Simultaneous esophageal resection and pulmonary lobectomy for synchronous esophageal cancer and lung cancer is associated with an increased risk of postoperative complications, including esophageal leakage and broncho-pleural fistula [1]. Endoluminal vacuum therapy (EVT) has been reported to be effective in the treatment of anastomotic leak after esophageal resection [2]. However, in the event of a bronchial fistula, EVT may cause significant air leakage through the fistulas, which may eventually lead to respiratory complications and impede negative pressure treatment. Here we present a patient with bronchopleural and esophagopleural fistula successfully treated with surgery and EVT.
A 69-year-old man was referred for the treatment of a tumor in the right lung and concomitant esophageal diverticulum. His medical history revealed arterial hypertension, peripheral arterial disease, myocardial infarction and coronary artery bypass grafting.
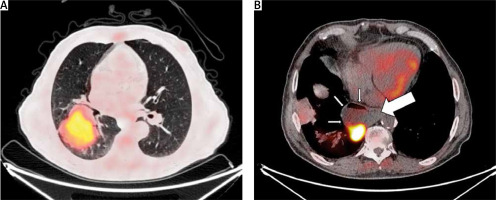
Positron emission tomography–computed tomography (PET-CT) using 18F-FDG revealed a 10.7 × 8.0-cm tumor with a standardized uptake value (SUV) of 9.3 in the lower and middle lobes of the right lung (Figure 1 A), diverticulum of the lower esophagus, which contained a 3.9 × 2.9-cm lesion with an SUV of 23.2 (Figure 1 B), and thickening of the stomach wall with a SUV of 3.3 suspected of gastritis. Fiberoptic bronchoscopy showed a tumor in the right lower lobe bronchus, and biopsy established the diagnosis of adenocarcinoma. Esophageal diverticulum with ulcerated lesion was visualized in esophagogastroscopy at 35 cm from the tooth line. Biopsy of the esophageal tumor revealed dysplasia and biopsy of the stomach showed chronic active inflammation. No other abnormalities were found using pulmonary function tests, electrocardiography and echocardiography.
Figure 1
PET-CT: A – lung tumor in the lower and middle lobes of the right lung; B – esophageal tumor within the wall of the esophageal diverticulum (thin arrows), esophagus (thick arrow)
Surgery was performed under general anaesthesia. The postero-lateral thoracotomy approach was used, and right lower bilobectomy, resection of esophageal diverticulum and systematic lymph node dissection was performed. The lower lobe bronchus and esophageal diverticulum were divided using an endostapler. The postoperative course was initially uneventful. Gastrografin swallow and chest computed tomography on postoperative day (POD) 9 revealed esophageal leakage and gastroscopy showed a 3-cm esophageal fistula at the level of the suture line (Figure 2 A).
Figure 2
Endoluminal vacuum therapy. A – Gastroscopy before EVT: esophageal fistula (arrow), esophageal lumen (asterisk); B – polyurethane foam wrapped around the tip of the nasogastric tube prepared for insertion; C – gastroscopy after EVT: healed fistula (arrow), esophageal lumen (asterisk)
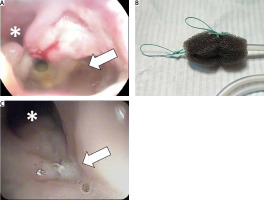
Under gastroscopic control, polyurethane foam (V.A.C., GranuFoam, KCI, San Antonio, TX, USA) wrapped around the tip of the nasogastric tube (Figure 2 B) was introduced into the esophageal fistula and EVT therapy (INFOV.A.C., KCI, San Antonio, TX, USA) with –100 mm Hg pressure was initiated. However, on POD 12 bronchopleural fistula developed with complete dehiscence of the bronchial stump. The patient was reoperated. Laparotomy and re-thoracotomy approaches were used. Gastrostomy and jejunostomy were placed, the bronchial stump was shortened and sutured, and the esophageal fistula was closed with a running suture. Both bronchial and esophageal suture lines were covered with omentum. The bronchopleural fistula healed, but esophageal leakage recurred after 8 days. EVT was reintroduced and continued with the pressure of –100 mm Hg. Sponges were changed every 3–4 days. EVT was stopped after 36 days when there were no signs of fistula in gastroscopy (Figure 2 C) and Gastrografin swallow. Follow-up gastroscopy after a month showed a completely healed esophagus. Final histopathology confirmed a diagnosis of adenocarcinoma of the lung (pT4, N0, M0, R0, stage IIB) and spindle cell (sarcomatoid) esophageal carcinoma (pT3, N0, M0, R0, stage IIA). At a multidisciplinary team meeting, the patient was disqualified from adjuvant treatment. Follow-up PET-CT 12 months after surgery showed no signs of relapse.
EVT is safe and effective for the treatment of fistulas in the esophagus, stomach, small and large intestines [3, 4]. In a recent publication by Schniewind et al., the authors compared EVT, surgery and stenting for the treatment of esophageal leakage after esophagectomy and found that EVT was associated with lower mortality than other methods [5]. However, simultaneous occurrence of both bronchial and esophageal fistula is a much more complex situation. Direct application of negative pressure therapy to the esophageal fistula located near the bronchial fistula can result in significant air leakage from the respiratory tract and respiratory failure, and the ineffectiveness of negative pressure therapy. In such a situation, closure of the bronchial fistula, preferably by suturing the bronchus and omentoplasty is essential. Interposition of the omentum between the sutured bronchus and the esophageal fistula improves bronchial blood supply and prevents recurrence of the bronchopleural fistula, separates the esophagus from the bronchus in the event of recurrence of bronchial stump dehiscence, and is an excellent foundation for the healing of the esophagus with negative pressure therapy [6].
EVT is generally considered a safe procedure. Minor complications have been reported rarely and included sponge dislocation and anastomotic strictures. EVT should be used with caution when the fistula is in proximity to the aorta or the heart because of the increased risk of life-threatening bleeding [7].
Surgery combined with endoluminal vacuum therapy may be effective in the treatment of complex, synchronous bronchopleural and esophageal pleural fistulas.





