Following the administration of spinal anesthesia, debilitating headaches from dural puncture are possible. Postdural puncture headache (PDPH) is characterized by neck stiffness, tinnitus, photophobia, or nausea, and it becomes worse while sitting up straight and gets better when reclining [1].
The most effective therapy for PDPH is an auto-logous epidural blood patch, which has a success rate of more than 75%, when conservative methods such as fluids, oral medicines or caffeine, abdominal binders, and supine flat posture fail to relieve the severe headaches [2, 3]. With this invasive approach, there is a risk of dural puncture, infection, and neurologic sequelae, including motor and sensory deficits. These risks are like those of other epidural treatments [4–6].
Transnasal sphenopalatine ganglion block (SPGB) has been utilized effectively in obstetric patients with acute PDPH as well as chronic conditions such as migraine, cluster headache, trigeminal neuralgia, and atypical facial pain [7, 8]. The transnasal method is a straightforward, low-risk, non-invasive procedure that may be helpful in the treatment of PDPH. Keeping the patient in a supine position and inserting a cotton swab soaked in 2% lignocaine into the patient’s nostril is the standard technique for performing this block. Using a lignocaine nasal spray, a modified version of the technique described above has been published and found to be effective in attaining this objective [9]. As the ganglion is known to be blocked by surface application of lignocaine, a nasal spray is a less invasive and less intimidating alternative [9, 10]. The use of lignocaine spray for intranasal sphenopalatine ganglion block following spinal anesthesia for post-dural puncture headache has not been extensively explored. Hence, we planned to compare the efficacy of lidocaine spray technique to swab application, using a VAS score for pain assessment.
METHODS
Ethics statement
The study was approved by the Institutional Ethics Committee of the Indira Gandhi Institute of Medical Sciences in Patna, India (1073/IEC/IGIMS/ 2019, dated 03-10-2019). Written informed consent was obtained from all trial participants. The trial was registered prior to patient enrolment with the national trial registry [CTRI/2019/11/022069]. This manuscript adheres to the applicable CONSORT guidelines and complies with the 2013 revisions to the Helsinki Declaration. This was a double blind randomized controlled study conducted at a tertiary care university hospital between December 2019 and March 2021.
Inclusion criteria
Forty patients of either gender were included in the study. The inclusion criteria for participants included consent to take part, American Society of Anesthesiologists physical status I-III, age 18 years, PDPH within 7 days of dural puncture, and VAS score ≥ 3.
Exclusion criteria
Patients who refused to give consent, patients with known nasal septal deviation or abnormalities such as polyps, patients with a history of any disorders involving the nose such as sinusitis, rhinitis, and with a history of allergy to study medications were excluded from the study.
Study randomization and intervention
Using a block randomization method with opaque, coded, sealed envelopes, patients were allocated to two groups. In group S patients received two puffs of lignocaine 10% spray in both nostrils followed by cotton soaked in normal saline, and group B patients received two puffs of saline spray in both nostrils followed by a cotton swab soaked in lignocaine 2%. Xylometazoline drops were instilled in both nostrils 5 min before the procedure.
The patients were kept in a supine position with the neck extended during the intervention. The applicator was introduced parallel to the nasal floor until resistance was felt. The swab was placed on the posterior pharyngeal wall, just above the middle turbinate. The spray applicator was directed in the same location. The procedure was repeated on the opposite nostril. Intranasal spray was given by insulin syringe to administer the treatment (lignocaine spray and conventional saline spray) [10]. Lignocaine and saline were loaded in the insulin syringe and the swabs were prepared by an independent clinician not involved in the study. Although the swab or spray did not come into direct touch with the ganglion, the local anesthetic infiltrated the area around it. The drug’s distribution and penetration are aided by the connective tissue and mucous membrane lining. Any patient who complained of not being relieved of pain (i.e., VAS score not improving) at 1 h after the procedure had the block repeated. If there was still no relief, the outcome was labeled as treatment failure and the patient was prescribed traditional methods such as intravenous fluids, caffeine, or nonsteroidal anti-inflammatory drugs.
Patients were assessed before the procedure and 30 minutes, 60 minutes, 2, 24, 48, and 72 h after the procedure for pain relief with the help of the visual analogue (VAS) score. Heart rate and blood pressure were recorded before and after the intervention.
The primary objective was to compare the efficacy of lignocaine spray versus swab application for sphenopalatine ganglion block in the treatment of PDPH using VAS pain scores. The secondary outcomes were the assessment of patients requiring rescue analgesia, repeat procedure and development of any adverse effects of sphenopalatine block.
Sample size estimation
Sample size was calculated based on the VAS score as it was the primary outcome [9]. Assuming a pooled standard deviation of 1.47 units, the study would require a sample size of 16 for each group (i.e., a total sample size of 32, assuming equal group sizes), to achieve a power of 80% and a level of significance of 5% (two sided), for detecting a true difference in mean/median VAS score between the test and the reference group of 1.5 units.
Statistical analysis
Data were analyzed using Stata Version 10 (Stata Corp, Texas, USA). Normally distributed continuous variables were expressed as mean (95% confidence intervals) whereas non-normally distributed variables were expressed as median (interquartile range [IQR]). Repeated measure analysis of variance (ANOVA) was used to compare the VAS score at different time points between test and control groups. The independent sample t-test was used to compare the difference of means between two groups.
The Mann-Whitney test was applied to compare the VAS score between groups at each point of time while the Kruskal-Wallis test was applied to test the equality of median VAS score over time.
Using the paired t-test, the variation in clinical factors was evaluated. A P-value less than 0.05 indicated statistical significance.
RESULTS
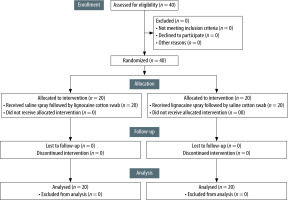
A total of 40 patients were recruited and analyzed (Figure 1). Table 1 presents the baseline demographic and clinical parameters between test and control groups that were comparable.
TABLE 1
Baseline demographic and clinical profile of patients in group S and group B
The mean VAS score of pain differed substantially between the two groups at each time point; additionally, the VAS score was significantly lower in group S than in group B until the second hour (Table 2). The Kruskal-Wallis test was applied to test the equality of median VAS score over time i.e., from baseline to 72 hours within each group S and B. VAS score was significantly different from baseline until the second hour in Group S (P = 0.0001) and until 48 hours in Group B (P = 0.0001). The Mann-Whitney test was applied to compare VAS score between Group S and B at each point of time. In both groups, the VAS score was significantly different until 1 hour from baseline. Following the block, the median VAS score in group S was 0 at the second hour, and it remained at 0 for the trial period. The median VAS score in group B was 2 at two hours and it was at 0 from 24 to 72 hours. To assess the impact of intervention on VAS score in both groups with a time variable, repeated measures analysis of variance was performed (Table 3). The comparison of hemo-dynamic parameters of patients in both group B and group S is shown in Table 4. The paired t-test was applied to assess significant changes of these parameters within the group, i.e., before and after the intervention. To evaluate the means of variables between the groups, a two-sample t-test was utilized. None of the variables were found significant within or between the groups before and after the intervention, indicating comparability of these variables between the two groups.
TABLE 2
Average VAS score in group B and group S at baseline and up to 72 hours
TABLE 3
Impact of intervention on VAS score in group B and group S (repeated measures ANOVA)
| Source | Partial SS | d.f. | Mean SS | F | P-value |
|---|---|---|---|---|---|
| Model | 1557.97 | 13 | 119.84 | 96.08 | 0.0001 |
| Group | 49.72 | 1 | 49.72 | 39.87 | 0.001 |
| Time | 1472.62 | 6 | 245.43 | 196.76 | 0.001 |
| Group*Time | 35.62 | 6 | 5.93 | 4.76 | 0.009 |
| Residual | 331.80 | 266 |
The side effects observed after the intervention included nausea, vomiting and stiff neck (shown in Table 4), and were found to be non-significant (χ2 = 3.11, Fishers’ exact P-value = 0.47).
TABLE 4
Comparison of clinical variables between group S and group B before and after intervention
Two patients each in both groups received repeat interventions after one hour of initial treatment. No patient required any rescue analgesic during the study duration.
DISCUSSION
In our study we used two puffs of lignocaine 10% spray in both nostrils and found it to be as effective in alleviating PDPH as the application of lignocaine swab for SPG block. The primary finding of our study was that lignocaine 10% spray is more effective in treating PDPH following spinal anesthesia, particularly in the first two hours after headache onset. There was no significant side effect such as nausea, vomiting, stiff neck, etc. Two patients in the group required the block to be repeated. A few patients complained of mild discomfort in the form of lacrimation during cotton swab application in the first hour of block. None of the vital parameters such as heart rate and blood pressure were affected by the block.
It is known that 0.5% to 24% of spinal anesthesia cases are complicated by PDPH. The cerebrospinal fluid leakage causes a reduction in intracranial pressure [11]. Brain hyperperfusion caused by an abrupt increase in cerebral blood flow following global vasodilation during spinal anesthesia may be one of the underlying mechanisms of PDPH. Through parasympathetic activity, compensatory vasodilation restores intracranial volume. In addition, traction on the pain-sensitive intracranial structures leads to a throbbing headache. Conservative therapies recommended for PDPH include hydration and bed rest. These treatments seek to reduce cerebrospinal fluid loss through the dural holes and replenish it through increased fluid ingestion [12]. Although these techniques are easy to apply and do not have any significant negative side effects, there are insufficient data to recommend their usage in the prevention of PDPH [13, 14]. The authors of a 2016 Cochrane review found insufficient proof that routine bed rest following a dural puncture prevents PDPH [12]. In addition, bed rest likely increased PDPH in comparison to early ambulation. Patients who fail to respond to conservative treatment within 48 hours must undergo additional interventions. The preferred treatment for moderate to severe PDPH is an epidural blood patch, but it is invasive.
This parasympathetic activity is inhibited by SPGB, which inhibits vasodilation and diminishes PDPH. The sphenopalatine ganglion is an extracranial neural structure with sympathetic and parasympathetic components as well as somatic sensory origins. It is in the pterygopalatine fossa and is accessible via transcutaneous or transnasal routes. However, the transnasal SPGB is very simple and the two methods that can be used are a cotton swab soaked with local anesthetic and the nasal spray method. The ganglion is not directly contacted by the swab, and the connective tissue and mucous membrane aid the local anesthetic reach the ganglion [15]. A study suggested that the mechanism may be mechanical stimulation of the sphenopalatine ganglion, as saline placebo also provided pain alleviation [16]. The better absorption of spray through mucous membrane and connective tissue may be due to its larger area of spread.
The data available to support the efficacy of the SPGB in treating PDPH are limited and consist primarily of case reports and case series. Cohen et al. [8] published the first article describing the effectiveness of the SPG block for the management of PDPH in 2009. They described their experience with thirteen parturients who were treated with SPGB for mild to severe PDPH. Eleven out of thirteen patients had pain relief without requiring an epidural blood patch, while the remaining two patients required it.
In a case series of 3 patients sphenopalatine block was given with lignocaine spray (two puffs of 10 mg in each nostril); all three patients had significant pain relief and were discharged asymptomatic [17]. A single blind study was done on 20 obstetric patients comparing the SPGB by lignocaine spray 10% with the 2% viscous lignocaine applicator method. This study concluded that both transnasal SPGB techniques resulted in a considerable reduction in pain from baseline after the block, with the applicator technique resulting in greater pain alleviation [18]. The beneficial effects of intranasal lignocaine spray are described in another case series of 11 individuals who developed PDPH after spinal anesthesia. Out of 11, 6 patients experienced total symptom alleviation and continued to be symptom-free after 24 hours without needing any additional treatment. After an hour (VAS 4 or 5), the treatment had to be repeated in 5 individuals. Following a second dose, there was no pain reduction in three individuals. They were instructed to drink lots of liquids while also being given oral paracetamol. After 3 days, their symptoms disappeared.
Both the techniques of SPGB for PDPH were found to be safe and effective. The spray technique also has other benefits, as described elsewhere. It is less traumatic, less intimidating to the patient and also can be administered at home if there is a recurrence of pain after discharge from hospital [9].
The limited sample size and the fact that this was a single site study are two limitations of our research. The inclusion of a heterogeneous group of patients was another limitation of the study.
CONCLUSIONS
We found that both techniques of sphenopalatine ganglion block provide effective pain relief in post-dural puncture headache following spinal anes-thesia without causing any significant side effect. The 10% lignocaine spray technique appears to be superior, especially during the early period.