Purpose
India’s cancer incidence is estimated at 1.15 million in 2018, and is predicted to almost double by 2040 [1]. In India, prostate cancer constitutes the 3rd most common malignancy in males, with an incidence rate of 9-10 cases per 100,000 population [2]. Depending on the stage of disease, various curative treatments include radiation (external beam radiation therapy – EBRT, brachytherapy – BT, or both), surgery, hormone therapy (HT), and chemotherapy.
Regarding healthcare facilities in India, as of date (July 30, 2022), there are a total of 612 medical colleges, which have the capability of educating 91,927 medical graduates in a year [3]. There are about 324 seats of radiation oncology specialization annually in different teaching centers of India. Till July 2023, India has approximately 609 radiotherapy centers with 671 linear accelerators, 42 tomotherapy units, 11 CyberKnife machines, 370 HDR-BT units, and 2 intra-operative radiotherapy (IORT) facilities, along with existing cobalt facilities in many centers.
In prostate cancer radiotherapy, BT plays an integral part of treatment in many countries. Results of prostate BT are comparable (if not superior) with other modalities, showing similar toxicities [4]. It may be the sole modality in low- and intermediate-risk cancer patients [5]. In high-risk and locally advanced cancer prostate cases, integrating BT with external beam treatment produces superior results in terms of biochemical progression-free survival (BFS). There is level 1A evidence advocated by international guidelines [6, 7].
Brachytherapy in India is practiced since 1918 [8]. Here, BT centers have increased rapidly over the years, and BT of cancer cervix is practiced across almost all institutions. Many of the centers are providing complex procedures, such as interstitial brachytherapy (ISBT) in locally advanced cancer cervix cases [9-11].
However, prostate BT in clinical practice has never been successful in Indian cancer hospitals [12]. Therefore, we wanted to understand the practice of ISBT in India and the attitude of Indian radiation oncologists towards prostate BT.
Material and methods
A 21-point questionnaire (Table 1) was designed in Google form and sent to radiation oncologists practicing in India, including all members of the Indian Brachytherapy Society (IBS), using texts, mails, and social media. Responses were collated, and descriptive statistical analysis was performed.
Table 1
A 21-point questionnaire
Results
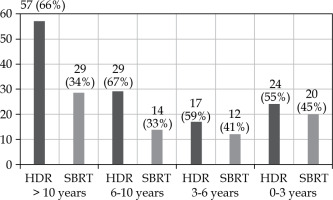
Respondents profile, patterns of ISBT, and prostate cancer treatment practice across institutions (Q. 1-7, Fig. 1A, B)
Fig. 1
Responses in: A) years in practice after speciality training, B) IGRT facility to treat prostate cancer, C) availability of HDR facility, D) practice of interstitial BT for all sites, E) availability of prostate BT template/needles, F) access to trans-rectal ultrasound (TRUS)
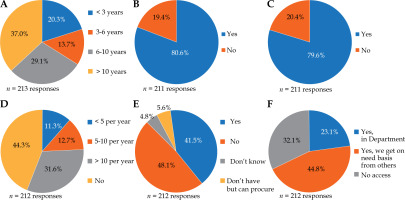
A total of 212 radiation oncologists working in 136 centers (centers of 8 respondents were not revealed) from 21 states and 4 union territories responded to the survey questionnaire, with majority (66%) of post-specialty training > 6 years, with 13.7% of over 3 but less than 6 years post-specialty training, and with 20.2% of less than 3 years. Over one-third of the respondents (n = 79, 37%) had 10 years and above of post-specialty training. 45.8% (n = 97) of the doctors worked in government teaching hospital, 31.6% (n = 67) in private teaching, and 22.2% (n = 47) in non-teaching center. In a month, almost two-thirds of the respondents (63.8%) handled 0-5 prostate cancer patients, and 35.2% (n = 75) treated more than 5 prostate cancer cases. In terms of access to facilities, 80.6% (n = 170) of the doctors had access to image-guided radiation therapy (IGRT).
We explored the patterns of practice in ISBT, as it should be the pre-requisite background to understand the infrastructure and experience of treating physicians in a department. We found that about half (44.3%, n = 94) of the respondents did not practice ISBT for any site, 31.6% (n = 67) of the doctors practiced more than 10 ISBT cases per year, 12.7% (n = 27) and 11.3% (n = 24) practiced 5-10 cases and less than 5 cases annually, respectively. Majority (83.3%, n = 175) did not practice high-dose-rate (HDR) prostate BT, 4.8% (n = 10) of the respondents claimed to practice more than 5 HDR prostate BT patients per year, 3% (n = 6) treated 2-5 cases per year, and 9% (n = 19) practiced less than 2 cases per year. Regarding boost practices across the country, only 2.8% (n = 6) of the oncologists preferred boost by brachytherapy vs. 38.1% (n = 80) by stereotactic body radiation therapy (SBRT); 10.5% (n = 22) practiced both SBRT and brachytherapy boost, and the remaining 48.6% (n = 102) practiced neither. Across 136 institutions, 11 claimed to practice less than 2 cases of prostate BT per year, 2 centers 2-5 cases per year, and 2 centers more than 5 patients per year.
Knowledge of respondents regarding prostate cancer management/indications of prostate brachytherapy (Q. 8-12, Fig. 2A-D)
Fig. 2
Responses in: A) need for prostate BT in clinical practice (200 respondents with n = 242 responses*), B) HDR-BT done to treat prostate cancer, C) introduction of HDR-BT in Indian cancer patients, D) advantage of HDR prostate BT (208 respondents with n = 451 responses**), E) use of SBRT or HDR-BT to treat prostate cancer, F) preference of HDR-BT and SBRT if all facilities are available
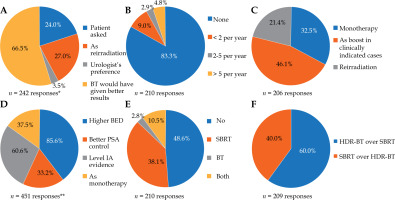
One fifth (21.6%, n = 45) and 6.8% (n = 14) of the respondents considered HT + EBRT + BT boost and HT + EBRT + SBRT boost, respectively, as the optimal management for locally advanced carcinoma prostate, while 38.9% (n = 81) preferred conventional or hypofractionated radiotherapy as the optimal choice. In the same question 68 radiation oncologists, i.e. 38% of the respondents, is open to any of the given options. When asked about the way to introduce HDR prostate BT in Indian setting, 32.5% (n = 67) of the doctors said it can be started as a monotherapy, 46.1% (n = 95) of the respondents thought that prostate BT should be initially introduced in Indian practice as boost along with EBRT, and 21.4% (n = 44) favored re-irradiation/salvage setting as the best way for HDR prostate BT to be initiated in clinical practice.
Almost all the respondents (85.6%, n = 178) agreed that HDR-BT offers higher biologically effective dose (BED), and 60.6% (n = 126) of them understood that there is level 1A evidence for BT boost in certain sub-sets of patients treated by radical radiotherapy. 33.2% (n = 69) of the respondents knew that it provides better prostate specific antigen (PSA) control, while 37.5% (n = 78) of the survey respondents believed it to be useful as monotherapy in some cases, with a definite role to play in treatment of prostate cancer by radiotherapy. Regarding contraindications to HDR-BT, 26% (n = 53) cited inability to undergo anesthesia, 17.6% (n = 36) mentioned TURP defect, 16.2% named seminal vesicle involvement, and 15.2% (n = 31) cited capsule breach. However, the majority of the respondents (70.6%, n = 144) considered all the above-mentioned factors as contraindications for HDR-BT.
More than half (66.5%, n = 133) of the oncologists had encountered the need for prostate BT at some point, and believed that prostate BT would have given better clinical result. 24% (n = 48) of the doctors mentioned that few times patients have enquired about prostate BT, while 54% (n = 27%) of the physicians would have used it in some re-irradiation setting; few oncologists (3.5%, n = 7) received a call from a referring urologist to do prostate BT at some point of their career.
Available infrastructure regarding prostate brachytherapy in centers and hurdles in practice (Q. 13-17, Fig. 1C-F)
Vast majority (79.6%, n = 168) of the respondents from 108 centers had access to HDR facilities, 41.5% (n = 88) of the doctors had access to prostate BT templates and needles/catheters, 23.1% (n = 49) to trans-rectal ultrasound (TRUS) in a radiation oncology department, and another 23.1% (n = 49) were able to access it from other departments.
We also analyzed the availability of infrastructure in institutions. There were responses from 136 institutions across India (8 respondents did not revealed their working centers), and 54 (39.7%) institutions had requisite templates and catheters. 90 (66.17%) centers had their own TRUS, or easy access to TRUS. About trained workforce, there were 9 respondents who thought they were well-trained in prostate BT.
The most cited reason for prostate BT not being popularly practiced in India was lack of training (84.8%, n = 179), followed by lack of infrastructure (69.2%, n = 146) and a belief that SBRT is an easier treatment option (54.5%, n = 155). 21.8% of the respondents had concerns regarding economic viability of prostate cancer brachytherapy program.
Despite availability of low-dose-rate (LDR) BT seeds in India [13], it may not gain preference over HDR in our country. In the question of choosing between LDR-BT and HDR-BT, 80 respondents withheld their answer because of lack of experience in prostate BT. Among those who gave an opinion, 88.9% (n = 112) said that arranging HDR-BT logistics, source procurement, training, and planning are easier.
Prospects of HDR brachytherapy and willingness to learn among the respondents (Q. 18-21, Fig. 2E, F)
Given all facilities are available, we found that 126 respondents (60%) were willing to practice HDR prostate BT, and 83 (40%) would go for SBRT. When we analyzed this profile of the doctors according to years of experience, we found a decreasing trend of interest in prostate BT among different age groups with lesser post-training experience (Figure 1). We also noted that out of 80 respondents who practiced SBRT for prostate boost, about 37 respondents (46.25%) would use HDR-BT if adequate facilities and training were provided (analyzing responses of questions No. 4 and 18). Most respondents (79.5%, n = 167) were willing to attend a dedicated prostate BT workshop for hands on training. 91.1% (n = 185) of them were ready to dedicate 2-4 days in training and education. 63.7% (n = 135) of the doctors opined that introducing prostate BT in India would help to provide optimal treatment by increasing treatment choices, while 34.4% (n = 73) of the oncologists felt that although it would provide better control, the cost of treatment would also increase.
Discussion
The present survey was undertaken to gain insight into the practice patterns as well as factors contributing to the lack of prostate BT practices in India. Previously, surveys from India regarding BT practices in general and cervical BT [9] have been published, but to the best of our knowledge, this is the first survey paper from India focusing solely on prostate BT practices.
A study by Murthy et al. was the first of its kind on prostate cancer in India. However, the issue of HDR prostate cancer BT was not considered in detail [12, 14].
Our study, with 136 centers (center of 8 respondents were not revealed) from 21 states and 4 union territories of India, represents the most widely done BT survey in this part of the world till date. Apart from the knowledge on prostate BT, this survey also indicate patterns of ISBT in India. Previous studies by Bandyopadhyay et al. and Chatterjee et al. showed that 12.3% (of 57 centers) and 49% (of 59 centers) of the responded centers were practicing interstitial gynecological BT [10, 11]. For the last 8 years, gynecological BT workshops are being held regularly by the Association of Radiation Oncologists of India, European Society for Radiotherapy and Oncology (AROI-ESTRO) group. Our recent study shows that 66% (of 136 centers) are practicing ISBT. These data (from question No. 6) included all ISBT practices, but we can assume that the improved percentage of centers practicing ISBT reflects an increased gynecological ISBT.
In a study by Vedang et al., only 3 out of 88 respondents reported using prostate BT [12]; however, we found this response to be higher in the current study. This may be because of different responders’ profile, as we have approached all IBS members.
Both HDR-BT and LDR-BT treatments show similar results [15, 16]. The benefits of HDR-BT over LDR-BT are the use of the same source for other BT procedures and lower operator dependency in case of prostate BT. In India, the practice of HDR system is widely utilized for BT, and doctors are trained and familiar to use HDR-BT in gynecological cancers, such as cervix or endometrium [9]. Due to unavailability and logistic challenges, LDR seeds have never gained popularity in India. Here, LDR seeds for prostate BT are being used by few centers only [17]. Most of the respondents in our study believed that setting up HDR prostate BT logistics would be easy. Recently in India, with the availability of LDR sources, physicians willing to choose LDR system can also choose that option.
The declining rate of BT use in the USA is due to low and declining number of prostate BT procedures performed by residents [18, 19]. Multiple factors were cited for the lack of popularity of prostate BT in India. Majority of the respondents suggested lack of training as the commonest reason, followed by lack of infrastructure, SBRT being an easier option, and economic non-viability. While lack of training was recognized as the main reason by 55% respondents in a recently conducted study by Vedang et al. from India, 85% of the respondents in our study suggested it as the main factor [12]. The issue of lack of training was found real even in countries where prostate BT has been practiced for a century; a declining trend is seen when adequate training curriculum is not maintained [18, 19]. A previous study reported that 68% of respondents provided an opinion that lack of sufficient number of patients to maintain a viable program is the reason for doctors not willing to pursue this modality [12]. We think in India, we have many HDR facilities that are used routinely for gynecological BT, so we already have a viable BT program. Additional logistics are needed to make that system work for prostate BT. With increasing life expectancy, changes in diagnostic modalities, increased awareness among the public, and changing lifestyles in Indian population, the incidence of prostate cancer will be increasing [2, 20, 21]. Therefore, it may be a good option to be prepared to deal with increasing incidence of prostate cancer. Also, with 35.2% of the respondents seeing more than 5 cases of prostate cancer patients per month, we believe viability of any prostate treatment program, such as BT should not be a problem. There are studies to suggest that SBRT boost can provide the same results, but in terms of logistics, the cost is bigger [22].
From this survey, it can be found that Indian physicians have good understanding about the benefits of HDR prostate BT, and they are well aware of how to integrate prostate cancer radiotherapy in the management of prostate cancer. Due to less exposure, they seem to be more concerned about contraindications. The survey indicates the need to train our clinicians with this conformal art of BT.
In most part of India, period from 0 to 3 years after obtaining specialty certification can be considered early level professionals, who still pursue training for further refinement. Period between 4 to 10 years are mid-level professionals, while 10 years post-specialization, radiation oncologists are serving as senior independent consultants and are in a position to decide treatment protocols and department policies. The above experience category was considered while the responses were recorded.
We found an increasing interest in prostate BT that may reflect clinical maturity and understanding gained over time that prostate BT may be an option for a better outcome (Fig. 3). Conversely, the survey shows growing popularity of SBRT among new generation of oncologists, as they are more exposed to SBRT training than BT. We found that the respondents with more than 10 years of experience are more willing to start a prostate BT program, provided that all facilities are available. Such senior members can start a BT program after discussion with hospital management.
There is an access of volumetric imaging in 61.4% (n = 84) of the centers. With 54 centers (39.4% of the surveyed institutions) having a requisite template and 90 (66.17%) centers having own TRUS or easy access to TRUS, we can conclude that lack of infrastructure is not the main factor behind lesser use of prostate BT. In spite of the lack of prostate BT practice, welcome findings of our survey are the willingness of majority of the respondents to learn prostate BT as well as their interest for a dedicated hands on workshop. Almost half of the respondents were willing to devote 2 dedicated days for such a workshop.
Training by the Groupe Européen de Curiethérapie (GEC) and the European Society for Radiotherapy and Oncology (GEC-ESTRO) for gynecological image-guided brachytherapy (IGBT) has left a positive impact, as more centers are now using interstitial IGBT in cancer cervix [23]. Apart from the improvement in logistics and HDR centers over the years, dedicated workshops on IGBT in cancer cervix can improve training, knowledge, and increased use of TRUS in pelvic BT.
TRUS is very widely used in pelvic BT procedures, such as gynecological and prostate BT [24]. This increase in interstitial gynecological BT practice may be a reason of wider availability of TRUS, as we found in this survey. We believe such improvement of interstitial and image-guided BT in cervix will also facilitate prostate BT. In fact, Bachand et al. showed that the confidence to practice prostate BT improves if residents are trained in other procedures in same site using similar instruments [25]. The change in attitude and willingness to learn prostate brachytherapy is reflected through 4 workshops, with central theme on prostate BT training that are held in India.
We can conclude that lack of training is the main factor impeding widespread use of this effective treatment among our patients. This corroborates with surveys from other countries, where it was seen that lack of training during residency is the root cause of decline in this interventional practice [26]. Training organized by the American Brachytherapy Society impacted the practice of BT, and about 80% of participants utilized this training in clinical practice [27]. A survey on prostate cancer in France among 54 centers also revealed that policy-makers need to facilitate logistics and training facilities across the centers for patients to obtain benefits of optimal treatment [28]. We advocate for dedicated workshops to adequately train our peers and encourage practice of this modality. There are instances where with good training and workshops, the ABS has successfully implemented its training strategy resulting in better outcomes in clinical practice [27, 29]. A study in Australia highlighted limited BT exposure during RANZCR training, and suggested that this training should be incorporated in specialty training program itself along with long-term BT workforce planning [30].
Conclusions
The present survey provides information on the prevalence of prostate BT services as well as the attitude of Indian radiation oncologists towards this technique. It is evident that the majority of radiation oncologists do not practice HDR prostate BT, attributing it to the lack of training and infrastructure. Most of the respondents are willing to learn and look forward to dedicated training workshops on prostate BT. Based on the survey’s results, training activities should be initiated by the Indian Brachytherapy Society with the aim to promote HDR prostate BT in India. This has the potential to translate into better utilization of HDR-BT facilities without major cost implications for healthcare providers and patients.