In 1896, Fordyce firstly described numerous hemispheric dark-purple papules on the scrotum in a 60-year-old man, which was named angiokeratoma of the scrotum, also known as angiokeratoma of Fordyce [1]. Angiokeratomas most commonly arise in elderly men in the scrotum, and occasionally occur on the penis, glans, and femoral region [2]. It is characterized by multiple dark-purple (the most common), dark-red, black, or tan dome-shaped papules with a smooth surface that may be accompanied by scaling. Those papules generally distribute in parallel to superficial blood vessels or scrotal skin lines. The lesions are usually asymptomatic, but some patients might develop papule haemorrhage [3]. Clinical differentiation of this disease from diffuse angiokeratoma, malignant melanoma, or melanocytic nevus is required. A variety of treatments have been reported for angiokeratoma of the scrotum, including cryotherapy with liquid nitrogen, electrosurgery (such as electrocautery and electrofulguration), excision, lasers [3], sclerotherapy [4], and topical drug treatments (e.g. rapamycin cream and ethanolamine oleate) [5, 6]. To our knowledge, intralesional glucocorticoid injections for angiokeratoma of the scrotum have not yet been reported in literature. Herein, we present a case of angiokeratoma of the scrotum treated with intralesional injection of triamcinolone acetonide, in which a satisfactory curative effect was obtained.
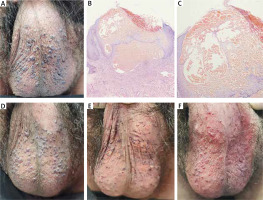
A 66-year-old man presented to our clinic with a more than four-year history of numerous dark-purple hemispherical papules with diameter 2–3 mm and smooth surface in the scrotum, often accompanied by itching and spontaneously bleeding without pain. Local thickening and pigmentation were found on the skin of the scrotum (Figure 1 A). There were no similar lesions on other parts of his body. The patient did not receive medical treatment, and there was no evidence of any systemic diseases. A skin biopsy showed hyperkeratosis, subkeratotic thrombosis, hyperplasia of the spiny cell layer, and sparse perivascular inflammatory cell infiltration in the dermis. Additionally, degenerated vascular endothelial cells were visible in the superficial dermis (Figures 1 B, C). The patient was subsequently diagnosed with angiokeratomas of the scrotum based on his clinical presentation and histopathology. The patient rejected the options of painful and destructive treatments, such as cryotherapy and electrosurgery. After informed consent, the patient initiated treatment with intralesional injection of triamcinolone acetonide (10 mg/ml, 0.1 ml/site) directly into the edge of the dense lesions (a total of 6 sites) every 2 weeks. Shortly after the initial injection, the patient responded well to the therapy, with the papules shrinking significantly (Figure 1 D). Three treatments later, the number of papules in the scrotum was significantly reduced, with smaller diameter and lighter colour. The thickness of lesion skin almost returned to normal and the hyperpigmentation improved remarkably (Figures 1 E, F). The patient is still in follow-up and continues to improve. This study was approved by the Ethics Committee of Guangzhou Institute of Dermatology, and the patient gave written informed consent to the publication of this case report.
Figure 1
A – Hemispheric dark papules on the scrotum, about 2–3 mm in diameter before intralesional injection of triamcinolone acetonide. B, C – Hyperkeratosis, subkeratotic thrombosis, hyperplasia of the spiny cell layer, and sparse perivascular inflammatory cell infiltration in the dermis (HE, B ×40; C ×100). D–F – Clinical presentation of angiokeratoma of the scrotum 2, 4, and 6 weeks after treatment, respectively
Angiokeratomas are benign capillary malformations that are usually asymptomatic but may occasionally cause bleeding, pain, and itching. Angiokeratomas of the scrotum mostly present as purple, red, or black dome-shaped papules, 1–4 mm in diameter, arranged in a linear pattern along superficial scrotal veins [3]. It is a type of genital angiokeratoma. The incidence of genital angiokeratoma has been studied in several studies, but its exact prevalence remains unclear [7]. Prolong venous hypertension, loss of venous supportive elastic tissue, and direct damage to skin capillaries may lead to angiokeratoma [8]. The histopathology is characterized by dilated capillaries in the papillary layer of the dermis and hyperkeratosis [9]. It is well known that histamine increases the permeability of small venules and causes vasodilatation [10]. Glucocorticoids have been shown to have an effect on vasoconstriction by reducing the release of factors as well as histamine [11]. Since James [12] gave the first intralesional injection of triamcinolone acetonide to treat localized dermatosis in 1960, intralesional steroid injections are now widely used in a variety of skin diseases [13, 14], for which the safety and efficacy have been confirmed by numerous experiments.
Intralesional injection of triamcinolone acetonide can rapidly achieve high concentrations in the localized lesion, resulting in local vasoconstriction, anti-inflammatory, anti-immune, and anti-proliferation effects. The present case showed that angiokeratomas of the scrotum were improved significantly after 3 intralesional injections of triamcinolone acetonide, with reducing lichenification of the scrotal skin. No local side effects such as capillary dilatation and subcutaneous fat atrophy were observed. With a large number of lesions, surgical excision, electrosurgery, and cryotherapy might lead to large invasions, which may be painful and even infectious throughout the treatment process. Postoperative hyperpigmentation, hypopigmentation, and scarring are also difficult to avoid. Laser treatment is expensive and not suitable for mass promotion (Table 1) [3–5, 7, 15]. No other side effects have been observed with intralesional injection of triamcinolone acetonide, except tolerable pain during the injection process. In addition, it is still simple, convenient, and affordable, thus making it more acceptable to the patients. We have successfully treated a variety of local proliferative or inflammatory skin diseases with intralesional injection of glucocorticoids in our clinical practice [13]. However, the efficacy and safety of this treatment for the angiokeratoma of the scrotum, including the long-term response after injection, needs to be verified with a larger sample size.
Table 1
The advantages and disadvantages of various treatments for angiokeratoma of the scrotum
| Treatments [Ref.] | Advantages | Disadvantages |
|---|---|---|
| Cryotherapy with liquid nitrogen [7] | Effective, convenient operation, suitable for several lesions | Longer recovery time, not suitable for diffuse lesions |
| Electrosurgery [15] | Operate easily with quick-effective | Painful, susceptibility to infection, high recurrence rate, not suitable for a large number of lesions |
| Excision [7] | Fast-acting and effective, suitable for several lesions | Painful, large traumatic, prone to infection, easily leave scars, not suitable for a large number of lesions |
| Lasers [3] | Easy to operate with quick-effective | Expensive, easily causes pigmentation, hypopigmentation spots or infection, not suitable for large number of lesions |
| Sclerotherapy [4] | Simple, convenient, and economical | Local irritation or slight pain, the effectiveness and safety of this method remain to be seen |
| Topical drug treatments [5] | Easy to operate, self-administered medication | With or without slight local discomfort, slow onset of action, long-time treatment |
| Intralesional injection of triamcinolone acetonide | Economical, less traumatic, no scarring, lesions shrink significantly after 1–2 injections, suitable for larger areas or a larger number of skin lesions | 3–4 injections are needed, careful attention to dosing, the effectiveness and safety remain to be seen |








