Introduction
During the COVID-19 pandemic traditional access to health care was limited, especially since 1 March 2020. At that time, face-to-face medical consultations were used almost exclusively for emergencies in order to reduce the risk of infection with the new disease among doctors and patients. In this difficult situation, telemedicine enabled patients to continue medical care, especially in the case of minor ailments and diseases. Telemedicine involves the use of telecommunication technologies to provide health services over a spatial distance with the aim of benefiting the patient or population [1]. The subject of our research was the rapidly developing subset of telemedicine: teledermatology. Extensions of teledermatology include teledermoscopy, teledermatopathology, or telecytology [2]. It has been found that teledermatology and teledermoscopy using smartphones are effective in the diagnosis and selection of dermatological diseases, including malignant neoplasms [3].
Aim
This study aimed to provide implications on the opportunities, application, and factors that impact the adoption of teledermatology in Poland among patients and doctors. We aimed to determine and compare participants’ perceptions of telehealth consultations to their attitude toward traditional in-person visits and investigate the sociodemographic and health-related factors associated with telehealth experiences.
Material and methods
Study population and design
This study of patients’ and doctors’ approach to telemedicine was a questionnaire-based survey. An original anonymous survey was conducted online via a survey tool for data collection (Google Forms) between 22 September 2020 and 29 December 2020 among 121 patients over 18 years of age, 63 dermatologists, and 50 doctors of other specialties. The study was approved by the Local Bioethics Committee at the Medical University of Bialystok.
Statistical analysis
Statistical analysis was performed using the c2 test in order to analyse relationships between pairs of groups. Sociodemographic data were calculated as mean with standard deviation and count (percentage) as appropriate and summarised using descriptive statistics. The analysis was conducted using GraphPad Prism 8.3.0 (GraphPad Software, La Jolla, CA, USA). Results were considered to be statistically significant at p < 0.05.
Results
Patients
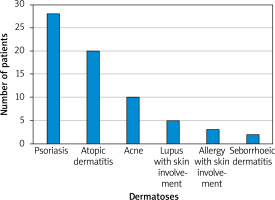
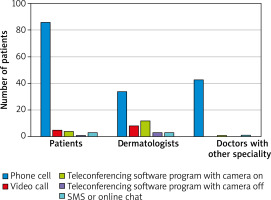
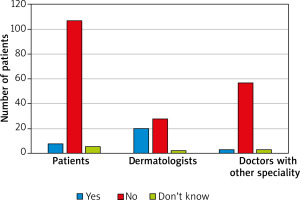
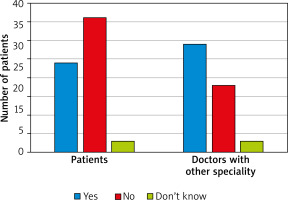
Among the group of 121 patients, 90.1% (109) were women and 9.9% (12) were men. The characteristics of the participants are presented in Tables 1 and 2. When asked about dermatological problems, 58.7% (71) of patients suffered from a skin disease: psoriasis was reported by 23% (28), atopic dermatitis 16.5% (20), and acne 8.3% (10); more than half of the patients in the study group (57%, n = 69) had been diagnosed with at least one disease other than dermatological during the analysed period (Figure 1). 37.2% of the patients with a history of any reported dermatoses had skin problems for more than 10 years, 19% between 1 and 10 years, 5.8% between a month and a year, and 2.5% under 1 month. Before the pandemic, almost two-thirds (66.1%, n = 80) had been treated by a dermatologist due to the skin problems, 29.8% (36) were had not been treated at all, 26.4% (32) had tried to treat their skin disease on their own, 18.2% (22) with the help of a doctor of other specialization, and 3.3% (4) in a beauty salon or with a cosmetologist’s help. Among patients with skin-involved problems, 57% also suffered from a disease other than dermatological and had been treated by other doctors: most commonly by a rheumatologist – 12.4% (15) subjects. When asked about ‘telemedicine’, 5.8% (7) patients did not know what the term meant, 6.6% (8) had used telemedicine before the COVID-19 pandemic, while 93.4% (113) had not had an opportunity to use this method of consultation before the pandemic. Conversely, during the COVID-19 pandemic 79.3% (96) used telemedicine, and only 20.7% (25) did not. Of respondents who used remote visits, 42.3% (41) had had 4 or more teleconsultations, 14.4% (14) – 3 times, 25.8% (25) 2 times, and 17.5% (17) once. In the majority (71.1%, n = 86) of cases teleconsultation during the pandemic was organized as a phone call (Figure 2). 63.5% (61) of the respondents declared that the discussed problems could not have been solved using telemedicine: 58.5% (56) reported a lack of ability to perform additional screenings, 53.8% (51) reported a lack of ability to assess skin lesions, and 18.5% (12) reported bad quality of internet or phone connection. Only 36.7% (37) of patients were satisfied with the quality of the telemedicine visit. Over half of the group (56.2%, n = 68) were certain that telemedicine cannot replace office visits, 32.2% (39) would rather avoid this change, 5.8% (7) would be willing to replace office visits, and only 1 (0.83%) person was certain that telemedicine could replace traditional visits. When asked about privacy during the visit, 58.6% (58) declared that they did not have an impression that their privacy was less protected compared to a regular visit. 60.6% (71) of the respondents claimed they were not satisfied with the form in which the visit was organized. Of the 121 respondents, two-thirds (66.7%) did not want their doctor’s appointments to continue in the form of teleconsultations. According to 40.5% (49), telemedicine can facilitate accessibility to a doctor. 40.5% (49) of respondents agreed that telemedicine can shorten the waiting time for a doctor’s appointment. The vast majority (81.8%, n = 99) claimed that reliable assessment of symptoms is not possible through telephone, even with visual support. A similar number of respondents – 80.2% (97) had doubt about the cost of private visits using telemedicine, they claimed it should be lower than for traditional visits. Among respondents, more than two-thirds (68.6%, n = 83) used the service of doctors other than dermatologists: family doctors – 21% (26), internal medicine doctor – 13% (16), and rheumatologist – 10% (12). 27.4% (33) claimed that this visit was more satisfying than visit using telemedicine with dermatologists.
Table 1
Responses among the analysed groups
Table 2
Characteristics of the analysed groups
Dermatologists
Among this group of 63 respondents, 59 were female and 4 were male. 95.2% (60) have been offering teleconsultations during the COVID-19 pandemic, 4.8% (3) did not. In contrast, before the pandemic only 14.3% (9) offered this solution in pursuing medical visits, and 85.7% (54) did not. Respondents from this study subgroup pointed out 5 means of communication that they used: 56.7% (34) phone call, 13.3% (8) videocall, 20% (12) Internet messenger with picture, 5% (3) text messages, and 5% (3) conversation through an online messenger (Figures 3, 4). The vast majority (90.5%, n = 57) of the dermatologists thought that telemedicine cannot replace office visits (Table 1). 46% (29) of them stated that telemedicine will not reduce the waiting time for a doctor’s appointment. Of the studied dermatologists, one-third (33.3%, n = 21) stated that telemedicine does not offer the same level of privacy protection as an office visit, while 61.9% (39) claimed that it offers a similar level of privacy. A reliable assessment without a direct visit was not possible in the opinion of 28.6% (18) of dermatologists. According to 57.1% (36) of dermatologists, telemedicine has no superiority among seniors. Among the diseases that should not be diagnosed via teledermatology, the most frequently mentioned were the following: nevi and lesions demanding dermoscopic control (92.1%), lesions in the genital area (65.1%), and those located on the scalp (60.3%). Fourteen percent (9) of respondents declared that a traditional office visit took more time, 52% (33) that teleconsultation required more time, and in the opinion of one-third (33%, n = 21) the duration of teleconsultations were similar to traditional office visits. Almost all the dermatologists (96.6%, n = 61) had scheduled an office visit or asked for additional photographs because the clinical picture during teleconsultation was not clear. Only 6.3% (4) definitely preferred telemedicine visits.
Doctors of other specialties
Among 50 doctors with (or during) a specialization other than dermatology 20% (10) were general practitioners, 10% (5) specialized in internal medicine, and 10% (5) were paediatricians. Of that studied subgroup, 74% (37) were female and 26% (13) male. During the COVID-19 pandemic, 88% (44) had been offering teleconsultations and 12% (6) had not, in contrast to the times before pandemic, when 76% (38) did not and 24% (12) did. The vast majority of consultations (95%, n = 42) were performed by telephone. Over half of the doctors (56%, n = 28) stated that telemedicine cannot replace office visits. Among all the doctors, 64% (32) felt that telemedicine will reduce the waiting time for an appointment. Telemedicine did not offer the same level of privacy protection as an office visit according to 30% (15) of respondents. Forty-four percent (22) of doctors would choose telemedicine to control the effects of treatment, and only 1 (2%) person felt sure that it was not useful in this type of consultations, while 50% (25) of respondents felt that it depends on the disease. Telemedicine would have application in elderly patients according to 58% (29) of interviewed doctors. The duration of teleconsultations was similar to traditional office visits in 48% (24). The majority of the doctors (84%, n = 42) declared that the inability to physically examine the patient during a teleconsultation may make diagnoses impossible. The vast majority (88%, n = 44) had scheduled an office visit because the clinical picture during teleconsultation was not clear.
Analysis of the study subgroups
When comparing patients’ and dermatologists’ answers, only the opinions on the possibility of reliable assessment of symptoms over the telephone and a sense of privacy were statistically significant – according to dermatologists it was possible to diagnose properly and with privacy (both p < 0.05). The comparison of patients’ and doctors of other specialties’ assessment of sense of privacy gave a statistically significant difference – patients more often felt private during telemedicine (p = 0.004). Regarding their opinion on the possibility of reliable assessment of symptoms over the telephone, patients were strongly against relying on the remote diagnosis of skin lesions, while dermatologists were willing to diagnose these changes properly, depending on the case (p = 0.003). In relation to the possibility of replacing traditional visits with telemedicine, 88.4% of the patients, 56% of other specialties doctors, and 90.5% of dermatologist denied such a possibility (there was a statistically significant difference between doctors with other specialties and dermatologists, and between doctors with other specialties and patients – both p < 0.05). Doctors of other specialties stated that telemedicine can be used in caring for elderly patients in comparison to dermatologists, and that the difference was statistically significant (p < 0.05).
Discussion
The first report concerning the provision of health services over a spatial distance can be dated back to 1879, when an article published in The Lancet showed that the use of a telephone can reduce unnecessary office visits [4]. However, only recently we can observe a tremendous development of telemedicine, and this phenomenon remains in compliance with WHO official guidelines that recommend reducing face-to-face consultations in order to decrease the potential risk of spreading the SARS-CoV-2 virus [5].
In the analysed period, only 6.6% of the interviewed persons had used telemedicine before the pandemic, compared to 79.3% who have been using telecare during the COVID-19 pandemic. In a study conducted by Handa et al. between May 2020 and October 2020 the number of teleconsultations per day rose 3.3 fold, from 23.60 in May to 77.96 in October [6]. These results highlight the expansive and growing role that telemedicine plays.
It is worth mentioning that 42.3% of our respondents have had 4 or more teleconsultations during the pandemic. Among dermatologists 39.7% stated that they had not been offering other visits than teleconsultations for the first 2 months of the pandemic (from March 11 2020). In one study, which concerned 153 U.S.-based dermatology offices open during the pandemic, it was noted that 87% of them offered teleconsultations. In the same research it was also mentioned that the number of teleconsultations in dermatology rose from 0 in April 2019 to 1564 in April 2020 at one of the U.S.-based hospitals [7].
Over 55% of patients participating in our research viewed telemedicine unfavourably. Among dermatologists in our study 41.3% stated that teleconsultations are more convenient compared to an office visit, but they preferred traditional visits. Thirty-six percent of doctors with specialties other than dermatology expressed the same view, but they were statistically more likely to state that teleconsultations are more convenient, compared to dermatologists (p < 0.05). In one study with 131 respondents who had had a video preoperative teleconsultation, 98% stated that they were satisfied with it and 92% reported that they would like such consultations in the future [8]. In our questionnaire 66.7% of respondents stated that they did not want doctor’s appointments to continue in the form of a teleconsultation. In contrast, in one study concerning urological patients 84.7% favoured teleconsultation compared to traditional visits [9]. In another study it was noted that patients who rated their experience with telemedicine lower compared to in-person visits had a lower patient activation score [10]. The patient activation score measures a patient’s ability to self-manage their healthcare [11]. In contrast, a study of Imlach et al. noted, in general, high satisfaction of patients with telehealth during lockdown; it was especially rated best for routine and familiar health issues. However, certain obstacles were noted when a physical examination was needed or when the diagnosis was unknown [12]. A study similar to ours was conducted by Yeroushalmi et al., who evaluated patients’ perception and perceived barriers of teledermatology [13]. In contrast to our respondents, very few patients reported that they were unlikely to undertake another telehealth visit (9.94%) or recommend one to others (6.92%) [13]. In our research 66.7% of patients did not want doctor’s appointments to continue in the form of a teleconsultation. One of the most commonly appearing comments in our questionnaire expressed the wish to remove teleconsultations completely, with 5 responders sharing such an opinion.
Almost all participating dermatologists had to ask for additional pictures or schedule an office visit due to an unclear clinical picture, and 91.3% of doctors with specialties other than dermatology expressed the same concerns. Furthermore, 61% of the patients declared that the problems that was discussed during teleconsultations could not have been solved using telemedicine. In research conducted by Isautier et al. it was noted that teleconsultations are not linked to a decrease in patients’ satisfaction, which stands in contrast to our findings. In this study it was also noted that 85% of older Australians stated that their experience with telemedicine was similar to or better than their experience with in-person visits [10].
The quality of network communication is considered the most important aspect influencing the development of telecare [14]. That problem is also discussed in other papers, where a high-speed Internet connection is considered essential [15, 16]. However, this was not the case among our respondents because 71.1% of teleconsultations were organized as a phone call. For 56.7% of dermatologists and 95.6% of other doctors that was also the most common type of medium. The lack of ability to organise them as a videocall was another commonly raised issue. The vast majority of our dermatologists (95.2%) have been offering teleconsultations and 56.7% of them usually in the form of a phone call without video. In one study performed before the pandemic only 20.4% of participating dermatologists offered teleconsultations, which highlights the impact COVID-19 has had on telecare’s development [17].
In our study, doctors with specialties other than dermatology were much more likely to state that telemedicine can replace office visits than respondents in the other 2 groups. Among dermatologists, only 1 subject declared that there were no dermatological conditions that cannot be treated using telemedicine. Over 90% of dermatologists stated that nevi should not be assessed using telemedicine, followed by lesions located over the genital area (65.1%) and on the scalp (60.3%). Similar opinions can be found in other papers where genital and hair disorders were named as the least suitable for a diagnosis using telecare by 28.5% and 23.9% of dermatologists, respectively [17]. Allergic disorders were the most common example of such a condition in the cited article, but they were not mentioned by any of the dermatologists in our study [17].
In our survey patients were statistically more likely to state that telemedicine does not allow doctors to adequately assess skin lesions, compared to dermatologists (p < 0.05). Almost 82% of patients expressed such an opinion, compared to 62% of dermatologists. This issue was not raised or examined in other available studies. In one study conducted among 34 dermatologists, a major challenge was the assessment of the topography and morphology of the skin lesions. That problem was highlighted by 91.2% of the responders [6]. These results point also to the risk of potential problems, including the lack of trust between medical professionals and treated patients. It may also be translated to a phenomenon which we experienced ourselves. Due to the pandemic restrictions, we mostly searched for the potential respondents online, mainly on Facebook groups. We received a significant amount comments and direct messages, commonly offensive and filled with swear words, regarding users’ opinions on telemedicine, duration of teleconsultations, and doctors’ involvement in the diagnoses and treatment using telecare, which we often had to mark as violating social media rules.
The demand for medical procedures and hospitalizations among senior citizens is the highest compared to other age groups [18]. Continuous office visits pose a risk to older adults and may be problematic to organize for their caregivers due to commonly occurring chronic diseases, functional decline, and loss of autonomy [18]. In one study the use of telemedicine allowed avoidance of 20 office visits over a 2-year period among 34 patients living in retirement homes who suffered from chronic wounds [19]. Another paper pointed out that teleconsultations helped reduce the need for office visits or hospitalizations by 79% for the elderly patients participating in the study. In our research, when asked about the possible use of telemedicine among senior citizens, dermatologists were significantly more pessimistic than doctors of other specialties.
In one retrospective cohort study it was proven that teleconsultations decreased the waiting time for an appointment with a specialist, but also allowed patients with a more severe condition to consult with a specialist faster [20]. Among our respondents, patients were statistically more pessimistic than doctors with specialties other than dermatology that telemedicine will decrease the waiting time for a doctor’s appointment (p < 0.05). In one study the patients themselves noted that they can get an appointment in days instead of weeks [12].
Even though some studies show the effectiveness of the usage of telemedicine in dermatology, issues such as legal problems and inadequate technology infrastructure seem to slow down its development in that field. The increased duration of teleconsultations reported by dermatologists may be a sign of those problems, where good quality images are a key factor in proper diagnosis and treatment compared to other areas of medicine [15, 17, 19, 21]. In one study teleconsultations required more time than in-person visits, but such a correlation was not reported with more trained professionals [15].
Telemedicine requires not only personnel training, but also both medical professionals’ and patients’ acceptance [15]. In our study, among participating patients, 57.9% strongly agreed that teleconsultation should be less expensive than an office visit. Another 22.3% stated that it should be less expensive. These results highlight even stronger patients’ views on telemedicine and the fact that it is not treated as an equivalent to a traditional office visit. In one study patients stated that they were willing to pay the same amount of money, because teleconsultations, in their opinion, required the same amount of work from the health care provider [12]. One study revealed uneasiness concerning security expressed by the participating dermatologists [17]. However, in our study 62% of dermatologists and 61% of other doctors stated that telemedicine offers the same level of privacy protection compared to an office visit. Furthermore, 59% of patients declared they have not had a feeling that their confidential data were any less secured compared to an in-person appointment. In one study patients who preferred traditional visits over telemedicine declared that personal contact with their doctor was important for them [22]. Other study concerning oncology patients highlighted that older patients may face difficulties while participating in a video teleconsultation due to the lack of technical knowledge. The same study also mentioned the increase in data transferred online, which raised security concerns [23].
The study sample was not statistically representative of the Polish population. Our participants were recruited mainly using social media, which is likely to undervalue the technical difficulties faced by telemedicine users. Females are thought to be more likely to participate in survey studies, which may be the reason for their disproportionate share. Furthermore, elderly people are less likely to be active social media users, and that might be a crucial factor in their low representation in our survey.
Conclusions
Considering our results, telemedicine is a useful and safe tool that allows doctors to communicate, diagnose, and treat without the potential risk of spreading the virus, allowing patients to get quality healthcare in the comfort of their own homes. However, patients’ dissatisfaction with telecare may reverse the progress already made and stop its further development. The results highlight the patients’ concerns about doctors’ abilities to adequately assess skin lesions and general health condition without personal contact or examination. The significant need to schedule office visits highlights the progress that has to be made in order to turn teleconsultations into an equally important part of diagnosis and treatment.