Introduction
Computed tomography (CT) scans routinely identify pulmonary nodules (PNs) during lung cancer screenings [1–3]. For PNs with a high risk of malignancy, video-assisted thoracic surgery (VATS) is commonly suggested for comprehensive resection, demonstrating lower morbidity and reduced hospital stay than thoracotomy [4]. However, challenges arise when PNs are diminutive (< 10 mm in diameter) or situated in deep regions > 5 mm from the pleura. In such instances, the lack of precise nodule identification can result in approximately 63% of VATS procedures converting to thoracotomy [5]. Consequently, preoperative localization of PNs becomes critical for guiding precise VATS resections [6, 7].
Numerous localization materials, including hook-wire (HW), coil, radio-label, localization needle, and various liquid materials (LMs), are employed in preoperative PN localization [7–10]. The most commonly used are HW and LMs [11–17]. However, comparisons between the safety, successful localization rate, and postoperative outcomes between HW localization (HWL) and LMs localization (LML) remain inconclusive. Thus, a gap exists for a more detailed meta-analysis focusing on comparative studies to assess the relative safety and efficacy of HWL and LML in VATS-based PN resection.
Aim
This meta-analysis aimed to juxtapose the safety and effectiveness of preoperative CT-guided localization of PNs using HW and LM.
Material and methods
Study selection
This meta-analysis, registered at INPLASY.COM under reference number INPLASY202350082, was executed in compliance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [18].
The PubMed, Web of Science, and Wanfang databases were searched to identify relevant studies published as of March 2023 using the following strategy: “(((hook wire) AND (((((glue) OR (lipiodol)) OR (blood)) OR (indocyanine green)) OR (blue))) AND (nodule)) AND ((lung) OR (pulmonary)).”
The criteria for the inclusion of studies were as follows:
The studies should be comparative in nature.
The studies shoiuld involve patients with PNs.
The interventions under consideration should be preoperative HWL vs. LML.
There were no language restrictions for the studies.
Conversely, studies were excluded based on the following criteria:
Data extraction
Data pertinent to the study were extracted independently by 2 authors from eligible studies. Discrepancies that arose were resolved by consultation with a third author. The baseline data extracted comprised the country, year of publication, first author, patient count, study design, gender ratio, age, PN count, PN-pleura distance, and PN diameter. The outcome data included technical success rates for localization, total complication rate, localization duration, pneumothorax rate, pulmonary haemorrhage rate, duration of VATS, and length of postoperative hospital stay.
Quality assessment
The Cochrane risk-of-bias tool was employed to evaluate the quality of randomized controlled trials (RCTs). This involved assigning a risk of bias (low, high, or unclear), including reporting, selection, detection, attrition, performance, and other forms of bias. The Newcastle-Ottawa scale (NOS) [19] was utilized for non-RCTs. The scale allocated points based on 3 criteria: selection (4 points), exposure (3 points), and comparability (2 points). A study with a NOS score of 7 or higher indicates a high-quality study.
Definitions
Technical success for HWL was defined as the visibility of the HW without dislodgement, whereas for LML, technical success was denoted by the visibility of the LM on the lung surface without diffusion away from the injection site [14]. The duration of localization was defined as the interval between the moment the patient was positioned on the CT bed and the successful insertion of the localization materials [20]. The extent of VATS was operationally defined as the interval between the commencement of the incision and the final closure of the wound [20]. The duration of hospital stay after surgery was defined as the period between the completion of VATS and the discharge of the patient [20].
Statistical analysis
The meta-analysis and associated analyses were executed using RevMan v5.3 and Stata v12.0. Pooled odds ratios (ORs) with 95% confidence intervals (CIs) were calculated for categorical data, while continuous data were evaluated using pooled mean differences (MD) with 95% CIs. Heterogeneity was appraised using the I2 statistic and Q test, with an I2 greater than 50% signifying significant heterogeneity. Random-effect models were employed in cases of significant heterogeneity, whereas fixed-effect models were utilized otherwise. Sensitivity analyses were performed using a “leave one out” approach to identify sources of heterogeneity. Subgroup analyses were conducted using different LMs (methylene blue, indocyanine green, and medical glue). Publication bias was evaluated using Egger’s test, with a significance threshold set at p < 0.05.
Results
Study selection
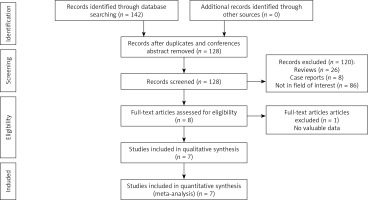
The flowchart of this meta-analysis is shown in Figure 1. A total of 7 studies were included in this meta-analysis from 142 relevant studies. Of the 7 studies, 6 studies were retrospective [11–15, 17], and one study was a prospective non-RCT [16] (Table I). These 7 studies were from several countries, including China, the USA, and Korea. These 7 studies included 551 patients (583 PNs) who had undergone CT-guided HWL and 551 patients (612 PNs) who had undergone LML (Table II). As the LMs, methylene blue [11, 13], indocyanine green [12, 14], medical glue [15, 17], and lipiodol [16] were used by 2, 2, 2, and 1 study, respectively. All 7 studies exhibited NOS scores of 8.
Table I
Baseline data of the included studies
| First author | Year | Country | Design | NOS |
|---|---|---|---|---|
| Chu [11] | 2022 | China | Retrospective | 8 |
| Ding [12] | 2021 | China | Retrospective | 8 |
| Kleedehn [13] | 2016 | USA | Retrospective | 8 |
| Lin [14] | 2022 | China | Retrospective | 8 |
| Pan [15] | 2020 | China | Retrospective | 8 |
| Park [16] | 2020 | Korea | Prospective non-randomized trial | 8 |
| Zhang [17] | 2022 | China | Retrospective | 8 |
Table II
Baseline data of the patients in the included studies
| Author | Groups | Liquid materials | Patients (n) | Age [years] | M/F | Nodules (n) | Nature of nodules (solid/GGN) | Diameter [mm] | Lesion-pleura distant [mm] |
|---|---|---|---|---|---|---|---|---|---|
| Chu [11] | Hook-wire | Methylene blue | 107 | 54 | 43/64 | 135 | Not given | 8 | 9 |
| Liquid | 112 | 54.5 | 41/71 | 151 | Not given | 9 | 10 | ||
| Ding [12] | Hook-wire | Indocyanine green | 92 | 53.1 | 26/66 | 95 | 13/82 | 6.7 | 8.4 |
| Liquid | 65 | 51.3 | 16/49 | 85 | 13/72 | 6.3 | 9.2 | ||
| Kleedehn [13] | Hook-wire | Methylene blue | 52 | 60.3 | 16/36 | 52 | Not given | 10 | 9.2 |
| Liquid | 57 | 62.6 | 25/32 | 57 | Not given | 10.6 | 14.7 | ||
| Lin [14] | Hook-wire | Indocyanine green | 41 | 49.6 | 9/32 | 42 | 4/38 | 7 | 8.8 |
| Liquid | 53 | 48.2 | 12/41 | 55 | 5/50 | 6.8 | 11.1 | ||
| Pan [15] | Hook-wire | Medial glue | 60 | 58.7 | 39/21 | 60 | Not given | 10.3 | 3.8 |
| Liquid | 60 | 55.5 | 35/25 | 60 | Not given | 11.3 | 3 | ||
| Park [16] | Hook-wire | Lipiodol | 125 | 59.6 | 64/61 | 125 | All GGN | 13.8 | 17.2 |
| Liquid | 120 | 60.9 | 50/70 | 120 | All GGN | 15.0 | 19.5 | ||
| Zhang [17] | Hook-wire | Medial glue | 74 | 51 | 38/36 | 74 | Not given | 9.4 | 20.6 |
| Liquid | 84 | 48.9 | 35/49 | 84 | Not given | 10 | 18 |
Successful localization rates
Six studies reported successful localization rates [12–17], with 445 and 441 PNs localized via HW and LM, respectively. The pooled successful localization rate was significantly higher in the LM group (LMG) (99.8%) than in the HW group (HWG) (99.8% vs. 96.0%, OR = 17; 95% CI: 0.05–0.53; p = 0.002, Figure 2 A). There was no significant heterogeneity among these studies (I2 = 0%). The risk of publication bias was not significant (p = 0.077).
Localization duration
Six studies reported the localization duration [11, 12, 14–17], including 499 and 494 patients who underwent HWL and LML, respectively. No statistically significant differences were observed between the 2 groups in terms of the pooled localization duration (MD: –0.75; 95% CI: –2.68 to 1.18; p = 0.45, Figure 2 B). There was substantial heterogeneity noted among the studies (I2 = 93%), but no single study was identified as the source of this heterogeneity based on the sensitivity analyses conducted. The risk of publication bias was not significant (p = 0.835).
Total complication rate
Five studies reported the total complication rates [11–14, 16], including 445 and 446 patients who underwent HWL and LML, respectively. The pooled total complication rate was substantially lower in the LMG (28.7%) than in the HWG (37.8%) (OR = 1.51; 95% CI: 1.12–2.04; p = 0.007, Figure 2 C). There was no significant heterogeneity among these studies (I2 = 36%). The risk of publication bias was not significant (p = 0.124).
Pneumothorax rate
Six studies reported pneumothorax rates [11, 13–17], including 487 and 525 patients who underwent HWL and LML, respectively. The pooled pneumothorax rates were comparable (24.4% vs. 18.7%) between the 2 groups (OR = 1.57; 95% CI: 0.85–2.89; p = 0.15, Figure 2 D). The heterogeneity was significant (I2 = 66%), and the sensitivity analysis indicated that the source of significant heterogeneity was Park’s study [16]. However, when removing Park’s study [16], the pooled pneumothorax rate was significantly lower in the LMG than in the HWG (10.7% vs. 19.3%, p = 0.02). The risk of publication bias was not significant (p = 0.535).
Pulmonary haemorrhage rate
Six studies reported pulmonary haemorrhage rates [11, 13–17], including 487 and 525 patients who underwent HWL and LML, respectively. The pooled pulmonary haemorrhage rate was substantially higher in the HWG (17.9%) than that in the LMG (5.7%) (OR = 3.79; 95% CI: 2.43–5.92; p < 0.0001, Figure 2 E), with no significance heterogeneity (I2 = 0%). The risk of publication bias was not significant (p = 0.159).
VATS duration
Three studies reported the VATS duration [11, 14, 16], including 270 and 285 patients who underwent HWL and LML, respectively. Pooled VATS duration was comparable between the 2 groups (MD = 1.39; 95% CI: –6.78–9.56; p = 0.74, Figure 2 F), with no significant heterogeneity (I2 = 39%). The risk of publication bias was not significant (p = 0.727).
Postoperative hospital stay
Two studies reported the duration of postoperative stay [11, 14], including 148 and 165 patients who underwent HWL and LML, respectively. Pooled postoperative stay duration was significantly lower in the LMG than in the HWG (MD = 0.79; 95% CI: 0.20–1.38; p = 0.009, Figure 2 G), with no significant heterogeneity (I2 = 37%). The risk of publication bias was not significant in the funnel plot.
Subgroup analyses
Table III shows the subgroup analysis based on the studies that compared HW with methylene blue localization. Three endpoints (pulmonary haemorrhage rates, pneumothorax, and total complication) could be pooled. The pooled total complication and pulmonary haemorrhage rates were significantly lower in the LMG than in the HWG. However, the pooled pneumothorax rates were comparable between the 2 groups.
Table III
Meta-analytic pooled results based on the studies based on hook-wire vs. methylene blue localization
Table IV shows the subgroup analysis based on the studies that compared HW with indocyanine green localization. Three endpoints (technical success rate, localization duration, and total complication rate) could be pooled. All the 3 endpoints showed comparable values between the 2 groups.
Table IV
Meta-analytic pooled results based on the studies based on hook-wire vs. indocyanine green localization
Table V shows the subgroup analysis based on the studies that compared HW with medical glue localization. Four endpoints (localization duration, total complication, pneumothorax, and pulmonary haemorrhage rates) could be pooled. The pooled pulmonary haemorrhage rate was substantially lower in the LMG than in the HWG. However, the remaining 3 endpoints showed comparable values between the 2 groups.
Table V
Meta-analytic pooled results based on the studies based on hook-wire vs. medical glue localization
Discussion
This meta-analysis compared the relative efficacy and safety of preoperative CT-guided HWL and LML for PNs. The results showed that LM was superior to HW in technical success and complication rates.
Technical success is critical for CT-guided localization, and the causes for technical failure vary based on the type of material used. With HW, the primary cause of failure is dislodgement or migration, whereas with LMs the main issue is diffusion [21, 22]. In this meta-analysis, the pooled rate of successful localization was notably higher in the group using LM compared to the group using HW. The technical success rate was notably high at 99.8% in the LMG, suggesting that LMs may be more effective than HW in localizing PNs. Factors contributing to HW dislodgement or migration include the incomplete release of the hook and patients’ respiratory movements [22]. However, the technical failure of LML can be mitigated by controlling the volume of the localization material [21].
Although the localization duration for both HW and LMs was comparable in this meta-analysis, significant heterogeneity was detected for this particular point (I2 = 93%), which questions the reliability of this finding. The variability in localization duration across different studies could be due to the varying experience levels of radiologists performing these procedures at different centres.
In comparing pooled total complication rates, it was found that LML is safer than HWL. Complications linked to localization primarily include pneumothorax and pulmonary haemorrhage. The higher complication rate following HWL could be due to factors like dislodgement of the HW [23] and the rigid nature of the HW. This meta-analysis found that while the initial pooled pneumothorax rates were similar between the 2 groups, upon revising the significant heterogeneity, the pneumothorax rate was still significantly lower in the LMG.
The duration of the VATS procedure was comparable between the 2 groups, implying that neither of the localization methods adversely affected the operative parameters. Even though the pooled postoperative hospital stay was significantly shorter in the LMG than in the HWG, this result should be further validated because only 2 studies were considered for this endpoint.
Subgroup analysis based on different LMs (methylene blue, medical glue, and indocyanine green) suggested that these LMs have a better safety profile than the HW. Even though no significant difference was seen in the total complication rate between indocyanine green and HW, a p-value of 0.07 indicated a tendency towards safer outcomes with the LM.
Nonetheless, this meta-analysis has several limitations. Firstly, the absence of any included RCTs could potentially bias the analysis results. Secondly, using different LMs in the studies could introduce additional bias, even though a subgroup analysis was performed based on different LMs. Finally, the majority of the investigations encompassed in this meta-analysis were executed in countries situated in Asia. Subsequent meta-analytic studies ought to endeavour to incorporate information from diverse global regions to expand the generalizability of the results.