Miller blades are the most commonly used blades for direct laryngoscopy in paediatric anaesthesia, including neonates. However, evidence that the Miller blade yields a superior view of the glottic opening compared with other blades is lacking [1, 2]. In a prospective, randomized study in infants and children, less than 2 years of age, the glottic views obtained with the Miller size 1 blade lifting the epiglottis and the Macintosh size 1 blade lifting the tongue base did not differ significantly [3]. In a second study, the glottic views and intubating conditions with the Miller and Macintosh size 1 blades in infants and children 1 month to 2 years of age were similar [4]. These data demonstrated equipoise for the glottic views with the Miller and Macintosh size 1 blades in infants and young children but shed no insight into their relative effectiveness to expose the glottic opening in neonates.
The neonatal airway presents several unique and challenging characteristics that require the skill set of an experienced paediatric anaesthesiologist to instrument the airway successfully [4, 5]. Since the introduction of Miller’s paediatric blade in 1946, it has been the standard of practice for direct laryngoscopy in infants and children including neonates [6–8]. This blade is most effective in exposing the glottic opening when it is inserted in the right paraglossal gutter, lateral to the tongue, lifting the long, floppy epiglottis, and exposing the glottic opening [3]. However, the glottic views with the Miller and Macintosh size 0 blades have not been compared in neonates. Accordingly, we designed this study to compare the glottic views (using the percentage of glottic opening [POGO] score) [9] with the Miller and Macintosh size 0 laryngoscope blades lifting the epiglottis and the tongue base in separate views as the primary endpoint and the cardiorespiratory responses as the secondary endpoints.
METHODS
After Institutional Review Board approval and registration at https://www.anzctr.org.au (ACTRN-12619000151134), 40 full-term neonates < 30 days postnatal age were enrolled. Written informed consent was obtained from the parents of each neonate. All neonates were ASA I or II, fasted, and unmedicated. Those with a history of a difficult airway or congenital syndrome, prematurity, or those with cardiopulmonary or neuromuscular disease were excluded from the study. Randomization was allocated using www.random.com and stored in sealed opaque envelopes until consent was obtained: the first randomization was the choice of the blade: Miller or Macintosh size 0 blade (Riester, Jungingen, Germany); the second was the order of lifting the epiglottis or the tongue base for the first photo. The alternate position was taken for the second photo in the same neonate.
After standard monitors (electrocardiogram, oxygen saturation [SpO2], non-invasive blood pressure, temperature, and end-tidal CO2 pressure) were applied, anaesthesia was induced with 50% air, 50% oxygen, and 8% sevoflurane. Once intravenous access was obtained, 0.5 mg kg-1 rocuronium was administered intravenously. After manually ventilating the lungs with sevoflurane in 100% oxygen for 3 minutes, laryngoscopy was performed by one of 3 paediatric anaesthesiologists using the assigned blade. The Miller size 0 blade was inserted into the mouth at the right commissure (paraglossal approach) lateral to the tongue [10]. The Macintosh size 0 blade was inserted in the midline of the mouth. The view of the glottis was optimized by repositioning the head and, if necessary, applying external, posterior laryngeal pressure. Two laryngeal views were obtained with the same blade in each neonate as described previously: lifting the epiglottis or the tongue base [3]. The glottic views were photographed by an anaesthesiologist using a digital iPhone X camera without a flash. The camera was positioned adjacent to the laryngoscope handle to photograph the best glottic views (Figure 1).
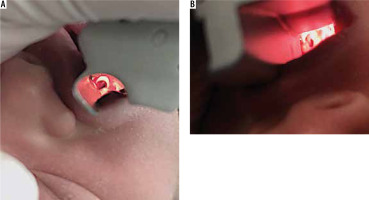
FIGURE 1
A) After optimizing the view of the glottis, the camera was positioned next to the laryngoscope handle of the Miller size 0 laryngoscope blade and focused on the vocal cords. B) After optimizing the view of the glottis, the camera was positioned next to the laryngoscope handle of the Macintosh size 0 laryngoscope blade and focused on the vocal cords
Heart rate, mean arterial pressure (MAP), and SpO2 were recorded immediately before laryngoscopy and after tracheal intubation.
Upon completion of the study, the photos of the glottis were randomized, de-identified, and reviewed using the percentage of glottic opening (POGO) score [9, 11]. The anaesthesiologist who reviewed the photos was blinded to both the study hypothesis and the blade that was used and its position when the photograph was taken.
Statistical analysis
The sample size was based on a difference of 20 in the POGO scores between the Miller and Macintosh size 0 blades, a standard deviation of 20, a 2-tailed α of 0.05, and a b of 0.2 [3]. These assumptions yielded a sample size of 16 neonates in each group. To account for dropouts and incomplete data collection, 20 neonates were enrolled in each of the Miller and Macintosh blade groups.
Data were analysed using the SPSS 22.0 program and GraphPad 6.0. Descriptive statistics were summarized as means (95% confidence intervals) (CI) for normally distributed data and medians (25–75% interval) for data that was skewed. The D’Agostino Pearson omnibus normality test was used to determine whether the data were normally distributed as per GraphPad 6.0. Normally distributed data were compared using the paired and unpaired t-tests whereas skewed and unpaired data were compared using the Mann-Whitney test. The numbers of neonates in each group were compared using c2 analysis. P < 0.05 was adopted as significant.
RESULTS
Forty-two neonates were assessed for eligibility in the study and 40 were enrolled. Of the 2 neonates who were ineligible, informed consent could not be obtained from the parents of one, and difficulty in intubating the trachea (Cormack Lehane score of 3) occurred in the second (CONSORT Flow Diagram). Of the 40 randomized neonates, 57.5% were female and 42.5% were male (P > 0.05). Thirty-two neonates underwent myelomeningocele repair and 8 underwent elective ventriculoperitoneal shunt surgery. None of the neonates sustained complications while participating in this study.
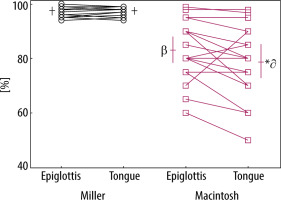
Demographic data were comparable in the 2 groups (Table 1). POGO scores (mean, 95% CI) using the Miller size 0 blade to lift the epiglottis were similar to those used to lift the tongue base (Figure 2).The POGO scores using the Miller blade were significantly greater than those using the Macintosh group for both lifting the epiglottis and the tongue base (P = 0.0001) (Figure 2).
TABLE 1
Demographic data
FIGURE 2
The POGO scores with the Miller and Macintosh size 0 blades lifting the epiglottis or the tongue base. Summary data are means and 95% confidence intervals. βThe POGO scores lifting the epiglottis with the Macintosh blade were less than those with the Miller blade (unpaired t-test, P = 0.0001). *The POGO scores lifting the tongue base with the Macintosh blade were less than with the Miller blade (unpaired t-test, P = 0.0001). ∂The POGO scores with the Macintosh blade lifting the tongue base were less than those lifting the epiglottis (paired t-test, P = 0.027)
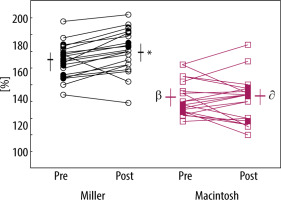
Heart rates (mean, 95% CI) post-laryngoscopy using the Miller blade were greater than pre-laryngoscopy, whereas heart rates using the Macintosh blade were similar pre- and post-laryngoscopy (Figure 3). Heart rates using the Miller blade both pre- and post-laryngoscopy were greater than those using the Macintosh blade pre- and post-laryngoscopy (P = 0.0001).
FIGURE 3
The heart rate with the Miller and Macintosh size 0 blades preand postlaryngoscopy. Summary data are means and 95% confidence intervals. * The heart rates with the Miller blade postlaryngoscopy were greater than prelaryngoscopy (paired t-test, P = 0.001). βThe heart rates prelaryngoscopy with the Macintosh blade were less than those with the Miller blade (unpaired t-test, P = 0.0001). ∂The heart rates with the Macintosh blade postlaryngoscopy were less than those with the Miller blade postlaryngoscopy (paired t-test, P = 0.0001)
MAP (mean ± 95% CI) using the Miller blade post-laryngoscopy was greater than that pre-laryngoscopy (P = 0.0001) whereas the MAP using the Macintosh blade did not differ post- and pre-laryngoscopy (Figure 4). MAP using the Miller and Macintosh blades pre-laryngoscopy did not differ; however, the MAP using the Miller blade post-laryngoscopy was significantly greater than that using the Macintosh blade post-laryngoscopy (P = 0.003).
FIGURE 4
The mean arterial pressure (MAP) with the Miller and Macintosh size 0 blades lifting the epiglottis or the tongue base. Summary data are means and 95% confidence intervals. *The MAP with the Miller blade postlaryngoscopy was greater than those prelaryngoscopy (paired t-test, P = 0.0001). ∂The MAP postlaryngoscopy with the Macintosh blade was less than that with the Miller blade (unpaired t-test, P = 0.003)

SpO2 (mean, 95% CI) post-laryngoscopy decreased significantly using both the Miller and Macintosh blades compared with pre-laryngoscopy, although the differences were of limited clinical relevance (Figure 5). SpO2 using both the Miller and Macintosh blades did not differ significantly either pre- or post-laryngoscopy.
FIGURE 5
SpO2 with the Miller and Macintosh size 0 blades lifting the epiglottis or the tongue base. Summary data are means and 95% confidence intervals. Numerals depict the number of neonates at each saturation value. *The SpO2 with the Miller blade postlaryngoscopy was statistically, but not clinically, less than that prelaryngoscopy (paired t-test, P = 0.015). βSpO2 with the Macintosh blade postlaryngoscopy was statistically, but not clinically, less than prelaryngoscopy (paired t-test, P = 0.03)

DISCUSSION
In this study, we compared the glottic views using the Miller and Macintosh size 0 blades to lift the epiglottis or the tongue base in neonates. We found that the glottic views using Miller blades to lift the epiglottis or the tongue base in neonates were similar and provided excellent views, whereas the views using the Macintosh blade to lift the epiglottis were greater than those lifting the tongue base. Overall, the POGO scores using the Miller size 0 blade to lift the epiglottis and tongue base were both significantly greater than those using the Macin-tosh blade.
In 2 previous studies, paediatric Miller and Macintosh blades were compared during direct laryngoscopy in infants and children, 1–24 months of age [3, 4]. In the first study, the glottic views in infants under 2 years of age using the Miller blade to either lift the epiglottis or the tongue base were similar to those achieved with the Macintosh blade lifting the tongue base [3]. However, when the Macin-tosh blade was used to lift the epiglottis, the glottic views were significantly worse than when lifting the tongue base [3]. This provided our first impression that the Macintosh blade may not provide as good a view of the glottic opening as the Miller blade in young infants. Also, only experienced anaesthesiologists performed the laryngoscopies, and the paraglossal approach was used with the Miller blade. In the second study, the glottic views with the Miller and Macintosh blades yielded similar views and intubating conditions [4]. However, in that study, trainees performed the laryngoscopies, and the Miller blade was not advanced via the paraglossal approach. However, the results of neither of the aforementioned studies predicted the effectiveness of these blades in neonates.
Despite finding equipoise in the overall effectiveness of the Miller and Macintosh blades to visualize the glottic opening in older infants and children [3, 4], the results of this study indicate that the glottic views with the Miller blade are superior to those with the Macintosh blade. We attribute this finding primarily to the developmentally immature upper airway in neonates compared with older children [4, 8]. The characteristics of the neonatal airway include compression of the dimensions of the upper airway (cephalad and anterior larynx), thus obscuring the glottic opening behind a relatively large tongue. The Miller blade offsets the disadvantages of these neonatal dimensions when it is used via the paraglossal approach by elevating the tongue and creating a straight-line view of the glottic opening from the anaesthesiologist’s eye to the larynx. In contrast, the Macintosh blade, with its curve, does not achieve the same direct view of the glottic opening because it does not elevate the tongue. Even with attempts to optimize the airway (external laryngeal manipulation), the POGO scores with the Macintosh lifting both the epiglottis and the tongue base were significantly lower than those with the Miller blade.
The success of tracheal intubation in neonates varies between 20% and 73% [12, 13]. Inexperienced practitioners reported the poorest success rates. An important objective of the Neonatal Resuscitation Program in North America is to teach intubation skills in neonates to paediatric residents [14]. However, this program does not recommend a specific laryngoscope blade for tracheal intubation in neonates, which, after the results of this study, may have to change to recommend the Miller 0 blade.
In the modern era, what is the optimal technique for direct laryngoscopy? Firstly, in the past, lifting the epiglottis stimulated vagal responses during light anaesthesia to a greater extent than lifting the tongue base [15]. Today, the depth of anaesthesia with modern anaesthetics precludes bradycardia during laryngoscopy even lifting the epiglottis and in the absence of anticholinergics in neonates and infants. Secondly, some refer to the use of the Miller blade to lift the tongue base as a reasonable alternative to lifting the epiglottis. Our data demonstrate that the glottic views in neonates using the Miller 0 blade in the 2 positions were indistinguishable. However, caution must be exercised when placing the Miller blade in the epiglottic vallecula because the tip of the blade is not rounded to preclude tissue trauma as is the tip of the Macintosh blade [16, 17]. Third, Miller inserted his paediatric blade at the right commissure (paraglossal approach) of the mouth, recognizing the fragility of the central incisors in young children and the ease with which they can be dislodged, compared with the stability of the bicuspids and lateral incisors. However, in the original description of his blade in adults, Miller moulded a lead tooth guard and applied it to the maxillary teeth to protect them from pressure from the blade before inserting it [18]. In contrast, Macintosh did not advocate the paraglossal approach for his blade; rather, he inserted the blade in the midline and swept the tongue to the left [17]. We employed these classical descriptions when we used the laryngoscope blades in this study.
Several reports of difficult airways in large populations of infants and children have underscored several interesting findings, although a close examination of these reports raises several important questions. In one study, the Paediatric Difficult Airway Registry in the USA reported the management of difficult airways in infants and children [19]. That database failed to detail which laryngoscope blade was used during direct laryngoscopy, whether a shoulder roll was used [20], and whether the paraglossal approach was used with the Miller blade [10, 18]. Trainees and certified registered nurse anaesthetists performed 80% of the first intubation attempts; staff anaesthesiologists performed fewer than 20% of the first attempts. Before a diagnosis of “difficult intubation” is confirmed, it behoves investigators to ensure that the approach to visualizing the glottis has been optimized in all aspects of exposing the glottis, which, based on the evidence to date, cannot be confirmed. The videoscopes and bronchoscopes that were used to successfully secure the airways neither confirm nor refute the presence of a difficult airway. In a second study, a review of more than 11,000 anaesthetics in infants and children in Germany reported that the frequency of difficult airways in infants was 6-fold greater than that in older children [21]. However, the Macintosh blade was used for all the laryngoscopies, including those in neonates. The results of the present study suggest that the substantial frequency of difficult intubations in neonates and infants using Macintosh blades may be exaggerated, at least in neonates; had the Miller blade been used in neonates, the frequency of difficult intubations may have been reduced. The frequency of difficult intubations in neonates requires that both the airway and the laryngoscopy technique are optimized to avoid the publication of weak data.
This study has several limitations. First, the sample size was small. This study was designed to compare two laryngoscope blades in neonates with normal airways undergoing elective surgery, not to report the frequency of difficult glottic visualization in a large population of neonates. Second, operator bias may have contributed to the homogeneity of the results because the anaesthesiologists were very familiar with both blades, thus limiting the external validity of the data. Had more anaesthesiologists been involved in performing the laryngoscopies with the 2 blades, then a larger sample size would have been required to offset inter-individual variability. We believe that given the hypothesis of this study and the skillset of the anaesthesiologist performing the laryngoscopies, we could not justify involving more anaesthesiologists in performing laryngoscopies. Third, although it may be tempting to apply these results to neonates with difficult airways, this should be approached with caution. Although our data demonstrate that the glottic views with the Miller 0 blade are superior to the views with the Macintosh 0 blade in healthy neonates, we did not include neonates with difficult airways. One child who was identified as having a difficult airway was excluded from participating because this was an exclusion criterion. Anatomically, we hold that the paraglossal approach with the Miller blade reduces the distance from the lips to the glottic opening and reduces the acuity of the angle between the blade and the trachea, both of which help to expose the glottis particularly in difficult neonatal airways, but that was not tested here [18]. Lastly, we quantified neither the time to achieve an adequate glottic view nor the time to tracheal intubation because the time expended to optimize the view of the glottic opening and photograph the larynx would have skewed these other times. Future studies will address the times to intubate the neonate’s airway with different laryngoscope blades.




