The importance of an interdisciplinary endeavour is the capacity of multiple professionals with different backgrounds working together to deliver higher quality care [1]. The concept of medicine as an isolated discipline concerned with the restoration of health has been replaced with the concept of different health professionals working together to maintain health [2]. This type of team-based learning can occur in either academic or clinical settings, during medical school and residency, and consist of any combination of professional groups [3]. Interdisciplinary collaboration in health care is crucial to offering patient-centred care, and working collaboratively is not only essential but also crucial in providing quality and safety in patient-centred care [2]. In the thoracostomy procedure, the physician/surgeon and nursing teams must work together to achieve patient care, sharing tasks and responsibilities [2].
Thoracic drainage is a surgical technical procedure that is frequently used in urgent and critical, potentially life-threatening traumatic situations [4]. These drains have been integrated into routine practice because they are simple, effective tools to manage chest trauma and pleural pathologies [5]. However, it is important to highlight the invasiveness of such techniques. Insertion of the tube remains the physician’s responsibility [6]. The physician’s proficiency during an emergency and anatomical knowledge of the involved structures are required for the accurate positioning and standardized execution of the procedure [7]. However, even though nurses do not insert the tube, they play an important role with major responsibilities during the thoracostomy procedure. These include, for example, monitoring the container and the suction level and recording the quantity, characteristics, and content of the drainage; monitoring air-leakage; administration of pain medicine; and providing information and education strategies to patients so that they can be active in their self-rehabilitation process [6]. Nurse practitioners and physician assistants can also be involved in this teamwork.
Nursing care can be pre-procedure or post-procedure. During pre-procedural care, consent is required to perform the procedure and provision of information about the reason for and risks of the thoracostomy. Depending on the country and legislation, this action may be the responsibility of the surgeon or the physician or the nurse. They must also ensure that the patient has no doubts, and understands what will happen and what the course of treatment will entail. It is important that the nurse prepare the appropriate materials for insertion of the chest tube and later assist in the procedure, or as mentioned above, according to country and legislation, they can also perform it. During the procedure, the nurse’s priority is to monitor the patient’s response. Post-procedural care involves monitoring vital signs, helping the patient to change position, protecting the drainage system, and helping to remove the tube when necessary [8, 9]. Nurses must also teach the patient proper management of the drainage device: how to keep the bottle or the closed plastic system below the level of the chest, and to report any dysfunction [5]. Because inefficient nursing care can cause complications, educational material with information for safety and care strategies should be available for these patients [5, 8].
For these skills, an interdisciplinary care approach is fundamental. In this context, the theme of interdisciplinarity has recently been more widely addressed and studied. Interdisciplinary means integrated across disciplinary knowledge and methods from different fields in the interests of problem solving [10].
Lastly, to organize interdisciplinary care, the use of protocols is required. Care protocols are defined as systematized orientations that prioritize critical and basic situations to streamline the decision-making process. These protocols can be organized as flowcharts, usually elaborated by the institution’s experts [11]. Care protocols facilitate the organization of the work process by standardizing procedures [12]. These protocols are an interdisciplinary approach to care, which encourages teamwork and consistency in patient care.
LITERATURE REVIEW
Aim
This integrative literature review aimed to search for articles related to the thoracostomy procedure that convey the procedure and the standard care to the medical staff and the nursing team, and interdisciplinary teamwork.
The databases searched and other information sources
The search was performed in the following databases: Medical Literature Analysis and Retrieval System Online – PubMed® (National Library of Medicine) and Scientific Electronic Library Online – SciELO. PubMed® includes citations for biomedical literature from MEDLINE, life science journals, and online books. SciELO is an electronic library providing access to scientific journals in Portuguese and Spanish.
Search strategy and intervention
This is an integrative literature review, with a qualitative approach [13]. The steps were: (1) choice of research objective; (2) definition of the criteria for inclusion and exclusion of studies; (3) search of databases; (4) inclusion of selected studies in frame format; (5) analysis of results, identifying differences and conflicts; and (6) discussion and analysis of results.
Data collection process and search outcomes
Application of inclusion and exclusion criteria (1st stage), which contained the descriptors listed in the medical subject headings (MeSH): “Chest Tube AND Nursing; Chest Tube AND Care; Chest Tube AND Drainage; Chest tube AND Insertion (this descriptor was not defined by the MESH, but by its appearance in many articles)”. And the descriptors should refer to the insertion of the chest drain into humans. Publications were selected when they were available in English, Portuguese, Spanish, or French. Exclusion criteria were as follows: theses; dissertations; abstracts of works published in annals of events; editorials; letters to the editor; and articles not available online and not free to access.
The second step was to read the titles and abstracts, and the third step was to read the full article and delete repetitive or irrelevant studies. Five relevant manuscripts were used in addition to the development of the literature review because they were of great relevance, so they did not go through the selection process [14–18]. Critical evaluation of the studies was based on the results of the aforementioned reference documents, and from reviewing of the articles found in the databases, and selection of information relevant to the theme in its context in the study.
Study design
Data collection on teamwork in thoracostomy from the literature, between January 2012 and September 2020, was done in December 2020.
Quality assessment
To validate the integrative review methodology, prior to conducting the research, a protocol was developed. This research protocol was endorsed by an expert researcher on methods of integrative review and another expert researcher in the area of thoracostomy and interdisciplinary teamwork. This was done in order to validate the descriptors and their relevance to the subject. This research was exempt from Ethics Committee approval because it did not involve human beings.
Data abstraction and process
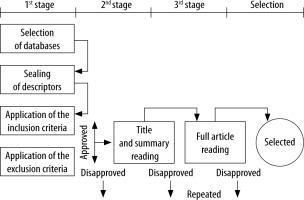
The collection of the articles was carried out in each database individually. The beginning and/or ending was not predefined, i.e. it occurred randomly. The selection criteria and the process are shown in Figure 1.
Synthesis
For the analysis procedure, we opted for content analysis [19]. This analysis was developed via 3 steps: (1) pre-exploration of the material or floating readings; (2) selection of units of analysis (or units of meanings); and (3) the non-priority categorization and sub-categorization process. The categories emerged entirely from the context of the research material. This procedure required the researchers to go back and forth from the reading of the material analysed and the objectives of the study. Each emerging category was discussed in the form of a frame within the information relevant to the study in a comparative way, along with the extraction of new information to enrich the theme.
Study risk of bias assessment and confidence in the assessment process
Two reviewers systematically evaluated the abstracts and articles to limit the risk of bias in the included or excluded studies. Only studies approved by the 2 reviewers were retained. During the analysis process, the reviewers worked independently. In the case of discrepancies in the outcome analyses, a third reviewer designated by the principal investigator reread the article.
RESULTS
After insertion of the descriptors, and before the application of the inclusion criteria, 11,277 articles were found. Most of the articles were found in Medline (99.0%). Inclusion and exclusion criteria, as well as the subsequent stages of evaluation of the articles, were applied. After excluding articles that did not meet the objective of our study, 475 abstracts were analysed (Table 1). Finally, the 19 selected articles were categorized according to Table 2, in articles with content focused on nursing care, content related to medical and surgical procedures, and interdisciplinary content.
TABLE 1
Articles found by database and selection of articles
TABLE 2
Selected articles and organization by category, title, principal author, year, country of production, methodology, and focus
| Category | Title | Principal author | Year | Country of production | Journal | Methodology | Focus |
|---|---|---|---|---|---|---|---|
| Nursing practices | Evidence-based care of patients with chest tubes | Carroll et al. [15] | 2016 | USA | American Association of Critical-Care Nurses National Teaching Institute | Evidence-based practice | To compare traditional practices with evidence-based practices and to develop evidence-based standards of practice for patients with chest tubes |
| Nurses’ knowledge of care of chest drain: a survey in a Nigerian semiurban university hospital | Kesieme et al. [8] | 2016 | Nigeria | Annals of African Medicine | Prospective cross-sectional study | To ascertain the level of knowledge of care of chest drains among nurses working in wards in a teaching hospital in Nigeria | |
| Impact of a thoracic nurse-led chest drain clinic on patient satisfaction | Williams et al. [20] | 2012 | UK | Interactive Cardiovascular and Thoracic Surgery | Prospective cross-sectional survey | To assess patient’s satisfaction with the clinic’s ability to manage their postoperative needs | |
| Medical practices | The application of low-fidelity chest tube insertion using remote telesimulation in training healthcare professionals | Garland et al. [21] | 2019 | Canada | Cureus | Technical report | To increase the technical performance of learners using a 3D-printed model |
| Evaluation of app-based serious gaming as a training method in teaching chest tube insertion to medical students | Haubruck et al. [22] | 2018 | Germany | Journal of Medical Internet Research | Randomized controlled trial | To investigate serious gaming in teaching chest tube insertion | |
| Ensuring basic competency in chest tube insertion using a simulated scenario: an international validation study | Hertz et al. [23] | 2018 | Denmark and Kingdom of Saudi Arabia | BMJ Open Respiratory Research | Prospective multicentre study | Aim was to assess the validity of a scale for chest tube insertion and to establish pass/fail score | |
| Steering the wheel towards the standard of care: proposal of a step-by-step ultrasound-guided emergency chest tube drainage and literature review | Menegozzo [24] | 2018 | Brazil | International Journal of Surgery | Literature review | To standardize a simple step-by-step technique of ultrasound-guided pleural drainage and to present a review of the potential benefits of applying ultrasound to the procedure | |
| Development and validation of an objective assessment scale for chest tube insertion under ‘direct’and ‘indirect’ rating | Ober et al. [25] | 2018 | Germany | BMC Medical Education | Randomized controlled trial | Primary objective of this study is to assess reliability and validity of the developed scale of chest tube insertion | |
| Teaching residents chest tubes: simulation task trainer or cadaver model? | Tan et al. [26] | 2018 | USA | Emergency Medicine International | Prospective randomized study | Efficacy of simulation and cadaver models in teaching tube thoracostomy and the effect on a resident’s clinical success | |
| Chest tubes: indication sizing, placement, and management | Ritchie et al. [27] | 2017 | USA | Clinical Pulmonary Medicine | Literature review | Provide a straightforward layout to educate those new to tube thoracostomy placement and enough nuance to improve the practice of some of those experienced in tube thoracostomy | |
| Impact of simulation-based training in surgical chest tube insertion on a model of traumatic pneumothorax | Léger et al. [28] | 2016 | France | Advances in Simulation | Prospective, randomized, controlled, bicentric study | To evaluate the success rate of surgical insertion of a chest tube in a task trainer simulator of traumatic pneumothorax | |
| Teaching project: low-cost pig model for training thoracic drainage | Netto et al. [4] | 2016 | Brazil | Revista do Colégio Brasileiro de Cirurgiões | Feedback questionnaire about the experimental model | To describe and evaluate the acceptance of the low-cost swine model for thoracic drainage in a medical teaching project | |
| Chest drainage teaching and training for medical students. Use of a surgical ex vivo pig model | Tube et al. [29] | 2016 | Brazil | Acta Cirúrgica Brasileira | Experimental, prospective, analytic, and controlled study | Implement a constructivist approach in thoracic drainage training in surgical ex vivo pig models, to compare the acquisition of homogeneous surgical skills between medical students | |
| A new instrument to assess physician skill at chest tube insertion: the TUBE-iCOMPT | Salmonsen et al. [30] | 2015 | Australia | Thorax | Experimental, prospective study | Objective is to develop and examine the validity of tool to assess physician skill at chest tube insertion | |
| The TACTIC: development and validation of the tool for assessing chest tube insertion competency | Shefrin et al. [31] | 2015 | Canada | Canadian Journal of Emergency Medicine | Prospective study | Aim is to develop and validate a scoring tool to assess chest tube insertion competency for paediatric emergency physicians | |
| An innovative non-animal simulation trainer for chest tube insertion in neonates | Gupta et al. [33] | 2014 | USA | Paediatrics | Prospective cohort study | The objective of this study was to assess the effectiveness of teaching the chest tube insertion procedure by using an easily constructed, non-animal simulation model | |
| Technical validation of pulmonary drainage for the treatment of severe pulmonary emphysema: a cadaver-based study | Lopez et al. [32] | 2013 | Brazil | Jornal Brasileiro de Pneumologia | Experimental, prospective cadaver-based study | To describe the pulmonary drainage surgical technique, to determine whether the site for the insertion of the chest tube is appropriate and safe, and to determine the anatomical relationship of the chest tube with the chest wall, lungs, large blood vessels, and mediastinum | |
| Interdisciplinary practices | Nurses’ knowledge and practice regard care of patient with chest drains in Sudan Heart Center, Khartoum, Sudan | Elfaki et al. [5] | 2016 | Sudan | Journal of Nursing and Health Science | Quantitative descriptive hospital-based study | To assess nurses’ knowledge and practice for patients connected to chest drain; to raise nurses’ level of knowledge and enhance their practice; to prevent and minimize chest drain risk and complications in view of improving patient outcome |
| Nurses’ knowledge levels of chest drain management: a descriptive study | Tarhan et al. [6] | 2016 | Turkey | Eurasian Journal of Pulmonology | Descriptive study using a questionnaire | To determine nurses’ level of knowledge regarding the care of patients with chest drains |
After categorization and analysis of the data, extra information emerged regarding new simulation technologies in the insertion of the chest drain that can influence the quality and success of the procedure, or even contribute to the development of new interdisciplinary procedures (Table 3). Additional themes were developed, and they included the following: experimentation with a new method and/or technology, using an alternative model to teach and evaluate drainage, considering patient characteristics and pathophysiology in the insertion of the chest drain in view of preventing complications, as well as highlighting the importance of involving nurses in the development of new techniques and procedures of chest drainage.
TABLE 3
New technologies
| Article | Author | Year | Thematic | Theme to be used |
|---|---|---|---|---|
| The application of low-fidelity chest tube insertion using remote telesimulation in training healthcare professionals | Garland et al. [21] | 2019 | 3D-printed model for teaching the medical procedure of chest tube insertion | They used an alternative simulation evaluation model |
| Evaluation of app-based serious gaming as a training method in teaching chest tube insertion to medical students: randomized controlled trial | Haubruck et al. [22] | 2018 | Use of serious gaming for teaching the medical procedure of chest tube insertion | |
| Teaching project: a low-cost swine model for chest tube insertion training | Netto et al. [4] | 2016 | Use of a pig model for insertion of a chest drain | |
| Chest drainage teaching and training for medical students. Use of a surgical ex vivo pig model | Tube et al. [29] | 2016 | Use of a pig model for insertion of a chest drain | |
| Teaching residents chest tubes: simulation task trainer or cadaver model? | Tan et al. [26] | 2018 | Participants were coached through an objective assessment checklist of 15 critical steps in chest tube insertion on simulated or cadaver model | Both sim and cadaver models are effective modalities for teaching chest tube placement |
| Steering the wheel towards the standard of care: proposal of a step-by-step ultrasound-guided emergency chest tube drainage and literature review | Menegozzo et al. [24] | 2018 | Standardization of the chest drainage procedure based on individual ultrasound techniques | The ultrasound-guided technique provides several benefits: the potential to avoid visceral injuries, intercostal artery laceration and subcutaneous drain placement are some of them |
| Nurses’ knowledge of care of chest drain: a survey in a Nigerian semiurban university hospital | Kesieme et al. [8] | 2016 | To identify the knowledge of nurses in the care and insertion of a chest drain | The importance of developing techniques of chest drainage and care with nurses |
| Nurses’ knowledge levels of chest drain management: a descriptive study | Tarhan et al. [6] | 2016 | ||
| Impact of a thoracic nurse-led chest drain clinic on patient satisfaction | Williams et al. [20] | 2012 | The quality and progression of patient care with a chest drain compared to nursing actions | |
| An innovative non-animal simulation trainer for chest tube insertion in neonates | Gupta et al. [29] | 2014 | New technologies for training and training of doctors in the insertion of the chest drain | Methodology of the research, in accomplishment of a simulation for experimentation of a new method and technology |
| Technical validation of pulmonary drainage for the treatment of severe pulmonary emphysema: a cadaver-based study | Lopez [33] | 2013 | Measurement of positioning and insertion of the chest drain in reference to other anatomical structures | The importance of considering the parameters of the patient (weight, height, etc.) and the pathophysiology in the insertion of the chest drain to prevent complications |
DISCUSSION
After exhaustive reading of selected articles and seeking to meet the study objective, according to the application of the content analysis method, the categories discussed below emerged.
Divergences in carrying out the procedure
When comparing the literature for insertion of chest drains [14–18] and articles found in the literature review, we identified differences between the procedure and care guidelines, with some divergences that could change fundamental aspects of practice, one of which is in the execution of a surgical procedure. This category, in which the closed thoracostomy is included, is strict regarding surgical asepsis. It involves patient safety as a key point, to avoid unnecessary patient complications such as discomfort and risk of death [27].
Given the importance of this, one of the divergences in the literature concerns the most adequate antiseptic in the preparation of the patient for the chest drain insertion procedure. While some studies [5] mention povidone-iodine as the preferred solution, other studies refer to alcohol-based products (chlorhexidine) [18]. Chlorhexidine may be 6% to 10% more effective in preventing infections in surgical procedures compared to povidone-iodine in patients with the same characteristics [34, 35]. Another systematic review achieved the same level of evidence and considered the reduction of costs when using alcoholic chlorhexidine (up to $26 per procedure) [36]. Several authors state that the option with the lowest incidence of infection and the highest cost-benefit is chlorhexidine alcohol [14, 34–36]. Another point of divergence in the literature is the use of 1% lidocaine [14] versus using 2% lidocaine [29] versus using neither [8]. In the literature, there are no high-quality studies on the benefits or efficacy of one over the other, only indications of different dosages, and other articles also indicate that both concentrations are acceptable [37, 38].
Success in performing a thoracostomy is related not only to the insertion of the chest tube but also to its maintenance. Basic care to ensure its effectiveness and patency are necessary. Dressing was one of the points addressed in the articles and literature of reference [8, 15–18]. Some studies recommend, as a cover, a simple dressing with petroleum gauze or lint gauze covered with micropore or tape [14–16], while others recommend transparent dressing [8]. When comparing issues such as level of skin irritation, the literature reveals that both dressings showed the same performance, but that with regards to the level of wound recovery and costs, transparent dressing presented more positive results [39, 40]. In addition to other benefits, transparent dressing decreases the risk of infection and requires a smaller number of exchanges because it can be maintained for 3 to 7 days. To conclude, transparent dressing is the most suitable for the protection of the insertion site on the chest.
As a complementary aspect, 2 studies discuss pain control and analgesia as one of the fundamental procedures in pre- and post-surgical care [6, 8]. Pain can cause patient instability leading to failure, and/or it can become the main cause of complications during and after the procedure, and it increases the length of hospital stay. Therefore, professionals should value assessment of the aspects that involve the reduction of pain and reinforce patient’s confidence in safe relevant strategies [41, 42].
Interdisciplinary action and the quality of the procedure
It is essential to promote interprofessional healthcare education and training [43]. Among the 19 studies in the systematic review, 14 only approached chest drain insertion techniques for physicians or medical students [4, 21–33]. None studied interdisciplinary work in drain insertion or chest drain care, and only 1 presented any protocol for teaching and training students in drainage [28]. On the other hand, 5 studies presented nurses as the main actors, 1 of which was an evidence-based guideline on nursing practices in the management and care of the chest drain [15], while the other 4 evaluated nurses’ knowledge and practices about chest drain care [5, 6, 8, 20]. One study, elaborated by a surgical department of thoracic surgery [8], showed how important it is to know the other professions’ roles and their importance in patient health care. It also demonstrated how it is possible to enlarge vision to interdisciplinary teamwork to improve health care. When the general principles on the care of patients with thoracic drains are implemented correctly and effectively by nurses, it will accelerate the healing process [6]. Other studies confirm the importance of the procedure protocols; once they are standardized and systematized, patient care is substantially improved. In addition, the authors suggest that nurses’ knowledge of chest anatomy and physiology is critical for rapid intervention when patients with chest drains present complications, and that the nurse must also know the reason for insertion of the drain, thereby raising awareness of the care procedures needed to maintain patient safety [6].
Finally, only 1 study directly approached the doctor-nurse partnership in the procedure and care of the chest drain, including multidisciplinary collaboration as a key point in patient care. An interdisciplinary approach to patient care is fundamental because each professional has his/her own functions and roles during chest drain insertion and care; however, all must work together for the best patient outcome [20]. Collaboration among nurses and physicians allows better patient-centred care [2]. It is also important to emphasize that the chest drain training programs should include the presence of a nurse during the insertion procedure and that national and international guidelines should emphasize the roles and duties of the nurse in the care of the patient with a chest drain [6].
Use of protocols for patient safety
Among the 20 studies evaluated in the integrative review of the literature, only 5 reported the use of protocols for insertion and management of the chest drain [6, 20, 24, 29, 33]. Two of them approached the use of protocols for teaching and training for medical students and physicians in the technique of insertion of the drain [29, 31]. Another study commented on the partnership between doctors and nurses in the care of patients with a chest tube [20]. This study assessed patient satisfaction with the ability of nurses to manage postoperative needs in a ward-based nurse-led clinic managing patients after thoracic surgery. The use of a protocol for outpatient care was created with the aim of allowing the nurses to provide their own independent care, with the option to request a physician if necessary. Most of the patients (99%) were satisfied with the care. Among the two-thirds of patients who were treated according to the protocol and without referring to a physician, very few considered that a medical consultation was necessary. Another article described a step-by-step approach for ultrasound-guided chest tube drainage [24]. Finally, a study evaluating nurses’ knowledge on chest drains suggested the creation of protocols for drainage care [6].
Patient safety needs to be the priority to the health care team [44]. Studies show that the use of evidence-based protocols contributes to patient safety, because nurses are thereby trained in patient care and are given knowledge of drainage systems [45] and the types of drainage to expect from whichever device is inserted into a patient. They can also contribute to patient safety and prevent potential harm because they can collaborate in the rehabilitation process since adequate drainage management improves effectiveness [45]. In addition, some authors argue that protocols may improve communication between doctors and nurses during care and that a standardized document improves interdisciplinary communication and drainage care [45]. Thus, it is fundamental that protocols involving procedures and patient care can be developed to delineate each discipline’s roles and responsibilities. Another fundamental factor in patient care is education. Providing patients with accurate and easy to understand information decreases recovery time and increases positive outcomes [16].
New technologies for the insertion of chest tubes
Studies also discussed the use of technology for the instruction of procedural techniques [4, 29, 33]. The use of animal models that mimic human physiology enables the development of practical skills, given the high cost and lack of accessibility of simulators or cadaver labs. Other studies go further and seek alternatives with materials that can achieve high fidelity without high-cost technology, developing their own instruments with recycled materials and proving their effectiveness for improved learning [30]. Low-cost training models for chest tube insertion were developed and tested [28, 46]. The use of a low-cost 3D-printed model for medical teaching of the procedure was analysed [21]. This model is cost-effective and valid for teaching thoracostomy. Another approach emphasized the importance of expanding knowledge of the procedure beyond the medical domain, encouraging interdisciplinary activity, and deepening knowledge and nursing responsibilities in chest drain insertion [5, 8, 20]. In this context, it behoves us to mention digital chest drainage, using digital devices that have been proven to have important benefits such as objective assessment of real air-leak, early active intervention or conversion to a one-way valve system that would allow for outpatient management, early patient mobilization, and therefore early hospital discharge [47]. Another important component is thoracic ultrasound, an imaging diagnostic technique that helps to identify the best puncture site and guides the procedure for insertion of the drainage. Chest ultrasound is essential during these invasive manoeuvres to increase safety and decrease potentially fatal complications [48].
Future research
Interdisciplinarity represents the combined courses of 2 or more disciplines like nursing and medicine [49]. In healthcare settings, clinical situations like life-threatening events require interprofessional management of the patient based on the unique disciplinary knowledge of the health professionals [49]. Reeves and Zwarenstein [50–53] have demonstrated in several studies that that interprofessional teamwork improves healthcare outcomes. When analysing the existing literature on thoracostomy and care, we can identify a large number of studies. Notwithstanding this vast amount of information, the literature is fragmented into disciplines and isolated analyses. Each discipline addresses the aspects that pertain to its own responsibilities in the execution of the procedure, but in practical reality, all actions have the same orientation (the patient’s well-being), and the different disciplines need to act together. This study enabled a comparison of surgical and nursing practices in the placement of chest drains through a dialogue with several authors on integration review and content analysis, compiling the information and defining an international standard for the procedure and materials used. From this study, it was possible to define an interdisciplinary and updated practice with safe means promoting safe chest drain insertion. Future research should aim to develop a learning and assessment tool for interdisciplinary chest tube insertion. Finally, future studies should concentrate on extensive patient education. It is essential in this type of interdisciplinary care to consider patient education and, more specifically, to train him/her in the management of thoracic drainage [54, 55].
CONCLUSIONS
Chest tube insertion should be interdisciplinary, to encourage improved teamwork organization, and not fragmented into disciplines and isolated analyses. This review is a source of rich information that can instrumentalize the creation of optimized processes for the interdisciplinary procedure of insertion of the chest drain. Therefore, it is necessary to develop interdisciplinary research bringing these results closer to multidisciplinary reality. The protocols are a good strategy, which are oriented and stimulated by health organizations promoting increased patient safety. The evaluation of interprofessional practices could also create a standard of techniques and materials that could be used internationally to become a reference for safe practice. Construction of interdisciplinary practice promotes improvement and qualification in health services, contributing to the development of research processes and the evolution of healthcare as a whole. It is also important to emphasize the importance of expanding this study, considering aspects such as patient education for self-care, monitoring air-leakage with an interdisciplinary view, proper handling during patient transport, and care according to each context (emergency, hospitalization, home).