
Figure 1 shows a representative case of a 2-year-old patient (height 82 cm, body mass 10 kg) who required a Hickman catheter for chemotherapy for leukaemia. As an infraclavicular axillary vein approach with a real-time ultrasound-guided technique is the standard approach for Hickman/Broviac catheter implantation in our institution, the paediatric surgeons scanned the axillary veins of the patient in the Trendelenburg position on both sides and confirmed that the veins were open and intact. The right side was chosen because catheter tip malposition [6] and risk of superior vena cava (SVC) perforation [7, 8] have been reported for CVCs inserted from a patient’s left side, even though the success rate to puncture the target vein via the real-time ultrasound-guided left supraclavicular CVC approach is reported to be higher than that with the right supraclavicular approach [9]. Indeed, it is reported that 3.4% of the CVC tips inserted via the left supraclavicular approach using the real-time ultrasound-guided technique were positioned touching the lateral wall of the SVC [6].
FIGURE 1
A Hickman catheter implanted via the right real-time ultrasound-guided infraclavicular axillary vein approach with a subcutaneous tunnel with its exit inside the ipsilateral nipple to obtain sufficient subcutaneous tunnel length. The chest X-ray shows that the calibre change portion of the Hickman catheter was positioned just at the sharp curve in the subcutaneous tunnel, and its lumen was bent and occluded (arrow)

The vein puncture and guide wire insertion were performed successfully via the short-axis out-of-plane real-time ultrasound-guided right infraclavicular axillary vein approach. The needle insertion angle was gentler when using the long-axis in-plane approach; however, the puncture site of the needle was much more lateral than that for a short-axis out-of-plane approach because of the length of the ultrasound probe. The running route of the subcutaneous tunnel was designed by laying the Hickman catheter (Medicon Inc., Osaka, Japan) on the patient’s chest wall. The subcutaneous tunnel exit needed to be made more medially from the patient’s nipple or more laterally from the axillary midline to obtain sufficient tunnel length owing to the distance between the suture cuff and the calibre change portion of the implanted catheter. The medial side of the nipple was chosen for the subcutaneous tunnel exit rather than the lateral side of the axillary midline, since the implanted catheter engraftment in the subcutaneous tunnel was considered uncertain, with less subcutaneous fat, and was more painful and uncomfortable because subcutaneous tissue movement is more associated with upper limb movement on the lateral side of the axillary midline.
After the subcutaneous tunnel was created and the Hickman catheter was inserted, the cut length of the Hickman catheter tip was determined using a C-arm X-ray machine so that it came to the carina level. However, the calibre change portion of the Hickman catheter, where the catheter is soft and its lumen is easily occluded by bending, was positioned coincidentally just at the sharp curve of the subcutaneous tunnel, and its lumen was bent (Figure 1). Blood aspiration with a syringe was impossible. Therefore, the fixation suture on the catheter should be released to withdraw the side of the catheter tip for approximately 1 cm and to correct the running route of the subcutaneous tunnel and bent catheter in the subcutaneous tunnel. As a result, the Hickman catheter was fixed again with the catheter tip located shallower than the carina level (Figure 2). Six days after the catheter implantation, the patient required a new Hickman catheter because the original Hickman catheter gradually became shallower, and its tip was lost in the ipsilateral jugular vein (Figure 3).
FIGURE 2
Chest X-ray showing the Hickman catheter fixed after being withdrawn approximately 1 cm to solve the bending problem. The tip of the Hickman catheter was withdrawn approximately 1 cm to solve the bending problem (arrow) in the subcutaneous tunnel, and the catheter was fixed with its tip located shallower than the carina level
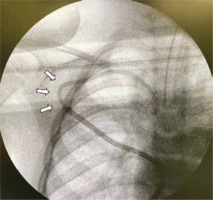
FIGURE 3
Chest X-ray showing the Hickman catheter with the catheter tip lost in the ipsilateral jugular vein. The Hickman catheter became shallower, and its tip became lost in the ipsilateral jugular vein (arrow) 6 days after implantation

In such cases, real-time ultrasound-guided supraclavicular cannulation of the brachiocephalic vein [10, 11] is a practical alternative for Hickman/Broviac catheter implantation, whose puncture site is located much more medially than that of the real-time ultrasound-guided infraclavicular axillary vein approach, to obtain sufficient subcutaneous tunnel length and to prevent the implanted catheter from bending and occlusion while following a sharply curved angle in the subcutaneous tunnel as with the real-time ultrasound-guided infraclavicular axillary vein approach. The step-by-step procedures for real-time ultrasound-guided supraclavicular tunnelled Hickman/Broviac catheter implantation were introduced in our previous paper with figures and a video [5]. As shown in Figure 4, the puncture needle and its entire passage into the target brachiocephalic vein are visualised in a long-axis in-plane view during the puncture procedure with the real-time ultrasound-guided supraclavicular approach. The brachiocephalic vein is larger than that of the internal jugular or subclavian vein because it is located more proximally than their confluence. In contrast, the axillary vein is smaller than the subclavian vein because it is located more peripherally [12]. The subcutaneous tunnel of the Hickman/Broviac catheter inserted via the supraclavicular approach passes over the clavicle [5]. To prevent accidental removal of the catheter during manipulation to create the subcutaneous tunnel and catheter fixation (a pitfall of the right supraclavicular approach for CVC or Hickman/Broviac catheter implantation), it should be noted that the CVC insertion depth via the right supraclavicular approach is significantly shorter than that of the right jugular vein or the left supraclavicular approach to locate the catheter tip at the carina level [6].
FIGURE 4
Real-time ultrasound-guided supraclavicular approach to the right brachiocephalic vein. The puncture needle (arrow) and its entire passage into the target brachiocephalic vein are visualised in a long-axis in-plane view during the puncture procedure via the real-time ultrasound- guided supraclavicular approach

This paper highlights the real-time ultrasound-guided supraclavicular approach as a practical alternative for real-time ultrasound-guided infraclavicular axillary vein Hickman/Broviac catheter insertion, especially in young paediatric patients, to prevent the implanted catheter from bending and occlusion while following a sharply curved angle in the subcutaneous tunnel, when its exit should be created inside the patient’s nipple to obtain sufficient subcutaneous tunnel length.




