Purpose
Brachytherapy (BT, interventional radiotherapy – IRT) is a kind of radiation therapy, in which the radioactive source is placed nearby or even inside the cancer itself; BT may be used alone or in combination with other therapeutic strategies such as external beam radiation therapy, surgery, or chemotherapy. It may represent a valid alternative to surgery in some circumstances [1] or a necessary complementary step to surgery in other situations [2], therefore it plays a pivotal role in several anatomical areas, or in specific patients who may benefit from the method in a balance between risks and benefits, such as elderly or frail patients [3,4].
Even though this kind of radiation therapy appears effective and valuable, BT has been facing a slow but progressive decline over the past decades in Italy and Europe. However, as experts in the field have highlighted, there are many signs of a renewed interest in BT thanks to new technologies. Even though no European data are available to indicate how much the number of centers offering brachytherapy has fallen, we may have an idea looking at the US National Cancer Database, which showed a decline in the proportion of patients treated with brachytherapy from 62.9% in 2004 to 51.3% in 2012 [5].
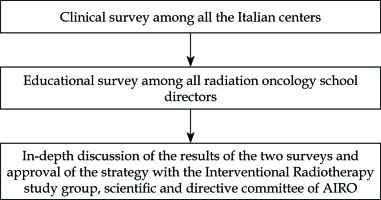
The actions supporting BT of the Italian Association Radiotherapy and Clinical Oncology (AIRO) study group on Interventional Radiotherapy are included in the Trilogy project workflow.
To identify the practical and theoretical reasons why BT has faced a slow decline in Italy, a programmatic path divided into three steps like a trilogy was launched. The workflow of our approach is presented in Figure 1.
Steps 1: Survey on clinical “state of the art” in Italy
The Interventional Radiotherapy (Brachytherapy and Intraoperative Radiotherapy) study group of the AIRO conducted a clinical survey among all the Italian centers in order to analyze the use of BT in clinical practice.
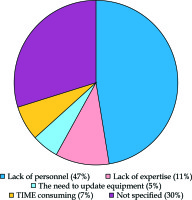
In this first paper, a total of 66 questionnaires were obtained (33.5% of all brachytherapy centers in Italy), out of which 48 (74%) from non-academic hospitals, 6 (10%) from academic hospitals, and 12 (16%) from private institutions. Most centers (84%) had only one brachytherapy machine, and 44% did not deliver brachytherapy treatments or delivered less than demanded due the reasons listed in Figure 2 [6].
Steps 2: Survey on educational “state of the art” in Italy
Then, the study group in collaboration with the Gemelli INTErventional Radiotherapy ACtive Teaching School (Gemelli – INTERACTS – Fondazione Policlinico Universitario “A. Gemelli” IRCCS, Università Cattolica del Sacro Cuore), implemented a specific survey aimed at all radiation oncology school directors in Italy to define the main educational training priorities related to BT.
In this second paper, a total of 23 school directors answered the survey. The results evidenced a wide heterogeneity in the learning activities available to trainees in BT across the country. While theoretical knowledge is adequately and homogeneously transmitted to trainees, the types of practice to which they are exposed varies significantly among different schools as reported in Table 1 [7]. Analyzing the different kinds of BT procedures/sites treated, three major groups can be identified according to the survey results:
Available and important for residential training (gynecologic, skin, anus, breast, esophagus, eye).
Important, but not sufficiently available (prostate, sarcoma, head and neck).
Apparently less relevant for residential training (lung, BT in children, and rectal).
Table 1
Brachytherapy (BT) procedures in radiotherapy school. Modified from reference [7]
Step 3: Discussion and strategy identification
The third step implied the discussion of the results obtained by the two surveys within the study group, with the definition of a possible strategy to overcome the identified problems. The “Task Force” for the in-depth discussion was composed of 12 people: chair (LT), elected chair (AV), past chair (CA), deputy chairs (CV, VDS), secretary (VL), and board members (FB, VF) of the AIRO Interventional Radiotherapy study group; a member of GIOGER (Italian Group of Geriatric Oncology) (GC), the chair of the scientific commission of the AIRO (RC), the AIRO president (SMM), and member of AIRO committee (MAG).
AIRO Interventional Radiotherapy study group “state of the art” analysis
There is a considerable amount of literature covering the topic of the role of BT in clinical practice; BT can be indicated in exclusive, adjuvant, perioperative setting, but also to deliver a boost. In particular, there is evidence, which has proven that in selected cancers, such as cervical and prostate cancer, BT boost vs. no boost increases overall survival after external beam radiation therapy [8,9,10]. Moreover, there is evidence that the use of intensity modulated or stereotactic radiation therapy as alternatives to BT boost resulted in worse results not only in terms of overall survival, but also with regards to aesthetic results, and function and organ preservation [11,12,13,14]. It is worth to mention that BT plays an important role in treating elderly patients, particularly unfit, frail, or sarcopenic, in which a conservative therapeutic approach may be the best choice [15].
Analyzing the international scenario in terms of cultural background, it becomes clear that there is an adequate attention and consideration towards BT, supported by the presence of dedicated guidelines, with regard to several anatomical sites issued by the main European [16,17,18,19,20,21,22,23,24,25] and American societies [26,27,28]. For this reason, it is sensible to correlate the cultural diffusion of the role and importance of BT at a national level, with its actual diffusion in the clinical practice [29,30,31,32,33,34,35,36,37,38]. In our view, scientific national associations are called to a difficult, but at the same time, fundamental role in supporting and fostering the process of re-discovery of BT through a proper and dedicated vision.
Vision of AIRO Interventional Radiotherapy study group
After having analyzed and discussed the results of the AIRO Interventional Radiotherapy study group surveys, we shared a vision about the emerged issues, so the following strategy was adopted.
Four relevant domains were identified (Table 2):
Table 2
Domains, issues, and relative solutions (accomplished or in progress) proposed according to the defined strategy
Clinical practice
First of all, the working group has fostered the inclusion of BT as a treatment option when clinically indicated, in the frame of national guidelines such as other study groups [39]. To facilitate such goal, representatives of the Interventional Radiotherapy study group were included both in the committee for the discussion of national guidelines and in other AIRO study groups (especially the ones dealing with gynecology, breast, and prostate cancer). Moreover, the members of the study group have been included in the AGENAS (National Agency for Regional Sanitary Services) working group for National Protocols (PDTA, Pathway Diagnostic Therapeutic Assistential).
In the near future, it will be fundamental to include BT within the interdisciplinary guidelines, taking into particular consideration not only cancer patients, but patients who could benefit from these treatments such as frail elderly [40]. For this reason, it has become important to develop synergies with other scientific societies such as GIOGER, SIGG (Italian Society of Geriatrics and Gerontology), and SIOG (International Society of Geriatric Oncology).
A series of systematic reviews and scientific papers were written under the auspices of the AIRO study group and, at the moment, some of them have already been published, whereas others have been submitted [41].
A very interesting point, when considering the potential indications of BT across the different American and European guidelines, is to focus on the level of evidence available.
In fact, for a large number of sites (including prostate, cervix, endometrium, breast, uvea, esophagus), the indications that can be found in the guidelines are actually based on randomized controlled trials (Table 3) [42].
Table 3
Type of study supporting brachytherapy
Education
Another key point that emerged from our surveys is the need for an improvement of interventional radiotherapy education in Italy, especially to better define and harmonize programs at national level, particularly in practical teaching. For this reason, AIRO supported attendance in experienced centers or national and international courses on specific aspects of BT in order to facilitate the achievement of a satisfying level of BT knowledge among radiation oncologists. Moreover, AIRO endorsed University post-specialty courses (‘second level’ Masters) to allow professionals (already certified in radiation oncology) to acquire more complex BT knowledge. This will facilitate the recruitment of skilled professionals for hospitals’ BT units [43,44].
Research
The role of research in the field of interventional radiotherapy faces the same problems, highlighted in the clinical and educational settings. In fact, one of the greatest issues is the paucity of data due to the relatively small number of patients included in randomized clinical trials. As a possible solution to this problem, there has been a huge effort in creating a national and international network for dedicated research and big data sharing. The study group has thus supported the COBRA (COnsortium for BRachytherapy data Analysis) project born in the framework of the GEC-ESTRO for a wide national research database [45,46,47,48].
Communication
Finally, we believe that difficulties of communication with other specialists, with patients, and also institutional representatives regarding the present modality of the procedures, may represent a further obstacle. Active support to a more accurate knowledge of BT among colleagues and patients should be pursued. However, the ability to address the first three aspects (clinical practice, education, and research) may facilitate a better and more effective communication, especially with the specialists from other oncology branches. A task force was created within the study group for the development of patient specific booklets both paper- and web-based. The term “interventional radiotherapy” was introduced in the name of the study group.
Changing the name allows several advantages, leading to better communication with colleagues and patients because it better explains the effective operational aspects of the technique. According to our view, it results also in better communication with the national institutional representatives, with a consequent smoother procedural and organizational crosstalk, resulting also in a more adequate reimbursement.
Conclusions
Modern interventional radiotherapy can be considered an important tool for the management of cancer patients to be integrated with other therapeutic strategies. The AIRO vision implies that specific strategic interventions must be other specialties in an interdisciplinary setting. We deeply believe that brachytherapy (interventional radiotherapy) is increasingly being considered and in the coming years, we expect more pronounced results.