Lumbar spine surgery is one of the most frequently performed surgical procedures, which necessitates extensive dissection of subcutaneous tissues, bones, and ligaments. As a result, a significant degree of postoperative pain occurs that lasts for 4–5 days, with the highest pain scores recorded during the first 24 hours after surgery [1].
Through the blocking of pain transmission signals, the use of combined regional and general anaesthesia lowers surgical stress reactions, which makes it easier to regulate pain, ambulate more quickly, recover functionally, and help prevent the emergence of chronic pain syndromes [2, 3].
The thoracolumbar interfascial plane block (TLIP), which also targets the dorsal rami of the thoracolumbar nerves as they pass through the paraspinal musculature, was initially introduced in 2015 by Hand et al. [4] (between the multifidus muscle and the longissimus muscle).
By aiming the injection in the plane between the longissimus and iliocostalis muscles (mTLIP), which helps prevent the distribution of local anaesthetic to the ventral ramus and neuraxial region, Ahiskalioglu et al. changed this approach in the following years [5] to increase its safety profile. Additionally, compared to the standard TLIP, the entire volume of local anaesthetic is kept in the intermuscular region for a longer period, boosting block density and duration.
There are a limited number of studies [5–7] investigating the analgesic efficacy of mTLIP block. Moreover, there is a lack of clarity regarding the optimal dose, ideal local anaesthetic volume, and concentration for mTLIP block in lumber spine surgery.
This study was designed to investigate the anal-gesic efficacy of two different volumes of bupivacaine 0.25% (20 mL and 10 mL) for ultrasound- guided mTLIP block in patients undergoing lumbar spine surgeries. We hypothesized that increasing the volume of local anaesthetic in interfascial plane blocks would decrease the total 24 hours postopera-tive morphine consumption and increase the total analgesic duration.
METHODS
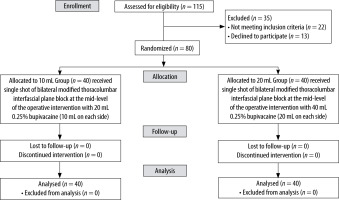
This randomized, controlled, double-blinded study was conducted after receiving approval from the Research Ethics Committee of our institution (ID: MD-307-2020). The study was registered at clinicaltrials.gov (ID: NCT 05276908) before patient enrolment. All patients gave their written, informed consent. The Consolidated Standards for Reporting Trials (CONSORT) guidelines were followed.
The study comprised eighty patients with an ASA physical status of I–II, a BMI of 20–35 kg m–2, and ages ranging from 20 to 65 years who were sche-duled for lumbar spine procedures involving one to three consequent lumbar vertebrae under general anaesthesia. Patients who had previously undergone lumbar surgery, patients who were scheduled for extensive lumbar spine procedures like large tumour excisions or scoliosis correction, patients who had severe neurological compromise (severe muscle weakness like foot drop or sphincter disorders like urinary incontinence), patients with coagulopathies, and patients with infection at the block site were all excluded from the study.
Intravenous access was placed in the operation room, and Ringer’s acetate was started. An electrocardiogram, non-invasive blood pressure monitoring, and pulse oximetry were all attached as standard patient monitoring devices. All patients received an IV premedication of midazolam 0.02 mg kg–1 30 minutes before surgery.
Using computer-generated random numbers stored in sealed envelopes, patients were randomly assigned to one of the two groups. Group 10 mL: 20 mL (2 × 10 mL) bilateral injection of 0.25% bupivacaine for mTLIP block at the mid-level of surgical intervention. Group 20 mL: bilateral mTLIP block with 40 mL of 0.25% bupivacaine at the mid-level of the surgical operation (20 mL on each side). An anaesthesiologist who was unrelated to the study prepared the specific local anaesthetic combination solutions. The patient’s group assignment was concealed from the patient and the anaesthe-siologist who was involved in the intraoperative and postoperative data collection.
Using IV fentanyl at a dosage of 2 μg kg–1 and IV propofol at a dosage of 2 mg kg–1, general anaes-thesia was induced. Tracheal intubation was aided by 0.5 mg kg–1 IV atracurium. Anaesthesia was maintained with the help of 0.8% isoflurane in oxygen-enriched air (FiO2 = 0.5). Every 25 minutes, 0.1 mg of atracurium was administered as a maintenance dose. The patient was positioned in the prone posture. Then mTLIP was conducted.
Modified thoracolumbar interfascial plane block (mTLIP) technique
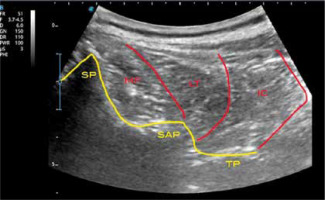
At the intended lumbar level, a Siemens Acuson X300 Ultrasound System curvilinear array ultrasound probe was positioned. The corresponding spinous process and interspinal muscles were identified, and the probe was moved laterally to identify the longissimus muscle and iliocostalis muscle. Under ultrasound guidance, a 38-mm, 22-gauge (22-G, 50-mm “Stimuplex”; BBraun, Melsung, Germany) regional block needle was advanced medially to laterally through the longissimus muscle belly and at an angle of 15° toward the iliocostalis muscle. Following the injection of 2–3 mL of isotonic saline solution to confirm the correct needle tip position, 0.25% bupivacaine (10 or 20 mL, depending on randomization) was slowly injected while being carefully monitored for the spread of local anaesthetic into the fascial plane between the longissimus and iliocostalis muscles. The same process was repeated on the contralateral side (Figure 1).
FIGURE 1
Ultrasound image of the thoracolumbar spine. IC – iliocostalis muscle, LT – longissimus thoracis muscle, MF – multifidus muscle, TP – transverse process, SAP – superior articular process, SP – spinous process
After ruling out other potential causes, rescue analgesia of fentanyl 1 μg kg–1 was administered if the mean arterial blood pressure or heart rate rose above 20% of baseline preoperative levels. For fluid replacement, maintenance, and losses, ringer solution was injected. The patients were mechanically ventilated with a goal to maintain end-tidal CO2 at 30–35 mmHg.
Hypotension (a reduction of more than 20% of the baseline reading) was treated with 5 mg of ephedrine, which were repeated to maintain the mean arterial pressure (MAP) above 70 mmHg. Bradycardia, defined as a heart rate (HR) less than 50 beats per minute, was treated with 0.4 mg atropine. Neostigmine (0.05 mg kg–1) and atropine (0.02 mg kg–1) were used to reverse the remaining neuromuscular blockade at the end of the procedure, and the patients were extubated once their airway reflexes had fully recovered.
The patients were then shifted to the post- anesthesia care unit, where the MAP, HR, and SpO2 were monitored until the patient was fully awake (sustained voluntary head elevation for 5 seconds), at which point the numeric rating scale (NRS) was evaluated and the extended modified Bromage scale was used to gauge the motor function in the lower limbs [8].
After that, the patient was transferred to the ward. Infusions of 1 gm paracetamol were given intravenously to all patients every six hours for the first 24 hours following surgery. Postoperative pain assessment using NRS, and morphine administration were started immediately postoperative and then every two hours for 24 hours. If the patient’s NRS > 3, additional rescue analgesia in the form of IV morphine 0.05 mg kg–1 boluses were administered. A morphine dose of 0.5 mg kg–1 per 24 hours is the maximum permitted dose. If the patient needed more than two doses of rescue analgesia in the first hour following surgery, the block was deemed to have failed. Ondansetron 0.1 mg kg–1 IV was used to treat postoperative nausea and vomiting (PONV).
Total morphine consumption in the first 24 hours postoperatively was set as the primary outcome of this study. The following were set as secondary outcomes: (i) time to first rescue analgesia (measured from time of block administration to time of rescue analgesia administration); (ii) NRS, both at rest and during movement: 30 minutes, 2, 4, 6, 8, 12, 16, 20, and 24 hours postoperatively; (iii) total intraoperative fentanyl dose; (iv) baseline preoperative HR and MAP readings were taken, immediately before surgical incision, at 30-minute intervals intraoperatively, and at 30 minutes and 2 hours postoperatively; (v) block related complications such as local anaesthetic toxicity, hematoma formation, and lower limb weakness; (vi) nausea and vomiting scores using a four-point verbal scale (none = no nausea; mild = nausea but no vomiting; moderate = vomiting one attack; severe = vomiting > one attack).
Sample size calculation
The sample size calculation was performed using G*Power 3.1.9.2 (Universitat Kiel, Germany). A pilot study of 10 cases in each group was performed and the mean (± SD) of total morphine consumption in the first 24 hours (the primary outcome) was 5 ± 3.16 µg in group T 10 and 2.5 ± 2.5 µg in group T20. Based on the following factors, the sample size was determined: 0.88 effect size, 95% confidence limit, 95% power of the study, group ratio 1 : 1 and five cases were added to each group to overcome dropout. As a result, the sample size is increased to total eighty patients (forty in each group).
Statistical analysis
For statistical analysis, SPSS v27 (IBM, Chicago, IL, USA) was used. Histograms and the Shapiro-Wilks test were used to assess the normality of the data distribution. The unpaired student t-test was used to examine the mean and standard deviation (SD) of quantitative parametric data. Quantitative non-parametric data are reported as median and interquartile range (IQR) and are subjected to Wilcoxon and Mann-Whitney tests for analysis. Using c2 or Fisher’s exact tests, qualitative variables were assessed as frequencies and percentages (%). The three metrics were compared within the same group using repeated measures ANOVA. Statistical significance was defined as a two-tailed P-value ≤ 0.05.
RESULTS
To determine eligibility, one hundred and fifteen patients underwent screening. Thirteen patients declined to participate, and twenty-two were eliminated because they failed to meet the inclusion criteria. A total of eighty patients, forty in each group, participated and completed the trial. The eighty patients were all followed up and statistically analyzed (Figure 2). Both study groups’ demographic information and surgical time were comparable (Table 1).
TABLE 1
Patients’ characteristics of the studied groups
There was no significant difference in the total dose of postoperative morphine consumption over the first 24 hrs. as it was higher in 10 mL Group (6.20 ± 2.18) compared to 20 mL Group (5 ± 0.00) (P = 0.056). On the other hand, the time of the first request for rescue morphine was significantly lower in the 10 mL Group (7.80 ± 3.98) compared to the 20 mL Group (13.23 ± 3.00) (P < 0.001).
The number of patients who required rescue morphine in the postoperative 24 hours were significantly higher in the 10 mL Group compared to the 20 mL Group (P = 0.007), with statistically significant differences in the first 12 hours and insignificant differences in the second 12 hours between both groups (P ≤ 0.001 and 0.431, respectively) (Table 2).
TABLE 2
Analgesic requirements of the studied groups
Data of time to first request of rescue morphine, total morphine consumption and total fentanyl dose are presented as mean ± SD. Data of patients received rescue morphine, request of rescue morphine in first and second 12 h and Patients received intra-operative fentanyl more than induction dose are presented as number (percentage).
NRS at rest in all time measurements (30 minutes, 2, 4, 6, 8, 12, 16, 20 and 24 hours postoperative) was significantly higher in 10 mL Group compared to 20 mL Group (P = 0.002, 0.037, 0.050, 0.024, 0.002, 0.009, 0.041, 0.002 and 0.002, respectively) (Table 3).
TABLE 3
NRS at rest and movement
Similarly, NRS during movement in all time measurements (30 minutes, 2, 4, 6, 8, 12, 16, 20 and 24 hours postoperative) was significantly higher in 10 mL Group compared to 20 mL Group (P < 0.001, < 0.001, < 0.001, < 0.001, < 0.001, 0.001, 0.002, < 0.001, and < 0.001, respectively) (Table 3).
Total fentanyl dose was significantly higher in 10 mL Group compared to 20 mL Group (P = 0.002). A number of patients receiving intra-operative fentanyl more than induction dose was significantly higher in 10 mL Group compared to 20 mL Group (P = 0.003) (Table 2).
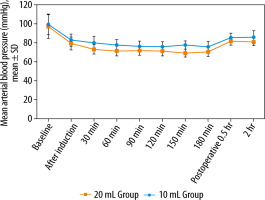
Compared to the preoperative baseline values, all readings of the intraoperative MAP (after induction of anesthesia, 30, 60, 90, 120, 150 and 180 minutes) and the first two hours postoperative readings showed statistically significant decrease (P < 0.001). Also, MAP at all time measurements was significantly higher in 10 mL Group, except for the preoperative baseline values (Figure 3).
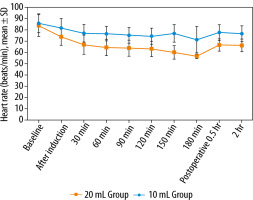
All readings of the intraoperative HR, and the first two hours postoperative readings showed statistically significant decrease compared to the preoperative baseline values (P < 0.001). Also, HR at all time measurements was significantly higher in 10 mL Group compared to 20 mL Group (P < 0.05) except for the preoperative baseline values (Figure 4).
The two groups were comparable regarding the PONV incidence: 2/40 (5%) in the 10 mL Group and 3/40 (7.5%) in the 20 mL Group. None of our patients suffered from local anaesthetic toxicity, hematoma formation, or lower limb motor weakness according to the extended modified Bromage scale.
DISCUSSION
The principal findings of this study are that using 40 mL of 0.25% bupivacaine (20 mL on each side) for bilateral ultrasound-guided mTLIP block in patients having lumbar spine procedures increased the time to and decreased the need for rescue analgesia as well as reduced the need for intraoperative fentanyl, and the postoperative NRS compared to the 10 mL of 0.25% bupivacaine group.
TLIP is a regional anaesthesia technique that targets the dorsal rami of the thoracolumbar nerves as they pass through the paraspinal musculature. It represents the sensory component of the dorsal rami of the thoracolumbar nerves. The classic approach, as described by Hand et al. [4] in a volunteer- based study, involves local anaesthesia injection between the multifidus muscle and longissimus muscles at the level of the third lumbar vertebra (L3) with needle orientation from lateral-to-medial at an approximate angle of 30° to the skin under ultra-sound visualization.
The mTLIP block involves injecting local anaes-thetic between the iliocostalis and longissimus muscles at the targeted lumbar vertebral level with a needle angled at 15° from medial to lateral to improve the sonographic visualisation and blocking the dorsal rami of thoracolumbar nerves at two levels, caudal and cranial, to the injection site. Additionally, by avoiding accidental neuraxial injection, the medial-to-lateral needle advancement improves the safety profile of this procedure in comparison to the conventional method [5].
The area of sensory analgesia with TLIP block has been demarcated by Hand et al. [4] using 0.2% ropivacaine 20 mL on each side (40 mL in total). Five minutes after block application, the participants experienced a loss of pinprick sensation area in lower back of 137.4 ± 71.0 cm2. After 20 min, the area increased to 217.0 mean ± SD 84.7 cm2 with cephalic spread from the injection site was 6.5 mean ± SD 1.8 cm and caudal spread of 3.9 mean ± SD 1.2 cm.
The effectiveness of mTLIP as an analgesic has only been the subject of a small number of studies. Although 20 mL of local anaesthetic solution was employed in the majority of published papers, there is still a dearth of evidence-based recommendations for the ideal volume, concentration, and kind of local anaesthetic for mTLIP analgesia. It would logically follow that a larger volume would allow for a considerably wider spread in the interfascial plane and that a denser block would result from a higher local anaesthetic concentration. While potentially reducing the risk of local anaesthetic toxicity, our study shows that 10 mL of 0.25% bupivacaine was not equivalent to the use of a greater dose of local anaesthetic. The insertion of local anaesthesia in the thoracolumbar interfascial plane between the paraspinal muscles prevents it from being washed away, which is another benefit of the anatomical structure that supported the use of a modest volume of local anaesthesia in the mTLIP block [6–10].
Ahiskalioglu et al. [6] compared the effectiveness of a 20 mL 0.25% bupivacaine injection in a mTLIP block to conventional opioids in patients undergoing spinal surgery and showed that TLIP block can be a crucial part of multimodal analgesia for two- or three-level lumbar spinal surgery. Patients used less intraoperative and postoperative opioids while reporting better pain scores and fewer side effects 24 hours after the procedure.
Li et al. [7] reported two cases of multi-level lumbar spinal surgery performing bilateral mTLIP block at the level of L3 with injecting 0.375% ropivacaine 40 mL (20 mL injected into each side). The block was conducted prior to surgery and revealed loss to pinprick over the posterior lumbar from the left to the right midaxillary lines and from the L1 to L5 spinous processes. They demonstrated that the mTLIP block can relieve the rest pain at 48 hr and the movement pain at 24 hr postoperatively.
Similarly, Ekinci et al. [9] reported a case of lumbar spinal fusion surgery at three levels (L1–L4 vertebral levels). A mTLIP block was performed, after general anaesthesia induction, by injecting 20 mL of 0.25% bupivacaine on each side (totalling 40 mL) at the level of the L3 vertebrae. The maximum visual analogue scale that the patient experienced was three at rest, and he achieved mobilisation within 24 hours. The patient was mobilised very easily, and no additional analgesic was administered during the postoperative period.
Ciftci et al. [10] compared 20 mL 0.25% bupivacaine injection in mTLIP and erector spinae block (ESPB) to opioid analgesia groups in simple discectomy surgeries demonstrating that both blocks provide adequate analgesia compared to opioid group while the was no significant difference concerning intra- and postoperative opioid consumption and post-operative pain score between the ESPB and the mTLIP group with median (minimum–maximum) postoperative total fentanyl consumption was 20.0 (0–140) μg, 20.0 (0–140) μg, and 140.0 (80.0–160.0) μg in the ESPB, mTLIP, and the control groups, respectively with significant difference between the groups (P < 0.001).
Diffuse cutaneous, paravertebral, or epidural dissemination of local anaesthesia are outcomes of ESPB, which targets the ventral and dorsal rami of the spinal neurons. In contrast, TLIP provides targeted dermatomal coverage by focusing primarily on the dorsal rami of the spinal nerve, which are the nerves of interest in lumbar spine surgery [11]. In addition, some reports indicate that local anaesthesia extended to the lumbar plexus in patients with lumbar ESPB, causing weakness in the lower limbs [12]. Also, ESPB injects local anaesthetic into a deeper site. Therefore, the treatment for complications, such as hematoma after alternative nerve blocks, may be delayed. In our study, no complications of TLIP blocking were reported.
The mTLIP block has also been reported as an effective management method for chronic back pain by injecting 0.25% bupivacaine and 40 mL of methylprednisolone into each side at the level of the L3 vertebrae [13].
Ohgoshi et al. [14] presented two cases of multi-level lumbar laminectomy performed using the classical approach of a TLIP block at the level of L3 after general anaesthesia induction. The TLIP blocks were administered bilaterally by injection of 0.375% ropivacaine, 20 mL into each side (total volume of 40 mL). With ultrasound visualization, the local anaesthesia spread was observed to be at the level of L1 to L5 in the injected plane.
Kumar et al. [15] presented a case report of TLIP block after a single level of lumbar discectomy at L3–L4. The block was administered following the induction of general anesthesia, with no additional intraoperative analgesic needs. The first request for an analgesic dose was after 5 hours postoperatively.
Ammar et al. [16] investigated the TLIP block technique with a 20 mL mixture of 10 mL 0.25% bupivacaine and 10 mL 1% lidocaine on each side compared to an opioid analgesia group after a single level of lumbar discectomy. They demonstrated that TLIP block is an effective and safe method for postoperative analgesia through a reduction in the postoperative pain score both on rest and movement and lower cumulative morphine consumption than the control group (9.7 ± 6.38 vs. 25.88 ± 5.17 mg, P < 0.001).
Chen et al. [17] investigated the injection of 30 mL of 0.375% ropivacaine in a TLIP block in patients undergoing lumbosacral spinal fusion surgery. The consumption of opioids in the first 48 postoperative hours has decreased, and the number of effective patients controlling analgesia compressions in the TLIP group was significantly lower than that in the control group. As a result, perioperative pain scores were reduced and patient satisfaction improved, enabling patients to both get out of bed and be discharged earlier.
Hu et al. [18] performed a meta-analysis pooling all the data published in nine randomized-controlled trials, including 618 patients, examining the efficacy of TLIP following lumbar spine surgery. They provided evidence that the TLIP block can effectively reduce postoperative pain and lower patient analgesic consumption when compared to the control group. On the other hand, they demonstrated a significant heterogeneity in VAS scores at 24 hours postoperatively during rest and movement among nine randomized controlled studies. This may be relayed to the use of different local anaesthetics with different half-lives, leading to different effects on pain scores at various times. As a result, selecting the best anaesthetic type, dose, and concentration is critical for postoperative pain relief.
LIMITATIONS
This study has some limitations; the study included patients who had undergone heterogenous operations (canal stenosis, discectomy, fixation, and fractures) which may not generate comparable intensity of intra- and postoperative pain intensity. Patients with fractures were operated on during a scheduled, elective, surgery and were not treated with opioids preoperatively.
Another limitation is the fact that the block was performed after general anaesthesia induction, thus the authors could not perform dermatomal sensory testing. Future studies are recommended to investigate the analgesic efficacy of different concentrations and volumes as well as varying types of local anaesthetics or mixtures for mTLIP. Future studies are also recommended using radiologic and cadaveric techniques to demonstrate the extent of spread under different volumes of local anaesthesia.
CONCLUSIONS
Bilateral mTLIP block using 40 mL of 0.25 % bupivacaine (20 mL on each side) increased the postoperative total analgesia duration for lumbar spine surgeries, and was associated with lower postoperative pain scores compared to 20 mL of 0.25% bupivacaine (10 mL on each side). Moreover, this study demonstrated that mTLIP is a safe and effective technique in different lumbar spine surgeries (single and multi-ple levels of discectomy, lumbar canal stenosis, and lumbar fixation).