Dear Editor,
According to CDC data, chronic pain affects 50 million Americans, or 20% of the national population, causing significant and prolonged morbidity. Chronic low back and neck pain carry an estimated healthcare spending cost of 67.5 to 94.1 billion USD annually, the third highest in the US after ischaemic heart disease and diabetes [1]. While some patients may require surgical intervention, it is estimated that between 10% and 40% will continue to experience persistent pain after back surgery, a syndrome called failed back surgery syndrome (FBSS) or post laminectomy syndrome (PLS). With a constantly increasing number of spinal surgeries (e.g. 220% increase in spinal fusion surgery between 1990 and 2000), these number are expected to remain significant [2]. The aetiology of PLS varies and includes patient, operative, and post-operative factors; it includes persistent pain due to inability to achieve the aim of surgery or operating on an incorrect level, persistent radicular pain from long-term nerve root injury, re-stenosis of neuroforamen or central canal, facet disease, and pain from surgical scar [3]. The complex aetiology and comorbidities of PLS make it challenging to treat; management usually includes medical optimization and psychosocial intervention, but usually requires neuromodulation, with options including spinal cord stimulation (SCS), peripheral nerve field stimulation, and dorsal root ganglion stimulation; however, the data from these methods are still lacking and the efficacy is anecdotal [4].
Implanted intrathecal drug delivery systems (IDDS) are an effective modality in the management of chronic pain symptoms related to spasticity and terminal cancer. Intrathecal therapy emerged in the 1970s to address chronic malignant pain after the efficacy of intrathecal morphine was shown in cancer patients. Since 1984, it has also been used for severe spasticity, including for multiple sclerosis, spinal cord injury, cerebral palsy, and post-stroke [5]. More recently, IDDS have been used for refractory non-cancer pain syndromes with varying degrees of success; importantly, IDDS also provide a treatment modality that reduces consumption of systemic opioids, an important factor considering the constantly increasing prevalence of opioid addiction and the overall trend to avoid and reduce opioid treatment for chronic pain [6]. Increasing evidence has emerged supporting the use of IDDS in PLS as a safe and effective therapy [7]. While generally safe and effective in these applications, granuloma formation and persistent cerebrospinal fluid (CSF) leak following implantation, catheter exchange, or intrathecal pump revision are known and significant complications of intrathecal pump catheter management [8].
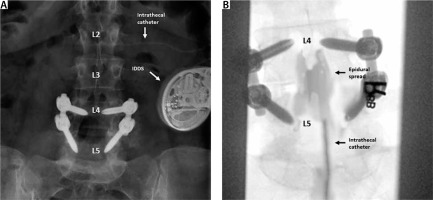
FIGURE 1
Caudal instillation of epidural blood patch for post-laminectomy syndrome. Intra-operative fluoroscopy images present (A) hardware from previous instrumentation, including L4–L5 fusion, implanted intrathecal drug delivery systems and intrathecal catheter, and (B) epidural spread of 15 mL sterile autologous blood following a caudal approach at the L5–S1 level in this patient with previous lumbar spinal instrumentation
Post-dural-puncture headache (PDPH) is a known complication of neuraxial anaesthesia and is classically attributed to accidental dural puncture during epidural anaesthesia. It is most commonly encountered in obstetric anaesthesia with the use of neuraxial anaesthesia in parturients and can result in significant suffering secondary to debilitating pain. A recent study estimated the risk at 0.9% of women undergoing epidural, spinal, or combined spinal-epidural anaesthesia [9]. The incidence of PDPH following IDDS placement is harder to estimate but may be as high as 23% [8]. An epidural blood patch (EBP) is considered the most effective treatment for PDPH [10]. Patients who experience PDPH following IT catheter insertion frequently improve with conservative management. Less invasive measures, such as sphenopalatine ganglion block and bilateral greater occipital block, have also shown promise in the therapy of PDPH. However, in refractory cases escalation of care to EBP or a fibrin glue patch may be warranted.
A 55-year-old male with a history of FBSS secondary to an L4–L5 posterior fusion required treatment of pain secondary to anterolisthesis and severe spinal stenosis at L4–L5. An IDDS was implanted for the administration of intrathecal morphine and treatment of his severe persistent post-operative pain. IT catheter positioning and pump implantation were performed without complication. On the fourth post-operative day, the patient presented with symptoms characteristic of PDPH including positional headache, neck pain, and nausea. A trial of conservative management, which included bedrest, over the counter analgesics, and hydration, failed after three days. Other conservative methods, including trans-nasal sphenopalatine ganglion block and bilateral greater occipital nerve block, were considered but not attempted in this case due to the severity of the patient’s headache. Therefore, it was decided to proceed with an EBP. Given the patient’s history of lumbar surgery and instrumentation, a caudal approach was elected. The caudal epidural space was accessed using a loss of resistance technique at the level of the sacral hiatus without complication; penetration of the epidural space was achieved 1cm after ligament engagement. An epidural catheter was threaded to the L5–S1 disc space, and 15 mL of autologous blood, drawn in a sterile fashion, was slowly administered into the epidural space via the catheter. Blood was administered in small aliquots, until the patient experienced consistent discomfort.
The patient tolerated this procedure well and recovered as expected. Following the procedure, the patient reported complete resolution of PDPH symptoms without reoccurrence upon subsequent follow-up.
Chronic back pain is associated with significant morbidity and financial toxicity, on both the individual and societal level. The number of spinal procedures has been increasing steadily; however, a significant proportion of patients will continue to endorse pain after surgery and will be diagnosed with PLS. In this population, despite increased risk from previous lumbar instrumentation, IDDS can be a safe and effective treatment modality. Furthermore, with increased emphasis on reduced overall opioid consumption, patients with FBSS may be increasingly considered for IDDS. While lumbar EBP is effective for treatment of PDPH, prior surgical manipulation and instrumentation precludes a lumbar approach for minimally invasive treatment of commonly occurring PDPH symptoms following IT catheter placement. In patients with FBSS, who suffer from PDPH recalcitrant to conservative measures, a caudal approach for EBP may be a safe intervention.




