Introduction
Diabetes mellitus is a disorder of metabolism governed by various etiological factors, characterized by prolonged hyperglycemia due to a defect in the production or action of insulin or both [1]. Type 1 diabetes mellitus (TIDM) occurs when the body fails to secrete functional insulin [2, 3]. Type 2 diabetes mellitus (T2DM) is a result of insulin resistance [2]. Mutations of PPARγ on chromosome 3, ABCC8 and KCNJ11 genes on chromosome 11, and the CALPN10 gene on chromosome 2 have been shown to increase the risk [4, 5]. In 2015, diabetes caused the deaths of about 5 million adults. India has the second highest number of children suffering from TIDM [6].
Cervical cancer is the fifth commonest cancer in humans and second on the list of common cancers in women worldwide. It has proven to be a type of cancer that frequently attacks women in India and is the most frequent cancer-causing mortality in developing nations. In India, about 365.71 million women aged over 15 years are more vulnerable to cervical carcinoma. Risk factors may include immunodeficiency diseases, herpes, smoking, and oral contraceptives. Unlike other cancers, cervical cancer manifests early, with incidence rising in the age group of 30–34 years and peaking at 55–65 years, with a median age (age 21–67 years) of 38 years [7–9]. Studies suggest that UBE2C, CCNB1, CCNB2, NIP210, MELK, CDC20, etc. genes were overexpressed in tumors. There is no tangible evidence regarding the genetic relationship between diabetes mellitus and patients suffering from carcinoma of the cervix.
As per a combined consensus report drafted by the experts from the American Diabetes Society and the American Cancer Society to re-explore the link between the incidence of malignancies and diabetes, common risk factors, biochemical links, and correlation between treatment of diabetes and the risk of malignancies, it was found that T2DM may aggravate the risk of certain malignancies (hepatic, pancreatic, and endometrial). However, there was no conclusive evidence to associate cervical carcinoma with T2DM. This relationship was likely extrapolated as a result of having similar risk factors. The risk factors were categorized as non-reversible (age, sex) and reversible (diet, physical activity, alcohol, smoking). The biochemical link associated with it involved hyperglycemia, hyperinsulinemia with activation of the IGF-1 axis, and inflammation, with previous literature suggesting that metformin may be associated with a lower risk of cancer while exogenous insulin may be associated with a higher risk [10]. A cross- sectional population-based study was conducted by the Epidemiological Department of Mexico to determine the prevalence and risk of cervical carcinoma in T2DM patients. They took 160 cases of cervical carcinoma and 25,262 controls and concluded that the prevalence of cervical carcinoma in females with T2DM is significantly higher than in non-diabetic females (1,336 vs. 576 subjects per 100,000 inhabitants, p < 0.001). The study postulated that in the cervical cancer cells of diabetic patients, the pathway involved is the LKB1-AMPK-mTOR signaling pathway, which senses and responds to nutrient availability, energy efficiency, stress, hormones, and mitogens that govern protein synthesis. This suggests the critical role of this cascade in the progression of cancer and diabetes [11]. A study explored the relationship between usage of metformin and the risk of cervical carcinoma in T2DM. Conducted by the Nation Taiwan University of Medicine, this was one of the first cohort studies to report that metformin use may reduce the risk of cervical cancer as opposed to patients taking alternative hypoglycemic agents. This finding was presumed to be due to the anti-inflammatory action of metformin or the inhibition of pro-inflammatory pathways such as the nuclear factor-ĸB and signal transducer and activator of transcription 3 (STAT3) pathways. Also, it was reported that metformin restricts malignant cell growth in the cervix through AMPK-independent activation [12]. A meta-analysis including 11 studies and a systematic review was conducted to find the predictive value of diabetes and the prognosis of cervical carcinoma. A total of 11,091 patients were reviewed, and the study suggested that patients with T2DM had poor overall survival and recurrence-free survival. This establishes that T2DM is a key prognostic factor in patients with carcinoma of the cervix. The subgroup analysis revealed that diabetes had an independent relationship with shorter overall survival. The ease of diagnosis of T2DM makes it a well-suited indicator for assessing the prognosis of cervical cancer [13].
Although many studies have shown a correlation between the prognosis of cervical carcinoma and diabetes mellitus, the literature lacks information about the vulnerability of women with T2DM to cervical carcinoma. Therefore, this study was performed to evaluate the potential association between cervical cancer and T2DM among women.
Material and methods
The current hospital-based case control study was conducted at hospitals attached to Kasturba Medical College, Mangalore, MAHE, Manipal, Karnataka, India, for a period of about three months. Mangalore is a city in Karnataka, India, well known for its excellent medical infrastructure. As per the 2001 census, the city has an excellent literacy rate of about 82.2%, which includes a high female literacy rate as well. Clearance was obtained from the Institutional Ethics Committee for the study. Women diagnosed with carcinoma of the cervix (using standard methods) and admitted to the study hospital during the study period were considered. Diagnosis of diabetes was made or verified via standard procedures. Total numbers of cases and controls were 60 each, giving a total sample size of 120. Convenient sampling was used until the sample size was reached. A structured questionnaire was created, validated and used. It included the subject’s awareness about cancers and diabetes. Socio-demographic details of the participants were collected. Patients not willing to participate were excluded from the study. Patients with cervical carcinoma with or without diabetes were assigned to two groups based on attainment of menopause (women ≥ 60 years, no history of menstruation without drugs > 1 year, follicle stimulating hormone and estradiol level are in post-menopausal range) [11, 12].
Data were analyzed using SPSS version 11.5. Results were expressed as proportions using appropriate tables and graphs. Odds ratios were calculated, and the χ2 test was used. P-values ≤ 0.05 were considered statistically significant.
Results
Table 1 shows that the median age of patients in cases and controls was 57.50. Among the cases, most patients had had cervical carcinoma for 2 years or more. The most common blood group among cases was O positive and among controls A positive. Among cases, most women (40%) had a high parity score greater than P3L3, with P4L4 being most common and P10L9 being the highest. The stage of the disease was mostly higher than stage IIb, with stage IIIb being most common. The most common histological type was large cell non-keratinizing squamous cell carcinoma (LCNKSCC) (36%), followed by moderately differentiated squamous cell carcinoma (MDSCC) (27%). Diabetic patients in both case and control groups mostly took metformin for treatment, followed by insulin therapy.
Table 1
Demographic details of patients (N = 60)
Cervical carcinoma
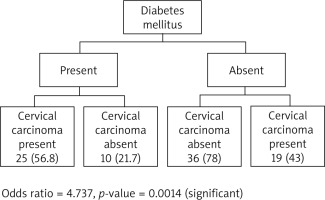
Figure 1 shows the association of diabetes in post-menopausal women with cervical cancer and patients without cervical cancer. The p-value is 0.0014, which is statistically significant.
Cervical carcinoma
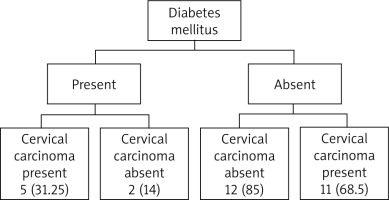
Figure 2 shows the association of diabetes in pre- menopausal women with cervical carcinoma and patients without cervical carcinoma. The results were not statistically significant.
Table 2 shows a univariate analysis to test for the risk factors of diabetes mellitus in patients with cervical carcinoma among the pre- and post-menopausal groups. The risk factors considered were hypertension, increased body mass index (BMI) and anemia. All of the above results were statistically non-significant.
Table 2
Univariate analysis showing risk factors for diabetes mellitus in patients with Cervical cancer
Table 3 shows the co-morbidities in the case and control groups. The cases most commonly had respiratory illnesses while controls mostly had other cancers.
Table 3
Co-morbidities in cases and controls
Discussion
The study analyzed the correlation between cervical carcinoma and DM among females in Mangalore. It was conducted on 60 cervical cancer cases and 60 equally age-matched controls. The mean age of both cases and controls was 56.50 ±11.3 years. It was found that 29% of the patients were sixty to seventy years old, implying that this age group is at a prospective risk of carcinoma of the cervix in India. This is consistent with the findings of West, as published in the British Journal of Cancer [14]. Another study conducted by White et al. revealed that the risk for cervical cancer does not decline until 85 years, and hence screening must be done between the ages of 21 and 85 [15].
In our study, it was observed that about 40% of the females with cervical carcinoma were multiparous. This is consistent with a number of studies. It was first reported by Eluf-Neto et al. in 1994 [16]. The relative risk of carcinoma of the cervix amongst women with a parity of ≥ 5 is in the range 3.8–4.4 [17, 18]. Another study in Finland reported that the rise in frequency of carcinoma of the cervix among multiparous women was mostly seen below 50 years. It also took into consideration the age at first birth and the interval between births [19]. The reason for this finding may be the increased metaplastic response of squamous epithelial cells during pregnancy, which predisposes the cervical epithelium to malignant transformation. Our study also revealed that amongst cases, the most conventional histological sub-type is poorly differentiated LCNKSCC/SCC (36%), followed by moderately differentiated SCC (27%). Kuo et al. reported that in patients with DM, SCC is common, which is consistent with our study [20].
A study conducted by Tseng in 2016 evaluated the function of metformin in reducing the risk of carcinoma of the cervix. It was hypothesized that metformin attenuates inflammation by correcting metabolic derangements, arrests pro-inflammatory pathways such as the STAT3 pathway, and generally impedes the proliferation of cervical cancer cells through AMPK activation [13]. In our study, case and control subjects primarily took metformin as anti-diabetic medication; therefore, we cannot draw any conclusions about reduced risk. Research performed by López-Hernández revealed that the relationship between diabetes mellitus and cervical carcinoma was substantial (p < 0.001) and the risk was twice as high [11]. This is in accordance with our study, but in the post-menopausal women, we observed that the association of diabetes with cervical cancer was statistically significant (p = 0.0014), with the relative risk being twice as high (OR = 4.737, p = 0.0014). Similar results have also been reported by other researchers [21–24]. Furthermore, O’Mara et al. reported analogous findings of diabetes as a risk factor in the development of vaginal and uterine cancer [20]. But the same results are incongruent with the findings in pre-menopausal women, where the association was not statistically significant (p = 0.5071).
The reason for the correlation between DM and cervical carcinoma lies in the molecular mechanisms governing intracellular signaling. Type 2 diabetes mellitus is characterized by hyperglycemia along with insulin endurance and a simultaneous increase in cytokine production. This, coupled with other risk factors such as obesity and tobacco smoking, is said to alter the reliability of the LKB1-AMPK-mTOR signaling route, which serves as a step in the malignant transformation of cervical epithelial cells. A study by Kuo et al. revealed that an increase in IGF-1R expression leads to several cancers, including cervical, liver, and breast [25–27]. Cervical cancer develops due to an interaction between environmental factors such as infection by the human papillomavirus [16, 18] and genetic factors. The human papillomavirus affects the metaplastic region of the squamo-columnar junction between the endo-cervix and the ecto-cervix. This metaplasia may be triggered by chronic inflammation due to diabetes mellitus. Also, the above study provides evidence of the involvement of HLA class II haplotypes in the progression of carcinoma of the cervix. These genes may, furthermore, be influenced by diabetes. Hence, diabetes affects the environment and genetic factors, which lead to the development of carcinoma of the cervix.
In our study, the average weight and BMI as calculated for 116 patients showed similar distribution in case and control groups (60 cases: weight 50.05 ±11 kg and BMI 22.15 ±5). This corresponds to the results of the study conducted by other researchers [11]. In the univariate analysis, our study revealed that BMI was not a significant risk factor for cervical malignancy among diabetics in pre- and post-menopausal age groups, with p = 0.27719. This is in accordance with a study by Jiamset et al. in 2016, as it reported similar conclusions (p = 0.278). The above study also highlighted that the correlation between T2DM and five years without relapse plus overall existence of cervical cancer (p = 0.008) was significant [25]. This proves that T2DM in cervical carcinoma is a useful prognostic indicator, as similar results have been reported by other studies [26]. In our study, we performed a univariate analysis to determine whether hypertension and anemia were individual risk factors for diabetes in patients with cervical carcinoma. Both of the above associations were statistically non-significant, with p = 0.2187735. These associations have not been considered in previous studies.
The major strengths of the study lie in the equal numbers of age-matched cases and controls and the consideration of hypertension and anemia as risk factors. The association between diabetes and other cancers such as uterine, liver, and breast cancer has been studied previously, but its relation to cervical cancer is a fairly new discovery. However, this study is limited by its small sample size and limited information regarding lifestyle, physical activity, tobacco smoking, and alcohol consumption. Another confounding factor was the co-morbidities associated with the age of the patients.
Conclusions
This article highlights a remarkable association concerning diabetes mellitus and cervical carcinoma among females who have attained menopause. This illustrates that diabetes is one of the risk factors for cervical carcinoma and could contribute to its poor prognosis [28, 29]. India is a diabetic hub of the world and cervical cancer is known as a major cause of mortality in women, with more than a quarter of its global burden coming from developing countries [30]. Hence, diabetic females after attaining menopause have a greater risk of developing cervical carcinoma and therefore mandatorily should be screened routinely for early diagnosis, treatment and better prognosis. Future research with a longer timeframe is needed in order to generalize the results.
This study was limited by the fact that it was for a short duration and was tested on a relatively small sample.