Hailey-Hailey disease is a rare hereditary acantholytic disorder characterized by the presence of vesicles and crusted erosions typically located in the flexural areas of the body (axillae, groins and sides of the neck). The disease shows autosomal dominant inheritance, and the underlying defect is a mutation in the ATP2C1 gene encoding the Ca2+/Mn2+ ATPase which is a calcium pump located on the Golgi apparatus [1]. Abnormal calcium deposition results in desmosomal separation and acantholysis [2]. The generalized type of the disease is extremely rare and is usually triggered by bacterial or viral infection, arthropod infestation or medication [3–7]. Herein we present the patient with an atypical, generalized exacerbation of the disease, in whom thorough dermoscopic examination led to the identification of the trigger factor – Sarcoptes scabiei superinfection.
A 67-year-old Caucasian man was referred to the Department of Dermatology with an exacerbation of Hailey-Hailey disease accompanied by intense pruritus. The disease had been diagnosed 19 years prior to hospitalization on the basis of a typical clinical presentation, histopathological examination showing acantholysis with a dilapidated brick wall-like appearance of the epidermis, and a negative immunofluorescence. The previous course of the disease was mild, with recurrent erythematous plaques and erosions confined to the armpits and groins. Due to the current exacerbation, the patient was treated with topical and systemic corticosteroids (prednisone up to 30 mg/day), acitretin (30 mg/day) and tetracycline (1.5 g/day), but little improvement in clinical condition and pruritus was observed.
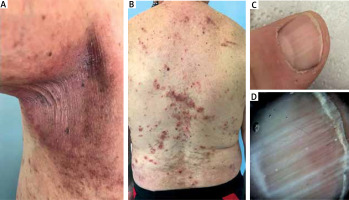
On physical examination, erythematous plaques with superficial linear fissures and erosions were observed in the axillary and inguinal regions (Figure 1 A). In addition, numerous excoriated papules and erosions with surrounding erythema were present on the back and chest (Figure 1 B). Longitudinal white bands were observed on the fingernails (Figures 1 C, D).
Figure 1
Clinical presentation. A – Erythematous plaques with single linear erosions in the armpits. B – Spreading of the lesions onto non-flexural areas – erythematous plaques, excoriated papules and erosions surrounded by erythema on the back. Excoriations may be noted on the upper back. C – Longitudinal leukonychia on the thumb. D – Dermoscopy (onychoscopy) allows for better visualization of the longitudinal white bands (Canfield D200EVO Videodermatoscope, 15× magnification, non-polarized light)
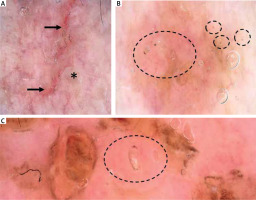
Dermatoscopy of the lesions in the armpits and groins showed a combination of white and pink structureless areas, separated by thick red lines of unspecific distribution, corresponding to small linear erosions. The whitish structureless areas were irregularly raised and folded, giving the appearance of a “crumpled fabric” (Figure 2 A). On the trunk, yellow structureless areas, corresponding to the erosions with serous exudate, were noted against a pinkish background. However, between the yellow structureless areas, dark-brown triangular structures were observed at the end of whitish serpiginous tract (“jet with contrail”) (Figure 2 B). Videodermoscopy (Canfield D200EVO Videodermatoscope) allowed for better visualization of the mites and confirmed the diagnosis of scabies (Figure 2 C).
Figure 2
Dermoscopic findings in the presented patient. A – Dermoscopy of the lesions in the armpits showing a combination of whitish and pinkish structureless areas separated by thick red lines, corresponding to linear erosions (black arrows). The whitish structureless areas are irregularly raised and folded, resembling a “crumpled fabric” (asterisk). In addition, black lines of unspecific distribution (fibres) are visible within the erosion (“sticky fibre” sign) (Canfield D200EVO Videodermatoscope, 15× magnification, non-polarized light). B – Dermoscopy of the lesions on the trunk showed presence of brown triangular structures (black circles), corresponding to the frontal part of the mites. On the left, a whitish linear structure, corresponding to the scabies burrow, is present (Canfield D200EVO Videodermatoscope, 30× magnification, non-polarized light). C – Brown triangular structure, corresponding to the frontal aspect of Sarcoptes scabiei, is present at the end of the short linear scabies burrow (black circle) (Canfield D200EVO Videodermatoscope, 50× magnification, non-polarized light)
The patient was treated with topical permetrine twice, 7 days apart. After treatment, significant improvement in skin involvement, especially on the trunk, and resolution of itching was observed. A follow-up dermatoscopic examination after 4 weeks showed no evidence of mites. Treatment with topical corticosteroids and methotrexate for Hailey-Hailey disease was initiated at the next stage.
Hailey-Hailey disease is characterized by a chronic and recalcitrant course, however, exacerbations due to infections with pyogenic bacteria or herpes simplex virus, contact allergy, ultraviolet B exposure and mechanical trauma have been mentioned in the literature [3, 4]. In such cases, generalized Hailey-Hailey disease may develop, with lesions spreading to non-flexural sites. Sarcoptes scabiei was added to the list of potential trigger factors in 2001, when the first case of atypical presentation of Hailey-Hailey disease induced by scabies superinfection was reported [5]. Similar cases were also presented later by Suehiro et al. [6] and Ikeda et al. [7]. However, none of these reports used dermatoscopy to diagnose scabies infection.
Histopathology remains the gold standard for the diagnosis of Hailey-Hailey disease, but it has been shown that dermatoscopy can be helpful in clinical evaluation and initial diagnosis [8–12]. On dermatoscopy, Hailey-Hailey disease shows an irregular combination of pink and white areas separated by pink furrows, which was termed a “cloud pattern” [8]. Another dermatoscopic feature is the “crumpled fabric pattern”, which describes the appearance of the whitish areas as irregularly raised wavy folds [10]. In the dermatoscopic analysis of 8 patients with Hailey-Hailey disease, Oliveira et al. [9] observed presence of polymorphous vessels (100%), including looped (100%) and glomerular (100%) vessels, on a pink-white (75%) or pink-yellow (25%) background, scaling (75%) and erosions (87.5%). In half of the cases, the vessels were peripherally distributed. In patients with dark skin phototypes, irregular brown-greyish-black areas/crusting may be observed as well [11, 12].
The absence of dermatoscopic features such as “pseudocomedones” and a central star-like pattern can help to rule out other acantholytic conditions, namely Darier’s disease and Grover’s disease. Longitudinal leukonychia is a valuable clue in the diagnosis of Hailey-Hailey disease [13]. In doubtful cases, dermatoscopy (onychoscopy) allows for better visualization of longitudinal white bands [13].
Dermatoscopy has been shown to be of great help in the differential diagnosis of skin infestations, including scabies, pediculosis, myiasis, tungiasis etc. [14, 15]. A separate term of “entomodermoscopy” was coined for this particular indication. In scabies, a brown triangular structure, referred to as a “hang glider” at one end of a whitish serpiginous area (“jet with contrail”) is observed on dermatoscopy [14]. The whitish area corresponds to the scabies tunnel, and the dark triangular structure is the anterior portion of Sarcoptes scabiei [15].
So far, dermatoscopy has also been used in the diagnosis of scabies infestation in the paediatric group, noting the presence of the mite in the burrows, and at the end of which the presence of larvae faeces in the form of dark, shapeless masses were found [16]. A recent observation by Oranges et al. [17] described, in addition to the classic “hang glider” dermoscopic feature, a new dermoscopic sign called the “butterfly” sign, characterized by the presence of a butterfly-shaped reddish area resembling blood [17]. The “butterfly” sign was found to correspond on microscopic examination to the well-defined gut area of the mite. The authors suggested that the novel dermoscopic sign may pose as a potential marker of Sarcoptes scabiei evolution in the era of resistance-to-permethrin development [17]. Specific dermoscopic features may also be found in nodular scabies. In a recent study by Errichetti et al. [18], the serpiginous tract and “jet with contrail” sign were noted in the majority (67.4%) of the lesions in the nodular variant of the infestation. In addition, the authors observed presence of red background (100%), dotted vessels of uniform (20.9%) or unspecific distribution (20.9%), and patchy white scales (25.6%).
We report the case of a patient with an atypical presentation of Hailey-Hailey disease due to superinfection with Sarcoptes scabiei. The underlying skin condition may favour scabies infestation. On the other hand, scratching due to intense pruritus might have led to the development of acantholytic lesions outside the flexural sites in the presented patient.
We would like to emphasize the value of dermatoscopic examination in any patient with an atypical course of the disease or unresponsive to standard treatment.








