Adhesive tape is commonly used to secure the endotracheal tube (ETT) during general anaesthesia. Use of adhesive tape in healthcare is associated with the risk of medical adhesive-related skin injury (MARSI), defined as erythema and/or other manifestations of cutaneous abnormality that persist 30 minutes or more after removal of the adhesive [1]. MARSI can affect skin integrity, cause scar formation and pain, and increase the risk of infection [2]. In addition to mechanical injury, use of adhesive tape can produce irritant contact or allergic dermatitis-type MARSI. While the epidemiology of MARSI is not well understood, one study reported a mean daily MARSI prevalence rate of 13.0% among adult inpatients, with erythema as the most commonly observed manifestation of injury [3].
Strategies to minimize MARSI rely on the identification of product-related and patient risk factors. These include extremes of age, immunosuppression, and history of dermatological conditions [1]. Although a variety of adhesive tapes are used in clinical practice, little is known about the relative likelihood of adhesives in producing injury among patients undergoing general anaesthesia. Several case reports have shown facial skin injuries from the ETT securing tape after standard extubation in at-risk patients, prompting interest in the role of the adhesive material in producing injury [4–7]. Recently, differences in postoperative eyelid erythema were found with 2 commonly used adhesives [8]. Whether similar differences exist among adhesives used for securement of the ETT is unknown. Pre-vious research investigating securement of the ETT has focused primarily on preventing unplanned extubation and contamination of the adhesive tape [9, 10]. Few studies have examined different me-thods of ETT securement on a broader range of outcomes, such as facial skin injury [11].
At our institution, Durapore (DP) and Hy-Tape (HT) are both frequently used for securing the ETT. The decision to use one tape or the other is largely based on provider preference and habit, and anecdotally no differences have been observed in skin injury between the 2 tapes. Because HT is more expensive than DP, it may be prudent to use DP prefe-rentially to control healthcare costs. For this reason, we performed a non-inferiority study to compare DP vs. HT on the proportion of facial skin erythema.
METHODS
Patient selection
This study was approved by the Institutional Review Board at our institution (IRB #13029). After obtaining written informed consent from participants, adult patients undergoing general anaesthesia with an ETT were prospectively enrolled in this study (ClinicalTrials.gov identifier: NCT03633877, registered on 14 August 2018). We conducted a rando-mized, blinded, split-face (face divided into 2 experimental halves) study at an academic medical centre. Patients were eligible for inclusion if they were at least 18 years old and if the expected duration of surgery was greater than 30 minutes. Patients undergoing surgery in the prone position, surgery on the head, brain, neck, teeth, mouth, eyes, or face, and those with pre-existing erythema, skin trauma, or lip piercings were excluded.
Protocol and data collection
To randomly allocate study subjects to one of two groups, an online randomisation tool (research randomiser version 4.0; www.randomizer.org) was used. Allocation concealment was maintained by preparing sequentially numbered paper assignments which contained the randomisation order and was administered by non-clinical research assistants who had no role in the data analysis. Based on the randomised assignment, one side of the face was exposed to Durapore (3M healthcare, Maplewood, MN, USA), a latex-free, silk-like tape with acrylate adhesive, while the other side of the face was exposed to and Hy-Tape (Hy-Tape International, Inc., Patterson, NY, USA), a latex-free, zinc oxide-based adhesive. Patients were blinded to the tape assigned to each side of the face to secure the ETT, and the tape was applied and removed while the patient was under general anaesthesia.
Prior to induction of general anaesthesia, a baseline photograph of the perioral skin was taken in the operating room. Afterwards, anaesthesia was induced according to standard of care. Once the anaesthesia provider placed the ETT, the adhesive tapes were applied by a research assistant according to the randomisation schema. Within 5 minutes of extubation, the tape was removed and a second photograph was taken by the same research assistant. Photographs were taken under normal operating room lighting using an iPad mini 4 (Apple Inc., Cupertino, CA, USA) at 6 inches from the mouth to the lens of the camera.
After completion of data collection, skin photographs were independently evaluated by 3 blinded dermatologists to determine the presence and severity of facial skin erythema, scaling, oedema, and tearing. Photographs were cropped such that only the perioral region was visible for assessment. The outcomes were evaluated on a scale of 0-3 (0 indicating none, 1 indicating mild, 2 indicating moderate, and 3 indicating severe).
The primary outcome was the proportion of patients who had facial skin erythema with DP vs. HT. Secondary outcome measures included scaling, oedema, tearing (also measured as proportions of patients who had the outcome with DP vs. HT).
Sample size calculation
A previous study found an 8% difference in erythema when using EyeGard vs. Tegaderm; specifically, 117 (77%) vs. 105 (70%) of the 2 groups, respectively, using the McNemar test, to secure eyelids for general anaesthesia of 151 patients [8]. We decided that for this study, the threshold for non-inferiority would be 20% for the primary and secondary outcomes. Assuming an a of 0.025, we estimated we would need 99 patients (198 split-faces) to have 80% power. To account for attrition, a total of 141 patients were recruited.
Statistical analysis
Each outcome was converted from the 4-point scale to a dichotomous score, where presence was indicated by a scale rating of 1, 2, or 3, and absence was indicated by a scale rating of 0. The assessments from all 3 dermatologists were then combined to determine the outcome for each patient. In the event that the evaluation was not consistent among the 3 dermatologists, we considered the evaluation of 2 out of 3 dermatologists as the final evaluation.
Descriptive statistics were used to summarize the demographic data of the study subjects. For the primary and secondary outcomes, we used the McNemar test to calculate the percentage difference and 95% confidence intervals (CIs) of the proportion of patients with each outcome [12]. For the primary and secondary outcomes, we used a non-inferiority margin of 20% difference with respect to the 95% CI. Statistical significance was considered for results with P <0.05.
RESULTS
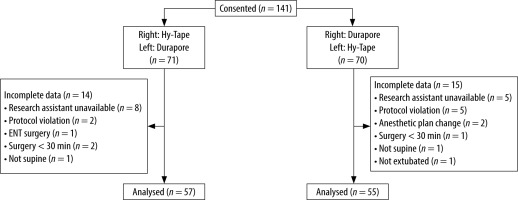
A total of 141 study subjects consented to participate and randomized to one of the two groups. Among these subjects, 112 completed the study and were included in the final statistical analysis. Twenty-nine patients were not included in the final analysis for the following reasons: research assistant unavailable (n = 13), protocol violation (n = 7), anaesthetic plan change (n = 2), surgery duration less than 30 minutes (n = 3), patient not supine (n = 2), ENT surgery (n = 1), and not extubated in the ope-rating room (n = 1). A patient enrolment flowchart is presented in Figure 1. The first patient was recruited on 17 September 2018, and the primary completion date for recruitment was 11 October 2019. The demographic characteristics of the cohort are presented in Table 1.
TABLE 1
Demographic characteristics
Table 2 shows the percentage differences in facial skin erythema, oedema, scaling, and tearing between DP and HT. On the half-face covered with DP, 64 (57%) had erythema present compared with 66 (59%) for HT, with a difference of 1.8%, less than the 20% threshold we set (95% CI: –5.6 to 9.2; P = 0.791). Figure 2 shows typical securement of the endotracheal tube with DP and HT on the right and left sides of the face, respectively, on an intubation manikin.
TABLE 2
Postoperative erythema, scaling, oedema, and tearing with Durapore and Hy-Tape
DISCUSSION
In this prospective, randomised, blinded study, we found non-inferiority in the proportion of facial skin erythema, scaling, oedema, and tearing with DP vs. HT. This was independently confirmed by 3 dermatologists at our institution.
There are several variables that could explain the non-inferiority between the 2 adhesives in this study. Skin injury occurs when the adhesion between the skin and tape is stronger than skin cell bonds [1]. We selected patients at random, and consequently many of our patients did not have risk factors for MARSI, such as advanced age. Most patients enrolled in this study were less than 70 years of age. Although skin injury can occur at any age, elderly patients are at greater risk due to physiological changes that increase susceptibility to injury. With increased age, the epidermal layer undergoes thinning, with decreased cohesiveness at the epidermal-dermal junction and overall decreased blood supply to the skin [13]. Additionally, older adults tend to have medical comorbidities, including malnutrition, diabetes, and immunosuppression, which contribute to their predisposition to skin trauma [1]. Varying levels of sebum may also have impacted this study, with increased sebum levels potentially interfering with tape adhesion and decreased levels potentially increasing the risk for MARSI [14]. Similar studies that examined the risk of facial skin injury from medical adhesives in patients undergoing general anaesthesia enrolled patients who were considered at-risk, with a notable difference observed with the compared adhesives [11].
Securing the ETT is a critical step of airway management with mechanical ventilation, but there is no universal method to provide security while minimizing the risk of facial skin injury. With an increase in surgical volume in the U.S. that is expected to continue in the post-pandemic recovery phase, as well as a rapidly growing elderly population, it is necessary to carefully examine our basic routines when taking care of at-risk surgical patients [15–17]. This includes choosing an appropriate adhesive by careful consideration of the age and risk factors of each patient that might predispose them to skin injury. Proper selection of an adhesive material is essential to avoid patient harm and potentially reduce health care costs. Given the excessive amount of waste inherent in the U.S. health care system, there is significant room for improvement across multiple domains, including the use of medical supplies [18]. At our institution, the cost of a single roll of DP is $0.61 per 2.5 cm × 9.1 m roll compared to $1.36 per 1.3 cm × 4.5 m roll of HT. There are approximately 21,780,000 surgeries performed in the U.S. each year [19]. At our institution, approximately half of all surgeries require general anaesthesia. Assuming this proportion is similar to the national average, and that a single anaesthetic requires approximately 65 cm of adhesive tape to secure an ETT, selective use of DP would result in an estimated saving of $1,650,000 annually. While there are other important factors to consider when selecting an adhesive to secure an ETT, such as strength of adhesion and risk of unplanned extubation, our study found that these 2 commonly used adhesives were both able to maintain facial skin integrity after removal. Further comparison of these adhesives in future studies could be beneficial to assess whether carrying multiple adhesives is a cost-effective strategy for medical institutions.
There are multiple limitations to this study. First, although our method for securing the ETT using 2 different adhesives is not routinely done in clinical practice, the split-face design of this study allowed us to better control for patient-related confounding variables and simplify the patient enrolment phase. Second, postoperative photographs were taken within 5 minutes of extubation and removal of the adhesive. Thus, any erythema or other manifestation of cutaneous abnormality would not meet the definition for MARSI because it must persist for 30 minutes or more after removal of the adhesive. Given our limited sample size, using erythema as a surrogate marker for MARSI was necessary because the true incidence of MARSI would not be detectable. Third, photographs were used to perform the skin injury assessments, making a physical assessment of the skin impossible. However, this approach was beneficial because it allowed for dermatologists to perform the assessment.
Tape width is a possible confounding factor in this trial; DP is 2.5 cm wide whereas HT is 1.3 cm wide. Reflecting the pragmatic design of this trial and common practices, the widths of these tapes were not altered for this trial. Another important factor to consider when minimizing risk of skin injury is the technique used to remove the adhesive. The peel force and angle during removal is often variable between providers and can contribute to greater risk of skin injury. A rapid, vertical pull generates a greater force than a slower, horizontal removal of the adhesive that stays close to the skin surface [1]. In our study, the peel force and angle were not standardized across all subjects. The pragmatic nature of this design reflects ordinary clinical practice, increasing the generalizability of our results.
In our randomized prospective controlled trial, Durapore tape used to secure the ETT was non- inferior to Hy-Tape in minimizing facial skin erythema. As such, other factors such as economics may be of greater consideration in tape selection for this purpose. Additionally, this study demonstrates the feasibility of the split-face technique and remote dermatology analysis for the study of adhesive-related skin injury.