Circumcision is a well-recognized surgical procedure that has been described since ancient times [1]. It is estimated that about 30% of males undergo circumcision worldwide [2]. It is usually carried out for religious reasons in Muslim and Jewish countries but is also performed due to medical indications, which in-clude chronic sclerosing inflammation and phimosis [3].
Pain after paediatric circumcision is severe, especially during the early postoperative period. Inadequate pain control in paediatrics could pose adverse effects, including, adverse haemodynamic, hormonal, metabolic, immunological-inflammatory responses, postoperative restless and agitation, disturbed sleep rhythm, and exaggerated pain perception with later painful surgical exposures. Therefore, it is better to prevent the onset of pain than to relieve it [4, 5].
Regional anaesthesia procedures can be safely utilized as adjuvant to general anaesthesia to achieve adequate intra- and postoperative analgesia in all paediatric age groups. It is an essential component of a multimodal pain control that should be performed wherever appropriate and possible [6]. The use of regional anaesthesia results in greater haemodynamic stability; the intraoperative opioid consumption is reduced, thus enabling a rapid and smooth recovery of children from anaesthesia and shortened hospital stay [7].
Caudal anaesthesia is one of the regional anaes-thetic techniques used frequently in children for perioperative analgesia. It is preferred because all types of surgery below the umbilicus can be covered by it: ‘one technique fits all’, besides being easy to learn with an excellent safety profile [8], while peri-pheral nerve blocks could provide longer analgesia restricted to the site of surgery, e.g. penile nerve block (PNB) [9].
We designed this study to compare the efficacy, postoperative analgesia duration, and complications between dorsal penile nerve block (DPNB), caudal nerve block (CNB), and their combination.
METHODS
After obtaining approval from the Research Ethical Committee of the Faculty of Medicine at Ain Shams University (approval no. FMASU MS 573/2021) and registering this study in Clinical Trials.gov (Clinical Trial ID NCT 05342259), the study was carried out according to the Consolidated Standards of Reporting Trials (CONSORT) 2010 statement. Written informed consents from the patients’ guardians were obtained. The study was conducted in the paediatric operating theatres of Ain Shams University hospitals from May 2022 to November 2022.
The double blinded randomized clinical comparative trial was conducted on paediatric male patients, 3–12 years old, with ASA I and II scheduled for circumcision. The exclusion criteria were refusal by a patient’s guardian, contraindications to regional blocks, such as bleeding disorders and skin infections, drug hypersensitivity, and failure of achieving the block.
This study patients (total 81) were distributed into 3 groups, each consisting of 27 patients; group 1: DPNB group, group 2: CNB group, and group 3: combined DPNB and CNB blockade.
Postoperative pain was measured and recorded on the Wong-Baker FACES® Pain Rating Scale (Figure 1) at 1, 3, and 24 hours after surgery [10].
The Wong-Baker FACES® Pain Rating Scale (Figure 1) – showing a series of faces ranging from a happy face at 0, representing “no pain”, to a crying face at 10, representing “the worst pain imaginable”; using the faces and written descriptions, the patient selects the face that best describes his/her level of pain – was applied by the physician and then it was explained to the patient guardian (usually the mother) for 24 hrs. Postoperative monitoring, usually after discharge from the hospital, comprised contact by phone to assess the pain level experienced by the children.
All procedures were done by supervisors and experts. All regional anaesthetic blocks were done by an experienced consultant anaesthetist. The dorsal slit technique was used technique for circumcision of all cases, which were done under general anaesthesia.
Pre-operative: All patients were assessed by careful history taking, full body examination, and laboratory evaluation (CBC and coagulation profile).
Intra-operative: Conventional monitoring was started upon arrival to the operating theatre, including noninvasive blood pressure, electrocardiograph, and peripheral oxygen saturation (SPO2).
General anaesthesia was induced by sevoflurane in an oxygen mixed with air gas flow. After induction, a 22-gauge cannula was inserted intravenously. Spontaneous breathing was maintained through a selected laryngeal mask airway device, and inhaled sevoflurane was controlled at 0.8 to 1.0 MAC for anaesthesia maintenance.
BLOCK TECHNIQUES
Caudal blockade technique
The patient was positioned in the lateral decubitus position. The back was adequately sterilized using povidone iodine. The posterior superior iliac crests were determined, and a line was drawn between them forming the base of an equilateral triangle in which the sacral hiatus forms its apex as a dimple between the 2 palpated bony prominences (sacral cornua). The needle was inserted into the sacrum at a 45° angle and redirected when it reached the posterior surface of the sacrum – a subjectively felt loss of resistance indicates a piercing of sacrococcygeal ligament (SCL) [11] – after which the needle angle decrease to 30° with slight cephalad advancement. After the aspiration was negative for both cerebrospinal fluid and blood and a negative whoosh test via introduction of 2 mL of air while auscultating the thoracolumbar region with a stethoscope [12], local anaesthetic (bupivacaine 0.25% [0.5 mL kg–1]) was injected in 1 mL increments under haemodynamic monitoring.
Dorsal penile nerve block technique
Under aseptic technique, the penis was gently pulled caudally for the needle insertion on each side of the midline just distal to the inferior pubic ramus. Then the needle was moved forward and directed slightly medially and caudally until feeling a ‘pop’ after it passed via the Scarpa’s fascia. Bupivacaine 0.25% was administered as a local anaesthetic at the recommended dose (2 mL up to 3 years old with the addition of 1 mL for every 3 years up to a maximum of 6 mL) [13].
In the combined and DPNB groups, a subcutaneous local anaesthetic infiltration was performed at the ventral penoscrotal junction for blockade of the perineal nerve that carries sensation to the ventral surface of the glans penis [14]. Local anaes-thetic was delivered via a 25G needle.
Combined block
Caudal block was performed, then the patient was placed supine and DPNB was performed [14].
Bupivacaine toxic dose in paediatrics is 2 mg kg–1, and we did not exceed this dose in any of the groups, block especially the combined block.
There was an interval of about 15 minutes between giving the caudal or penile block and the start of surgery. If there was an increase in the patient’s blood pressure or heart rate of more than 20% compared to the basal readings at the start of the operation, the block was considered to have not worked adequately or failed, and in this situation paracetamol 20 mg/kg was given as an intraoperative rescue analgesia and the patient was excluded from the study.
Outcome measures
Primary outcome: Postoperative pain scoring using the Wong-Baker scale at 1, 3, and 24 hrs.
Secondary outcome: Intra-operative arterial blood pressures and pulse rate, and postoperative complications such as: nausea, vomiting, bradycardia, urinary retention, itching, and constipation.
Sample size
Based on a previous study from Gokalp and Onur [14], who reported an effect size of 0.4 comparing the Wong-Baker scale in the first and third hours between 3 groups using an omnibus one-way ANOVA, a sample size of 27 per each study group, and a total of 81 for 3 groups, were calculated to achieve 80% power for detection of the differences between the means <i>versus</i> the alternative of the equal means utilizing the F test with a level of significance of 0.05. The variation size in the means is represented by the effect size f = σm/σ, which is 0.4.
Statistical analysis
Data analysis was done using Statistical Package for Social Sciences (IBM SPSS) version 23. The expression of quantitative variables was done in the form of mean and standard deviation or range if parametric, and median and interquartile range (IQR) if non-parametric, while the qualitative variables were expressed in the form of number and percentage. The comparison of quantitative parametric data between the 3 studies groups was done by using a one-way ANOVA test. The comparisons of quantitative and non-parametric data between the 3 study groups were done by using the Kruskal-Wallis test. The comparison between any 2 study groups with quantitative data and non-parametric distribution was done by using the Mann-Whitney test. The intergroup comparison of qualitative data was done by using the chi-square test. The confidence interval was set to 95%, and the margin of accepted error was set to 5%. The p-value was considered significant if < 0.05, highly significant if < 0.01, and not significant if > 0.05.
RESULTS
Demographic data
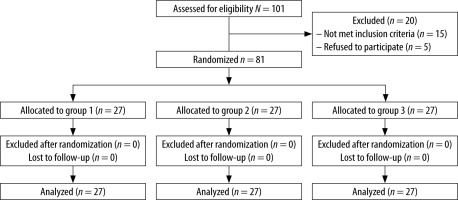
As shown in the flow chart of the study, a total of 81 patients were enrolled and analyzed in the study (Figure 2). There were no statistically significant differences between the 3 groups in terms of demographic data (Table 1).
TABLE 1
Comparison of the study groups regarding the demographic data
Intraoperative haemodynamics
There were no statistically significant differences found between the 3 studied groups regarding heart rate (HR), systolic blood pressure (SBP), diastolic blood pressure (DBP), and mean arterial pressure (MAP) intra-operative (Table 2).
TABLE 2
Comparison of the study groups as regard the HR, SBP, DBP, and MAP intra-operative
Postoperative Wong-Baker scale
These results show a highly significant diffe-rence between the 3 studied groups regarding the Wong-Baker scale postoperatively at 1 hour, 3 hours, and 24 hours with p-values < 0.001, < 0.001, and < 0.001, respectively (Figure 3). The Wong-Baker scale was significantly less in the CNB and the combined groups compared to the DPNB at 1, 3, and 24 hrs postoperatively (Table 3).
FIGURE 3
Comparison of the study groups regarding the Wong-Baker scale postoperatively at 1 hour, 3 hours, and 24 hours
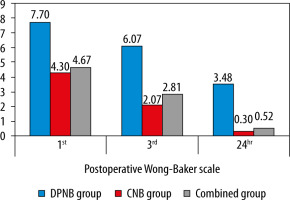
TABLE 3
Comparison of the study groups regarding the the Wong-Baker scale postoperatively
The following table compares the 2 groups regarding the Wong-Baker scale at 1, 3, and 24 hrs, postoperatively. It shows a significant difference between the DPNB and CNB group, and a highly significant difference between the DPNB and combined group, but with a non-significant difference between the CNB and combined group (Table 4).
TABLE 4
Post hoc analysis of Mann-Whitney test for comparing each of the 2 study groups regarding the Wong-Baker scale postope-ratively
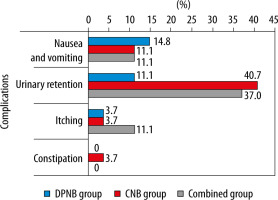
Postoperative complications (nausea, vomiting, urinary retention, itching, and constipation)
There was no statistically significant difference found between the 3 groups regarding the percentage of patients with complications, except for urinary retention, which showed a higher percentage in the CNB group and the combined group than in the DPN group, with a p-value of 0.034 (Figure 4, Table 5).
TABLE 5
Comparison of the study groups regarding postoperative complications
DISCUSSION
The current study was designed to compare the efficacy, duration of postoperative pain relief, and complications between 3 groups who underwent paediatric male circumcision, each one comprising 27 patients; group 1 received DPNB, group 2 received CNB, and group 3 received combined block.
Our results shows that there was no intergroup significant difference in age, weight, or height, with p-values of 0.068, 0.912, and 0.246, respectively.
On the other hand, our results show a significant difference between the 3 studied groups regarding the Wong-Baker scale postoperatively at 1 hour, 3 hours, and 24 hours, with p-values < 0.001, < 0.001, and < 0.001, respectively. The best results were found among the CNB patients (group 2) compared to the DPNB patients (group 1).
There was no significant difference between group 2 (CNB) group 3 (combined) regarding the Wong-Baker scale.
Al-Metwally et al. [15] compared caudal and penile block with respect to postoperative pain score, rescue analgesia time, and total analgesia dose. This study showed a significantly greater reduction in postoperative pain scores in the caudal group than in the penile group. The postoperative analgesia duration was significantly longer in the caudal group than in the penile group, with higher cumulative rescue analgesia consumption in the penile group than in the caudal group. These results agree with our study regarding Wong-Baker scale results and the superiority of CNB to DPNB.
Gokalp and Onur [14] showed that postoperative visual pain scores (VPS) recorded at the first and third hours after DPNB were significantly higher in comparison to caudal block but not significantly different on the second day. The VPS was significantly higher in the DPNB arm in comparison with the combined block. The analgesic requirement was higher in the DPNB groups. These results agree with our study regarding the Wong-Baker scale and the superiority of CNB to DPNB
Wang et al. [16] did not find a significant difference in heart rate or respiratory rate between the 2 groups. Furthermore, there were no significant differences in pain scores between the 2 groups when patients left the PACU. However, the time to first urination after surgery was shorter in the DPNB in comparison with the CNB group. In addition, patients of DPNB group requested analgesics later than those in the CNB group. The disadvantages of the caudal blockade, such as greater incidence of urinary retention, bilateral lower limb numbness, or even motor block, made penile dorsal nerve block a better option for analgesia of paediatric circumcision to avoid such side effects encountered in the CNB. These results disagree with our study as it favours the DPNB because of its higher post-op analgesia and fewer complications, while our study shows the opposite regarding post-op analgesia being significantly more effective with the CNB.
Haliloglu et al. [17] showed that pain scores in the very early postoperative period, such as after 30 minutes, were significantly lower with the CNB compared to DPNB. However, after 60 and 120 minutes the difference was insignificant between the 2 groups. These results differ from those of our study, which showed superiority of CNB regarding pain scores all along the first day post-operatively.
Bengisun et al. [21] observed that the proportion of patients who were free from postoperative pain for the first 6 hours was significantly higher in the caudal group. Also, the duration until first analgesic requirement was longer in the caudal group compared to the DPNB group. These results agree with our study confirming the superiority of CNB to DPNB.
In the study by Beyaz [18], the comparison of postoperative pain scores of the 2 studied groups showed no statistically significant difference in the time until the first postoperative analgesic requirement between the 2 groups. These results disagree with our study, which confirms the superiority of CNB regarding pain score postoperatively.
Patel et al. [19] showed that the pain scores were not significantly different between the caudal and dorsal penile block groups initially for the first 2 hours postoperatively, but on subsequent recordings a significant difference of pain scores was noted between the 2 groups, being significantly lower in the caudal group and the time to first analgesic requirement was significantly shorter in the DPNB group in comparison to the CNB group. These results agree with our study confirming the superiority of CNB to DPNB regarding postoperative pain control.
The results of the study by Bajwa et al. [20] showed a major deviation in heart rate with surgical incision for circumcision in the DPNB group in comparison to the CNB group, which showed a non-significant heart rate response to surgical incision. Also, in the CNB group the postoperative analgesia demand was negligible, with adequate postoperative pain control. Whereas in the DPNB group, postoperative analgesics were required as patients complained about pain and their parents were also unsatisfied. These results agree with our study, confirming the superiority of CNB to DPNB regarding pain control.
With regard to the postoperative complications, our results show that there was no intergroup statistically significant difference except for urinary retention showing higher percentage in the CNB group and the combined block group than the DPNB group.
These results agree with those obtained by Gokalp and Onur [14]. The most frequent complication was postoperative bleeding, which meant that 0.5% of patients needed reoperation, but there was no significant difference between the groups. In this study, the prolonged motor blockage was significantly higher in the caudal block arm compared with the combined block arm. These results agree with our study regarding complications.
Both Beyaz [18] and Haliloglu et al. [17] showed no caudal or penile block-related adverse events such as LA toxicity or oedema and haematoma at the block site. No patient developed postoperative motor block or urinary in either group. Only minor bleeding occurred with one patient after penile block was done, and it responded to compression without occurrence of significant haematoma. The same findings were also observed by Patel et al. [19].
The results of Wang et al. [16] showed that the CNB group was associated with a higher incidence of urinary retention, motor block, and postoperative bilateral lower limbs numbness, and Bengisun et al. [21] showed a delay in the time of first micturition in the CNB group compared to the DPNB group, but no child experienced urinary retention and there were no intergroup statistically significant differences for the incidence of postoperative adverse events in first 24 hours.
Limitations
This study has some limitations. New studies with larger samples are needed to investigate and reinforce the effect of DPNB and CNB on analgesia in children undergoing circumcision, and to include larger numbers of patients to recognize changes in the Wang-Baker scale between groups. In addition, studies with control groups are required for better support of the results and conclusions of the study data.
CONCLUSIONS
It can be concluded from the current study that both caudal and combined blockade were superior to DPNB alone for intraoperative and postoperative analgesia after circumcision. However, caudal block is associated with significantly higher incidence of urinary retention compared to the DPNB group. Also, there was no additional benefit as regards the analgesic efficacy of combining both blocks.