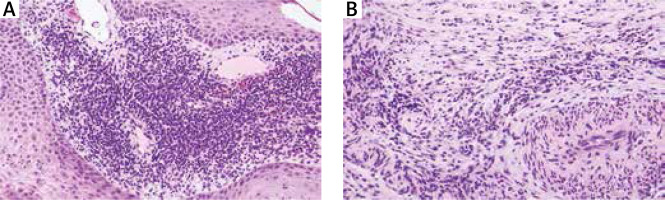
A 47-year-old female patient presented with a few months’ history of a painless ulcerated lesion on the face (Figure 1 A). Her medical history included paranoid schizophrenia. Clinical examination revealed a deep irregular ulcerative lesion with a raised erythematous border partially covered with a yellow granulation tissue and an eschar covering the centre of the forehead, the cheeks and the nose bridge reaching to the internal eye-corner on both sides (Figure 1 B). Based on the unclear history of the psychiatric symptoms and the isolation of Enterococcus faecalis in tissue culture, the provisional diagnosis of dermatitis artefacta was made. Other differential diagnoses included pyoderma gangrenosum and squamous cell carcinoma. The lesion progressed despite systemic and local antibiotics. Skin biopsy demonstrated granulocytic inflammatory infiltrate with numerous plasma cells and eosinophils as well as the features of obliterating endarteritis (Figures 2 A, B). The marked presence of plasma cells in the lesional biopsy prompted us to order a serum specific treponemal test (TPHA), which was reactive and the rapid plasma reagin test (RPR), which was negative. A diagnosis of the gummatous type of cutaneous tertiary syphilis was suggested. It was later discovered that the patient was diagnosed with syphilis during her pregnancy approximately 25 years ago and underwent the treatment in the form of injections, however no further medical details were obtained. There were no neurological, cardiac or ophthalmological abnormalities. The cytological and serological analysis of the cerebrospinal fluid were also negative. The patient was treated with penicillin G (24 million U/day intravenously for 14 days) and three intramuscular injections of benzathine benzylpenicillin 2.4 MU at weekly intervals. The enzymatic debridement of the necrotizing wound, topical antibiotics and synthetic wound dressing were used locally which led to a stepwise resolution of the skin lesion within 1 year (Figures 1 C, D).
Figure 1
A – Single skin-coloured nodule with an erythematosus border on the forehead 3 months prior to admission to our Unit. B – Asymptomatic punched-out ulcerated lesion covered with a granulation tissue and an eschar on the face upon admission before the treatment. C – A stepwise healing of the lesion in course of the treatment. D – Widespread scarring of the lesion 1 year following the diagnosis
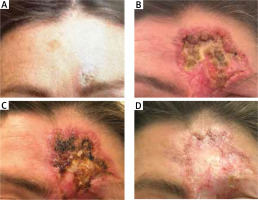
Figure 2
A – Psoriasiform hyperplasia of epidermis with a dense plasmacellular infiltrate around blood vessels of superficial plexus. B – Medium-sized vessel in reticular dermis with obliterated lumen, surrounded by numerous plasma cells
Syphilis is a systemic infectious disease caused by the spirochete Treponema pallidum [1]. Due to the variety of clinical presentations, syphilis is often called “the great masquerader” of other conditions. Although syphilis has a worldwide distribution, its incidence rate in Poland has been increasing in recent years [2].
If left untreated, almost one-third of patients with primary or secondary syphilis can develop the tertiary stage of the disease [3]. Late signs of the disease can present as cardiovascular syphilis, neurosyphilis or late benign syphilis in which the essential lesion is the gumma [1]. The gumma develops from 1 to 46 years after healing of the primary and secondary lesions [1]. The skin, bone and liver are the most common sites of involvement [1]. Cutaneous tertiary syphilis, which accounts for 16% of all late syphilis cases, may present as a superficial noduloulcerative type or a more destructive and rare, gummatous type [3]. The latter appears as a non-tender and nodular lesion leading to a central punched-out necrosis. Histologically, granulomas with multinucleated giant cells are confined to the dermis within lymphocytic and plasma cell infiltrate. Abundant presence of plasma cells is characteristic for the diagnosis of syphilis [4]. Due to the scarcity of the organism, silver stains or immunohistochemical stains for Treponema pallidum are often negative [4].
This case exhibits a gummatous form of late syphilis in an immunocompetent female patient. Its relevance arises from its unusual and dramatic presentation in an individual with schizophrenia in whom it clinically mimicked dermatitis artefacta. Similarly to previous cases [5, 6], the gumma appeared about 20 years after exposure to treponema pallidum and progressed very rapidly. Unlike other case reports, the healing process in our patient was slow despite the penicillin treatment [5, 6].
Syphilitic gumma is now an extremely rare condition, which can be easily misdiagnosed and requires a high level of suspicion due to its clinical polymorphism. Therefore, awareness of this clinical presentation is necessary to facilitate the proper diagnosis and treatment of cutaneous tertiary syphilis.








