Paediatric patients are a population characte-rized, among other things, by a high level of an-xiety connected with hospitalization. This can be linked to the strange environment of the hospital, the child’s inability to understand the proceedings, and their fear of the unknown. The anxiety is further aggravated by their being shifted to the preoperative area and separated from their parents for the induction of anaesthesia. The prevention of perioperative stress in a frightened child is important not only to render the child calm and cooperative for smoother induction but also to ensure better cooperation in the post-operative course. Anxiety and fear in children can lead to tachycardia, hypertension, and tachypnoea due to increased levels of catecholamines in the body [1]. It can also lower the pain threshold, leading to offensive beha-viour [2]. Forced separation from parents can cause psychological stress, leading to nightmares and maladaptive behaviour [2]. Premedication helps in overcoming these difficulties.
The route of administration of premedication should be acceptable and non-traumatic to the child. Often the intravenous (IV) route is chosen for drug administration. Because IV cannulation is painful, it can cause long-term psychological problems in the child resulting in, e.g., avoiding contact with a health care provider [2]. IV cannulation in a fully awake agitated child may require restraint of the child, which may further increase their psychological stress and worsen their anxiety. Therefore, other, non-traumatic routes of premedication such as oral, intranasal, nebulization, sublingual, or rectal might be valuable alternatives. The intranasal route has, apart from requiring no venous puncture, the advantage of high bioavailability due to rich nasal vascularity and no first-pass hepatic metabolism [18]. Hence, intranasal drugs are rapidly absorbed into systemic circulation and ensure rapid onset of sedation in children [3–5]. Children have been found to have high acceptability of the intranasal route of premedication administration in previous studies [6–8].
Midazolam, ketamine, and dexmedetomidine are some of the most commonly used drugs in premedication in children [9, 10]. Previous research has shown that when these drugs are administered intranasally or orally, they provide good parental sepa-ration and sedation, with one drug being superior to the other. As a result, these drugs were chosen for this study, but only in their combinations, The drug combinations are known to have synergistic effects, thereby reducing the dose of individual drugs required to provide similar effects and also reducing the side effects associated with the higher doses of individual drugs. Therefore, combination drugs can produce desirable effects with minimal or no side effects. As per our knowledge, there is no study done to date comparing the combinations of 3 drugs used for premedication in children through the intranasal route.
Our study aims at assessing the combination of these 3 premedication drugs – dexmedetomidine-midazolam, dexmedetomidine-ketamine, and midazolam-ketamine – in preventing preoperative anxiety in children of age group 2–4 years and thus preventing the ill effects of anxiety.
METHODS
This randomized double-blinded trial was conducted in paediatric patients after approval from the Institutional Ethics Committee (AIIMS/IEC/ 2018/661). The study was registered with the Clinical Trial Registry-India with registration number CTRI/2018/11/016471. Paediatric patients, American Society of Anesthesiologists (ASA) grade 1, between 2 and 4 years of age, posted for elective surgeries under general anaesthesia comprised the study participants. Written informed consent was obtained from the parents or the next of kin after explaining the procedure of premedication to them. Patients with recent history and active nasal bleeding, a nasal mass, active upper respiratory tract infections, history of psychiatric illness, cardiac arrhythmia, congenital heart disease, raised intracranial tension, raised intraocular pressure, or history of allergy to drugs being used were excluded. Exclusion criteria also included children who did not achieve parental separation even after 30 minutes of premedication and those with parental refusal.
Primary objectives: To assess the level of parental separation anxiety at 30 minutes after administration of intranasal premedication.
Secondary objectives: To assess the level of sedation, ease of IV cannulation, and mask acceptance at 30 minutes after administration of intranasal premedication.
Patients were divided into 3 groups of 50 each by computer-generated random number table method as follows: 1. DM Group: Patients pre-medicated with 1 µg kg–1 dexmedetomidine and 0.15 mg kg–1 midazolam intranasally; 2. DK Group: Patients pre-medicated with 1 µg kg–1 dexmedetomidine and 2 mg kg–1 ketamine intranasally; and 3. MK Group: Patients pre-medicated with 0.15 mg kg–1 midazo-lam and 2 mg kg–1 ketamine intranasally.
A pre-aesthetic check-up was done for these children a day prior to the scheduled day of surgery. Patients were kept fasting as per the standard protocol. Pre-sedation behaviour was assessed using a 4-point scale: 1 = calm, cooperative, 2 = anxious but reassurable, 3 = anxious but not reassurable, and 4 = crying or resisting.
The study drugs were prepared by an anaesthetist blinded to the observation or administration of anaesthesia. An observer completely blinded to the study and to the group allocation of the children recorded the pre-sedation scores and administered the drugs. The attending anaesthesiologist was blinded to the study drug and collected the rest of the data.
In all the groups, the drug was administered 30 minutes before surgery using a 1 ml tuberculin syringe, and the drug was instilled in both the nostrils equally with the child in the lying position in the preoperative area. Saline was added to make the total volume equal to 1 mL. The signs of nasal irritation (stingy and scratchy nose, watering of nose and eyes) were observed. Continuous monitoring of heart rate and pulse oximetry (SpO2) and mean arterial pressure (MAP) was done in the pre-operative period and was recorded every 5 minutes for 30 minutes. At 30 minutes after the intranasal dose, ease of separation from parents, sedation, and IV cannulation were evaluated by using the following scores:
Parent – separation anxiety scale [11]:
Patient unafraid, cooperative, asleep = 1;
Slight fear or crying, quiet with reassurance = 2;
Moderate fear, crying not quiet with reassurance = 3;
Crying, need for restraint = 4.
Sedation score [12]:
Ease of IV cannulation [4]:
Mask acceptance at 30 minutes on the operation theatre (OT) table was also assessed as per the following score:
Mask acceptance scale [7]:
Unafraid, cooperative, accepts mask readily = 1;
Slight fear of mask, easily reassured = 2;
Moderate fear of mask, not calmed with reassurance = 3;
Terrified, crying, and combative = 4.
Sampling and statistical analysis
Considering anxiolysis (calm at separation) as 30% in the midazolam group and 63.3% in the mida-zolam + ketamine group (Khatavkar et al. [6]), we estimated a sample size of 49 per group at 98.3% confidence interval (after applying Bonferroni correction to 95% confidence interval for 3-group comparison), 70% power, and 10% contingency. Data were entered and analysed using SPSS IBM software version 25 (IBM SPSS Advanced Statistics, Chicago, IL, USA). Nominal data were described using frequency and percentages and compared using the c2 test or Fischer exact test. Age distribution was analysed using one-way ANOVA. The haemodyna-mic parameters, heart rate, mean blood pressure, and saturation were analysed using repeated measures ANOVA. Continuous data were compared across the 3 groups using the Kruskal-Wallis test, and the significant results were further analysed using pair comparison. A P-value of < 0.05 was considered as statistically significant.
RESULTS
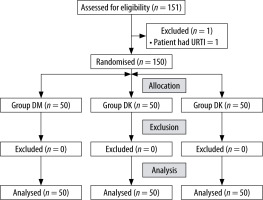
A total of 150 children aged 2-4 years and ASA class I were included in the study after fulfilment of the inclusion criteria. One patient was excluded due to the presence of an upper respiratory tract infection on the day of surgery (Figure 1).
The study groups were similar in number, age, gender, and ASA classification, as indicated in Table 1.
TABLE 1
Patient demographic data
Most of the children assessed had a preope-rative behaviour score of 3 (35.3%), 2 (29.3%), 1 (20.7%), or 4 (14.7%). The baseline pre-sedation behavioural scale of all 3 groups is indicated in Table 1.
There was a statistically significant difference (P = 0.019) in mean arterial pressure for 30 minutes after drug administration among the 3 groups. There was a slight drop in the MAP in the DM and DK groups after drug administration, which was not clinically significant and did not require any intervention. The baseline and the measured saturation (SpO2), and the heart rate for 30 minutes was similar between the groups with no statistical significance, with a P-value of 0.374 and 0.397, respectively. The heart rate and saturation remained clinically stable and similar in all 3 groups after drug admini-stration.
The difference in ease of IV cannulation at 30 minutes was statistically significant between the 3 groups, with a median value of 2 and a P-value of 0.010 with CI of 0.0–0.02 (Figure 2, Table 2). The difference in mask acceptance at 30 minutes between the 3 groups was statistically significant, with a median value of 3 and a P-value 0.007 with CI of 0.0–0.02 (Figure 3, Table 2). When compared to the other 2 groups, children in the MK group had better IV cannula insertion and mask acceptance.
FIGURE 2
Ease of intravenous cannulation at 30 minutes. The ease of IV cannulation at 30 minutes, as shown in the above figure, was statistically significant, with a median of 2 and a P-value of 0.010, with the MK group demonstrating more satisfactory results than the DK and DM groups
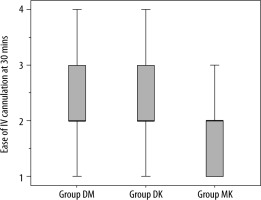
TABLE 2
Scores of parent separation anxiety, sedation, ease of intravenous cannulation, and mask acceptance at 30 minutes
FIGURE 3
Mask acceptance at 30 minutes. The mask acceptance at 30 minutes, as shown in the above figure, was statistically significant, with a median value of 3 and a P-value of 0.007, with the MK group demonstrating more satisfactory results than the DK and DM groups
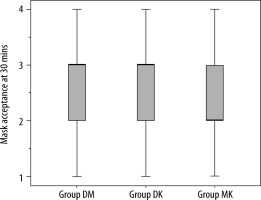
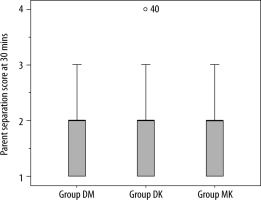
The scores of parent separation anxiety at 30 minutes between the 3 groups were not statistically significant, with a median value of 2 and a P-value of 0.82 with CI of 0.03–0.14 (Figure 4). The sedation score at 30 minutes was similar between the 3 groups, with a median value of 3 and a P-value 0.631 with CI of 0.38–0.58. All the 3 groups demonstrated adequate sedation and parental separation. The statistically significant values were further analysed in pairwise comparison by Kruskal-Wallis test. The ease of IV cannulation at 30 minutes and mask acceptance at 30 minutes showed a statistically significant difference between the MK group and the DM group, with a P-value of 0.012 and 0.005, respectively (significant values were adjusted by Bonferroni correction for multiple tests). When the groups were compared individually, the MK group had significantly better mask acceptance and IV canulation ease than the DM group, but the results for the MK and DK groups were nearly identical.
DISCUSSION
Premedication plays a vital role in relieving anxiety in paediatric patients posted for surgery. Separation anxiety is most common in children of the age selected in our study (2–4 years), and this trauma is further exacerbated by the unfamiliarity with the preoperative environment [13]. There are various psychological and pharmacological me-thods available for the child to reduce this separation anxiety [2]. The premedicant used should be acceptable, have a rapid onset, and provide good sedation. The commonly used drugs for premedication are midazolam, fentanyl, ketamine, dexmedetomidine, and clonidine.
The combination of several sedative drugs was found to have a better effect in most of the studies conducted using them [6, 14–17], while the intranasal route is relatively safe, non-invasive, and bypasses first-pass hepatic metabolism [18]. Hence, we conducted a study comparing the combinations of 3 drugs in intranasal preparation, i.e. dexmedetomidine-midazolam, dexmedetomidine-ketamine, and midazolam-ketamine.
All our patients accepted the drug via the intranasal route easily or with minimal resistance or by parental persuasion. None of the patients showed any side effects like nasal irritation, burning sensation, vomiting, or bradycardia after administration of the drug. All 3 groups of combination drugs showed stable haemodynamics with the administered doses.
This double-blinded randomized trial showed that an intranasal midazolam ketamine drug combination used as a premedication in children aged 2–4 years posted for elective surgeries under general anaesthesia produced greater ease of IV cannulation and mask acceptance at 30 minutes; however, there was no statistically significant difference in parent separation anxiety and sedation scores at 30 minutes among the 3 groups. Some patients did not achieve adequate parental separation and sedation, which could be due to drug spillage outside the nostrils during or after administration due to resistance, crying, and swallowing of the drug entering the mouth.
The groups were further compared with each other, and it was found that the DM group, DK group, and MK group had comparable parent separation anxiety, sedation scores, mask acceptance, and ease of IV cannulation at 30 minutes. The IV cannulation and mask acceptance score at 30 minutes were better in the MK group when compared with the DM group and the DK group. The children in the MK group were more comfortable clinically than the other 2 groups.
In our study, an intranasal dose of 0.12 mg kg–1 midazolam, 1 μg kg–1 dexmedetomidine, and 2 mg kg–1 ketamine in combination for premedication was chosen, similarly to previous studies [7, 14]. These doses produced good sedation and parental separation with stable haemodynamics. There were no complications like bradycardia, hypotension (< 20% of baseline), or conduction abnormalities usually associated with dexmedetomidine when used at a dose of 1 μg kg–1, which was similar to the results found by Sheta et al. [7] and other studies [19]. Excessive salivation associated with ketamine was absent at the dose 2 mg kg–1 intranasally in our study, similarly to the study of Bhat et al. [7, 15]. The study conducted by Akcay et al. [14] showed no emergence delirium or other complications, highlighting the safety of nasal ketamine with midazolam as a pre-medicant in paediatric patients. However, we did not follow the patients in the postoperative period.
There is no literature on intranasal dexmedetomidine-midazolam drug combination to date, to our knowledge, and in our study it was found that intranasal dexmedetomidine-midazolam combination was acceptable by our patients with no side effects.
The limitation of this study was that we did not follow up the patients post-operatively and we did not use an atomizer or nebulizer for intranasal administration, which can produce similar or better effects when used for intranasal drug administration compared to manual drug instillation [20].
CONCLUSIONS
The combination of midazolam and ketamine had a better clinical profile for premedication as compared to other combination drugs used in our study in terms of IV cannulation, acceptance of masks with comparable decrease in separation anxiety from parents, and adequate sedation. Therefore, it can be used as a safe premedicant in children in the age group prone to anxiety and requiring intervention like IV cannulation in the preoperative area. However, all 3 combinations of drugs can be used to decrease parental separation anxiety and to provide adequate sedation in the preoperative area.