Lumbar spinal stenosis (LSS) is defined as a patho-logical process in which bony, ligamentous, and synovial elements of the lower axial spine degenerate and progressively overgrow, compressing, in turn, the neural and vascular elements in the spinal canal. This compression can either be asymptomatic or generate a combination of static back pain, radicular lower extremity pain, and/or neurogenic claudication [1].
The pathological mechanisms of lower limb symptoms caused by LSS involve nociceptive, inflammatory, and/or neuropathic pain components. It was demonstrated that patients with low back pain (LBP) and/or leg pain caused by LSS typically suffer from mixed pain. In particular, nociceptive pain, triggered by the pathology causing the stenosis such as arthrosis of the apophyseal facets, degenerative disc disease, spondylolisthesis, and contracture of paravertebral muscles, is predominant in the initial stages of the disease. Along with stenosis worsening, nociceptive pain combines with neuropathic pain due to the dysfunction of the medullary nerve structures [2], with characteristic symptoms manifested as paraesthesia (tingling, pricking, chilling, burning, numbness), hyperalgesia, feeling of heaviness, and cramps in lumbar and lower limbs [3]. On this basis, LSS represents a classic example of chronic benign mixed pain.
Commonly, LSS treatment is achieved through nonsurgical and surgical approaches. These strategies can be pharmacological, rehabilitative, beha-vioural, surgical, or by minimally invasive analgesic techniques adopted in monotherapy but mostly in combination, or in sequence, and involving different specialists including orthopaedists, physiatrists, pain therapists, and neurosurgeons. Interestingly, in the last 10 years, some guidelines and algorithms have been proposed to guide the most suitable treatment during the therapeutic path [4, 5]. For each of the proposed therapeutic options, however, the scientific evidence is not sufficient to indicate which is the gold standard. Many doubts mainly concern the management of the initial stages of the disease and the pharmacological approach to pain.
Usually, the therapeutic path begins with the use of drug therapy. It consists of non-steroidal anti-inflammatory drugs (NSAIDs) for addressing nociceptive pain and, subsequently, multimodal strategies, in the advanced stages featuring mixed, nociceptive plus neuropathic, pain. In these patients, the use of anticonvulsants or antidepressants can help to address the neuropathic pain component. Additionally, weak opioids, or low doses of strong opioids combined with acetaminophen, can help pain relief, also improving the patient’s quality of life (QoL) [6]. Nevertheless, several issues concern the use of opioids in non-chronic cancer pain. These issues can concern the lack of long-term efficacy – effective pain relief is not obtained despite doses being increased – the risk of abuse or misuse, and the risk of opioid-induced side effects such as constipation.
Because in degenerative diseases mixed pain represents a complex and painful issue encompassing different types of persistent chronic pain, a multimodal and patient-tailored approach seems to be a rational and effective strategy for addressing pain management [7]. According to the recommendations of the International Association for the Study of Pain (IASP), the ‘multimodal treatment is defined as the concurrent use of separate therapeutic interventions with different mechanisms of action within one discipline aimed at different pain mechanisms’ [8]. Thus, multimodal analgesia can be achieved by a combination of opioids, useful for attenuating the pain-related signals in the central nervous system (CNS), with NSAIDs that act mainly peripherally by inhibiting the initiation of pain signals. In this context, other strategies, such as the use of local anaesthetics and minimally invasive strategies, are useful. Moreover, multidisciplinary treatment is defined as ‘multimodal treatment provided by practitioners from different disciplines not necessarily communicating with each other’ [8]. On the other hand, as proposed by Gatchel et al. [9], multimodal treatment can also be provided by a multidisciplinary team collaborating in the assessment and treatment using a shared biopsychosocial model and objectives (interdisciplinary approach). In turn, the multidisciplinary/interdisciplinary combination of the expertise of various professional figures can improve the clinical result, preventing or managing in the best possible way all the problems related to the use of drugs and non-pharmacological strategies.
By using LSS as a model, this project is aimed at evaluating the main issues in the management of mixed non-cancer chronic pain, identifying in turn what an expert panel believes can be helpful to treat this type of pain, according to multimodal/multidisciplinary paradigms. Practical suggestions for pharmacological pain management are also offered.
METHODS
Study design
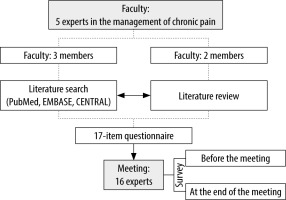
Three members (S.G., A.C., and P.D.M.) of a faculty composed of 2 orthopaedists (S.G. and G.S.), 1 neurosurgeon (P.D.M.), and 2 pain therapists (M.C. and A.C.) with expertise in the management of chronic pain (> 20 years of experience in the field) and engaged in scientific societies devoted to the study and the treatment of chronic painful diseases, conducted a literature search for the main issues in addressing mixed pain in LSS. They systematically searched PubMed/MEDLINE, EMBASE, and the Cochrane Central Register of Controlled Trials (CENTRAL). A strategy through precise MESH descriptors [‘Chronic Pain’, and the Entry Combination ‘therapy: Pain Management’] and the terms ‘mixed pain’ and ‘lumbar spinal stenosis’ was used for the search. The search string was: (“mixed”[All Fields] OR “mixes”[All Fields] OR “mixing”[All Fields] OR “mixings”[All Fields]) AND (“pain”[MeSH Terms] OR “pain”[All Fields]) AND (“lumbarised”[All Fields] OR “lumbarization”[All Fields] OR “lumbarized”[All Fields] OR “lumbars”[All Fields] OR “lumbosacral region”[MeSH Terms] OR (“lumbosacral”[All Fields] AND “region”[All Fields]) OR “lumbosacral region”[All Fields] OR “lumbar”[All Fields]) AND (“spinal stenosis”[MeSH Terms] OR (“spinal”[All Fields] AND “stenosis”[All Fields]) OR “spinal stenosis”[All Fields]). Additional records were searched through reference lists.
Subsequently, the other 2 members of the faculty (G.S. and M.C.) performed a revision of the papers. Primary studies of any design were included, and no restrictions on publication year were adopted. Papers were excluded if they did not fit into the conceptual framework of the study, i.e. focused on mixed chronic pain due to LSS. Furthermore, non-English language papers were excluded. The path followed a modified Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) strategy [10].
The analysis of the literature aimed at identifying the thematic areas useful for the development of a questionnaire elaborated by the whole expert panel. A consensus of at least 95% was established for each item.
Subsequently, 16 physicians participating in an expert opinion meeting on medical, surgical, and rehabilitative management in LSS were interviewed by means of a self-administered questionnaire. The experts were mainly employed at public facilities of the national health care system in the Campania region (Italy) and were all physicians (orthopaedists, physiatrists, and rheumatologists) and members of the National Association of Osteo-articular Specialists (ASON). They participated in previous analyses on pain management [11, 12]. The survey was administered before the beginning of the assembly, and all questions were discussed during the meeting. Subsequently, all participants filled in the questionnaire at the end of the activity. All responses remained anonymous, and no identifier was used to trace the participants on the survey. The flow chart of the study is reported in Figure 1.
RESULTS
The database search yielded 256 records. Fifty-seven records were identified through other sources. After removal of 235 duplicates, and exclusion of 52 non-pertinent records, 26 full-text articles were assessed for eligibility. Of those, another 10 papers were excluded and 13 articles were included in the qualitative synthesis for the tool development (Figure 2).
Based on the literature, 3 main thematic areas were identified: ‘diagnostic approach, counselling, and multidisciplinary approach’, ‘therapeutic approaches’, and ‘patient communication strategies’. A 17-item questionnaire was elaborated. The tool is shown in Table 1.
TABLE 1
Questionnaire on chronic pain management in lumbar spinal stenosis
Survey results
Diagnostic approach, counselling, and multidisciplinary approach
When asked about the therapy prescribed in the case of motor deficit not associated with other disorders, 8 (50%) physicians reported that they always prescribe “neuroprotective agents and analgesic therapy” and 8 (50%) reported “only kinesitherapy and neuroprotective agents”. After the discussion, the first option was chosen by 5 (31%) and the second by 11 (69%) clinicians. The option “muscle electrostimulations” was never selected in both cycles (Figure 3A).
FIGURE 3
Diagnostic approach, counselling, and multidisciplinary approach. Questions A–E. Note. Neurotropic agents include neuroprotective substances such as palmitoylethanolamide, and a-lipoic acid

The clinicians were then asked in which cases they preferred to have a consultation directly with the neurosurgeon. Before the course, 10 (63%) answered “in cases of particular severity of the anatomical-pathological picture”, 5 (31%) “in younger subjects”, and 1 (6%) “in cases where pain therapy is rarely effective”. After the course, all the subjects who selected “in younger subjects” changed their position, and a total of 13 (81%) answered “in cases of particular severity of the anatomical-pathological picture” and 3 (19%) “in cases where pain therapy is rarely effective” (Figure 3B).
Regarding the question “Do you perform a multidisciplinary approach involving a neurosurgeon for managing difficult-to-treat mixed pain?”, 8 (50%) stated that they usually contact the neurosurgeon to discuss the therapy, 5 (31%) preferred to let the neurosurgeon act independently, and 3 (19%) are not in contact with them. After the course, 9 (56%) were likely to contact the neurosurgeon, 1 (6%) preferred that the neurosurgeon acted independently, and 6 (38%) stated that they did not contact them (Figure 3C).
When asked if they were attentive to the chara-cteristics of the stenosis (e.g. laterolisthesis in scoliotic subjects) and if they informed the patient about possible therapeutic failures, 10 (63%) subjects answered positively, 5 (31%) considered that their experience was insufficient to address the issue, and 1 (6%) reported that they did not address the point even if they were aware of the therapeutic problems. After the discussion, 8 (50%) clinicians answered positively, and 8 (50%) considered that their experience was insufficient to address the issue (Figure 3D).
Regarding the conditions for which the intervention of the neurosurgeon is necessary, 10 (63%) clinicians reported that it depended on the characteristics of the stenosis regardless of the patient’s age, 5 (31%) in case of failure of any other therapy even in the elderly subject, and 1 (6%) in case of failure of any other therapy but only in younger subjects. After the course, the first option was chosen by 12 (75%) subjects and the second by 4 (25%) (Figure 3E).
Therapeutic approach
In response to the question “At what stage of pain therapy failure do you think you need a consultation from the pain therapist?”, 11 (69%) physicians answered “Only when I judge it can lead to a result” and 5 (31%) “Only if the patient shows acceptance of a further therapeutic procedure”. After the course, the first option was chosen by 9 (56%) subjects and the second increased to 7 (44%) answers. “Never” was not a selected option in both cycles (Figure 4F).
On the following question, “Before the consultation above, do you change the therapy and implement associations among pain relievers and other drugs?”, 1 (6%) physician answered: “Seldom”, 4 (25%) “Only in case of failure of opioid monotherapy”, and 11 (69%) “Always”. After the discussion, 5 (31%) reported that they implement associations “Only in case of failure of opioid monotherapy” and 11 (69%), again, “Always” (Figure 4G).
When asked “Do you prescribe maintenance therapy when a therapy brings good results?”, 10 (62.5%) physicians reported “to reduce the dose”, 4 (25%) “to suspend the therapy”, and 2 (13%) “to maintain the original posology after reaching the therapeutic goal”. After attending the course, a total of 9 (56%) participants modified their previous response in favour of therapy maintenance: 5 (31%) were likely to reduce the dose and 11 (69%) to maintain it after reaching the therapeutic goal. No physician chose the suspension at the end of the course. The reduction of the posology was intended to be carefully and continuously followed up to readjust the dose in case of relapse (Figure 4H).
Participants were then asked what were the most frequent pathologies for which they believe that opioid-based analgesic therapy is fundamental. Before the course, 10 (62%) opted for spinal stenosis with LBP and constant peripheral irradiation, 3 (19%) for spinal stenosis with prevalent chronic LBP, and another 3 (19%) for stenosis of the vertebral canal or lateral recesses with peripheral irradiation, as spinal claudication. After the discussion, the first option increased to 14 (88%) clinicians and the following 2 options decreased to 1 (6%) person each (Figure 4I).
On the analgesic therapy for long-term treatment (in cases of pathology that cannot be resolved with surgery, patient indisposition, pain persisting over 3 months), 11 (69%) physicians recommended opioids at a maintenance dose and analgesic therapy interventions if necessary, and 5 (31%) recommended opioids at maintenance dose. After the meeting, both options were selected by 8 (50%) participants in favour of the maintenance dose. “Periodic interventions with analgesic drugs without a pharmacological therapy” was not a selected option (Figure 4J).
When asked about a medication that could guarantee an acceptable tolerability for the patient and its dosage, 11 (69%) clinicians recommended oxycodone (5 mg) + acetaminophen 2 times/day, 4 (25%) oxycodone (5 mg)/naloxone 2 times/day, and 1 (6%) tapentadol (50 mg) 2 times/day. After the discussion, 14 (88%) physicians opted for the oxycodone-acetaminophen association, and 2 (13%) for the oxycodone-naloxone association (Figure 4K).
Regarding the usefulness of setting up maintenance pain relief therapy before the operation, 10 (62%) were always favourable, and 6 (38%) stated that it “depends on clinical considerations”. After the course, the first option increased to 15 (94%) clinicians, again in favour of opioid maintenance therapy. The option “No” was never selected (Figure 4L).
Clinicians were asked how much they agreed that it is necessary to set up an effective analgesic therapy in the pre-operative period to obtain a good postoperative outcome. Although before the meeting 11 (69%) participants considered the pre-operative analgesia very important, the number increased to 15 (94%) after the discussion. The remaining considered the procedure important only in selected cases. “Not very important” was not chosen (Figure 4M).
Patient communication strategies
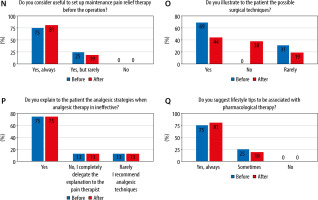
Twelve (75%) physicians confirmed that they were likely to explain to the patient the probable analgesic techniques they could receive. The other 4 (25%) stated that they “completely delegate the explanation to the pain therapist”. After the activity, 13 (81%) subjects chose the first option, and 3 (19%) the second. “I rarely recommend analgesic techniques” was never selected (Figure 5N).
When asked “Do you present and illustrate to the patient the possible surgical techniques indicated for their case?”, 11 (69%) clinicians declared that they present and illustrate the possible surgical techniques indicated for their case, and 5 (31%) declared that they seldom did it. Interestingly, after the discussion, 6 participants modified their answers – only 7 (44%) confirmed illustrating the possible surgical techniques, 3 (19%) seldom did, and 6 (38%) never did it; this option was not chosen previously (Figure 5O).
Twelve (75%) clinicians stated that they always explained to the patient that analgesic therapy cannot lead to the absence of pain, and thus it is necessary to consult a specialist to change the dose. Two (12.5%) declared seldom talking to the patients in this regard, and 2 (12.5%) declared never tackling the topic. The same results were obtained after the discussion (Figure 5P).
About two-third of participants (75%) recommended lifestyle tips in association with pharmacological therapy for pain relief whereas 4 (25%) addressed the point only if necessary. These percentages changed slightly after the debate – 13 (81%) were in agreement with the first option and 3 (19%) with the second. No expert selected “No” as an option (Figure 5Q).
DISCUSSION
Lumbar stenosis is a chronic pathology with a very variable clinical picture, being dependent on the severity of the pathology determined, and in turn by various factors including the age of the patient, number of levels involved, the extent of narrowing of the canal, or of the lateral foramina. Symptoms such as pain, paraesthesia, weakness of the lower limbs, and motor claudication can occur as isolated or associated and can dominate the clinical picture to a variable extent. Another important factor is the different evolutionary nature; some patients, in fact, remain for a long time with the same discomfort whereas others quickly experience a significant worsening of symptoms with a rapid deterioration of autonomy and QoL. From these considerations, the therapeutic approach cannot be univocal and often a multidisciplinary treatment, which includes pharmacological therapy, physiotherapy, rehabilitation, analgesic techniques, lifestyle modifications, and doctor-patient communication, must be undertaken before arriving at decompression surgery.
The analysis of the results of the questionnaires before and after the discussion shows that the therapeutic attitude of the individual specialist changes after comparison with experts with different competencies. The results of the study underline that the evaluation of symptoms is fundamental for defining the therapeutic strategy, and this is confirmed by the answers to the first question both in the first and in the second questionnaire; in the presence of pain alone, pharmacological therapy with neuroprotective agents such as the endogenous fatty acid amide palmitoylethanolamide, a-lipoic acid, and painkillers is indicated, although for 68% of participants it is considered effective even in the presence of only motor symptoms. In the literature, the anticonvulsants gabapentin/pregabalin, among the neuroprotective agents, and NSAIDs/opioids, among the painkillers, are the drugs with scientific evidence in the treatment of pain due to stenosis [4–6]. However, NSAIDs are effective only on nociceptive pain that characterizes the initial stages of the disease; on the other hand, opioids and pregabalin/gabapentin are more indicated in the advanced stages, characterized by neuropathic or mixed pain. Nevertheless, strategies for controlling and preventing the problem of opioid abuse, such as the early identification of high-risk patients, must always be considered.
The results of the second and fifth questions clarify when the intervention of the neurosurgeon is preferred. ‘In the entry questionnaire, 63% of the participants responded that this intervention was dictated by the severity of the pathological picture. On the other hand, in the exit questionnaire, the majority of the participants affirmed that the neurosurgeon intervention was conditioned by the patient’s age. Therefore, neither the failures of any other therapy nor the radiological aspects, but only the clinical pictures, lead to surgery. In particular, in less elderly subjects, an earlier surgery is recommended because the QoL is destined to worsen over time. While conservative management of LSS is often the preferred strategy, it was demonstrated that surgery is more effective when conservative approaches have failed for a period of up to 6 months [13].
The answers to the third question confirm that a multidisciplinary approach is a correct strategy. Of note, more than half of the participants are likely to contact the neurosurgeon or the pain therapist if they do not share their therapeutic attitude, while only 6% in the exit questionnaire, compared to 31% in the entry questionnaire, prefer that individual specialists act independently. The result is particularly comforting. Evidence suggests that the multi-professional strategy (especially when interdisciplinary) to chronic pain is the best strategy both in terms of cost-effectiveness and safety (less iatrogenic complications) [7, 14].
The answers to the fourth question show the diagnostic importance of the characteristics of the stenosis (50% search for them) but also the difficulty in finding them (50% do not search for them because they do not have sufficient experience); for example, often lateral stenosis, especially in scoliotic subjects, is confused with disc pathologies. According to Bagely et al. [1], the diagnosis of LSS can be a challenge. Again, a careful physical and neurological examination is necessary to refer the patient for imaging investigations (MRI, or CT with myelography if MRI is contraindicated). Among the clinical features, an evidence-based study demonstrated that the most sensitive clinical data concerns radiating leg pain that is aggravated while standing [15]. Clinical and imaging investigations can be combined with electrodiagnostic studies in those with an atypical presentation or inconclusive imaging.
From the answers to the sixth question, it appears that the pain therapist is always consulted in the case of failure of the analgesic therapy, but the motivation varies. Interestingly, just over half of the participants (56%) recognize them as having greater expertise, and 44% of the experts usually consult a pain therapist only in the case of conservative therapy. This attitude reflects lesser experience of the orthopaedist and physiatrist in the use of opioids, especially in managing higher dosages and side effects, and, on the other hand, the possibility of referring the patient to the pain therapist to undergo minimally invasive techniques such as epidural injections or neuromodulation. This is interesting data because most patients who suffer from chronic pain are not treated by a pain therapy specialist, and in about 40% adequate pain management is not provided [16]. Thus, more effective collaboration between the various professional figures would be desirable.
The seventh question clarified the timing of the recourse to the pain therapist after the failure of the analgesic therapy. Sixty-nine per cent of the participants in both questionnaires turned to the pain therapist after having varied the initial opioid therapy without success, while 31% turned to the pain therapist immediately if the initial opioid therapy had failed. In this case, seeking help from the pain specialist is motivated by the greater know-how that the pain specialist is recognized to have in the use of opioids.
The eighth question refers to the duration and posology of pharmacological treatment with opioids after the improvement of symptoms. The suspension of the therapy, which in the entry questionnaire was preferred by 25% of the participants, is zeroed in the exit questionnaire where all the participants were in favour of continuing the therapy. During the discussion among the participants, awareness on the safety of opioid treatment over time was raised and it led to a reversal of the trend as the choice to maintain the same posology went from 13% to 69%, while the choice to reduce the posology was approximately halved.
The ninth question confirms the use of opioids as the first-choice treatment for the management of LSS clinically characterized by LBP and constant peripheral irradiations (88% of the participants in the exit questionnaire compared to 62% of the participants in the entry questionnaire). The use of opioids for painful long-term non-cancer conditions such as osteoarthritis must be carried out with particular care. However, in this question, respondents were not asked to choose the most suitable pharmacological or non-pharmacological approach but instead to indicate under which circumstances the use of opioids was deemed most effective. In other words, although non-pharmacological strategies need to be strengthened and in chronic non-cancer pain opioids should be used with extreme caution, in the context of clinical conditions associated with LSS, respondents underlined that the use of opioids may be taken into account in more complex situations. This is an example of a strategy that follows a case-by-case analysis approach.
According to the answers to the tenth question, all participants were in favour of the use of opioids as a long-term maintenance therapy even for patients for whom surgery is indicated but who cannot undergo surgery for various reasons. Although it is not possible to have complete remission of the symptoms in the case of advanced stages of stenosis, the symptoms can be at least attenuated. This a further example in which the use of opioids, providing a careful analysis of the case, can lead to significant benefit for the patient.
The preferences in the choice of opioids are illustrated in the answers to the eleventh question. This question is focused on the use of an opioid alone (tapentadol), or an opioid (oxycodone) used in combination with a non-opioid analgesic (paracetamol) or with orally administered naloxone, which, due to significant first-pass effect, has limited systemic effects and hence selectively antagonizes the gastrointestinal effects of opioids [17]. We used these options because, according to the National Observatory on the Use of Medicines, oxycodone in combination and tapentadol are among the most prescribed drugs in this clinical setting [18]. Moreover, in Italy, the combinations opioid plus non-opioid analgesic, and opioid agonist plus opioid antagonist are commercially available in fixed doses.
Probably, because the respondents were not specialists in pain medicine, they were more likely to use a combination of drugs that could lead to a rapid effect (rapid-release oxycodone and acetaminophen) rather than referring to drugs with a longer half-life and, therefore, to manage a pharmacological program that must presuppose in-depth knowledge of pharmacokinetics and pharmacodynamics. Again, the pharmacokinetic characteristics of the rapid-release oxycodone and acetaminophen combination can make its use particularly suitable for pain from lumbar stenosis, which is by its nature chronic with exacerbations while standing and walking [19]. Nevertheless, it must be underlined that although acetaminophen is widely used for analgesia in osteoarthritis, low efficacy is reported and its efficacy in this setting is questioned [20]. Moreover, a Cochrane analysis found that there was very limited evidence that oxycodone may provide moderate benefit (equivalent to a 30% reduction in pain) against painful diabetic neuropathy or postherpetic neuralgia, and there was no evidence of other neuropathic pain conditions [21]. These data must be taken into consideration in the choice of pharmacological therapeutic options.
The answers to the twelfth and thirteenth questions show that pain relief therapy is very important even in cases undergoing surgery to obtain a good post-operative result. Patients who maintain enough independence to walk and consequently a good muscular tone up to the time of surgery can recover before and better after the operation. In this context, pain treatment is encompassed among the useful modalities of a multidisciplinary “prehab” protocol prior to surgery. The effectiveness of this approach has been amply demonstrated [22].
The fourteenth question is the first of the questions related to communication strategies between the clinician and patient. Most of the participants explain directly to the patients the analgesic techniques they can undergo, such as neuromodulation or epidural infiltrations, before referring them to the pain therapist for execution. This behaviour is correct because it marks the end of the pharmacological therapy with results below expectations and makes the patient aware of the need to associate a minimally invasive treatment before a possible surgical decision.
The answers to the fifteenth question are apparently contradictory. In the entry questionnaire, 69% of the participants indicate to the patient the most suitable surgical technique for their case, 31% do it only rarely, and none of them claimed never to do this. After the discussion, the former fell to 44% and the third increased to 38%. The explanation probably lies in the discussion with the neurosurgeon, who explained that there are many techniques in constant evolution including traditional decompression by unilateral or bilateral laminectomy, laminotomy, laminoplasty, arthrodesis, interspinous spacers, and minimally invasive lumbar compression. Each technique has strengths, weaknesses, and precise indications of the type and severity of the stenosis, parameters that only the operator can evaluate.
The sixteenth and seventeenth questions also concern communication strategies. The answers to the sixteenth question confirm, in both the initial and final questionnaires, that 75% of the participants usually explain to the patient at the beginning that opioid therapy cannot lead to the disappearance of pain and that it requires adjustments during therapy. Constructive patient-clinician communication is a crucial element of valid pain management, also in the setting of non-cancer pain [23]. The answers to the seventeenth question show the importance of associating changes in lifestyle with pharmacological therapy. These data confirm what has emerged from many recent studies – it was amply demonstrated that lifestyle interventions (e.g. nutritional interventions) can improve QoL and outcomes in patients affected by chronic painful conditions [24].
LIMITATIONS
This study has several limitations. The main limitation concerns the use of a non-validated questionnaire. However, we built the tool through a systematic review of the literature, and once the topics were identified, the greatest possible consensus was achieved. Another important limitation is the sample size. Although this gap does not allow statistically valid conclusions to be reported, we aimed to offer an overview of the subject as well as suggestions for further research.
Members of other departments such as physiotherapists and psychologists did not participate in this study. Probably, this lack represents a major limitation because only results from a physician-centred point of view are presented. Additionally, the absence of patients’ perspectives is an important limitation. Nevertheless, this investigation was not intended as a guideline or a consensus. The survey focused on members of the association who usually manage chronic non-cancer pain and who had already participated in analyses on similar issues.
CLINICAL PERSPECTIVES AND PRACTICAL SUGGESTIONS
From this investigation, some shared concepts of extreme practical usefulness originated. In most cases, specialists adopt a conservative initial approach; it is usually based on physical therapy, lifestyle modifications, and drug treatment. When pharmacological strategies are planned, NSAID therapy can be useful in the initial stages of the disease where nociceptive pain dominates the clinical picture. Nevertheless, as a monotherapy, NSAIDs are insufficient when facing advanced stages featuring mixed pain that is often combined with functional limitations such as claudication. In these phases, it can be advisable to use opioids associated or not with adjuvants such as pregabalin/gabapentin or muscle relaxants. Patient characteristics, type of pain, and comorbidities will guide the most appropriate choice between weak opioids, such as codeine or tramadol, and strong opioids, such as buprenorphine, tapentadol, and transdermal fentanyl. In the context of multimodal analgesia, drug associations play a key role. Among opioids, the oxycodone/paracetamol combination can offer several clinical advantages because it acts on the different components of pain: nociceptive component through oxycodone and paracetamol, neuropathic component through oxycodone, and bone component through paracetamol. On the other hand, of great concern is the use of opioids in non-cancer chronic pain. The opioid crisis is a serious phenomenon, although with different epidemiology in different geographical areas, i.e. there is a greater impact in the United States and Canada than in Europe [25]. Moreover, the certainties in the treatment of cancer pain do not apply to other types of chronic pain. For instance, the WHO analgesic ladder seems not to be appropriate for addressing non-cancer chronic pain [26]. As a practical suggestion, it should be emphasized that the opioid prescription must be carried out after a careful case-by-case analysis. The multidisciplinary approach is fundamental to optimize the treatment and to combine it with non-pharmacological approaches, pending or not pending surgery. Although these non-pharmacological approaches can be useful in reducing the requirement of opioids, to date it is not clear which combination is most effective in limiting opioid use and offering clinical benefits [27]. On the other hand, the demonization of opioids may deprive patients of a valid therapeutic alternative. As stated by Dassieu et al. [28], restrictive prescription strategies provided in response to the prescription opioid crisis may have consequences similar to prohibitionist policies, amplifying in turn overdose risks. Consequently, before opioid prescription clinicians must focus on basic concepts such as the expected duration of treatment and the rules that must be imposed to limit the rate of dose escalation. The goals and the limitations of opioid therapy must be explained to the patient, including the possibility of adjusting the therapy over time and counteracting the side effects during the therapeutic process. Again, a careful analysis aimed at assessing the patient’s risk of addiction would be desirable [29].
Further suggestions are diagnostic and refer to the surgical indication. While the severity of the anatomic and radiographic picture of the stenosis must be evaluated, it is not the main indication for surgery because it is not always correlated to the severity of the symptoms. However, the age factor plays an important role in the decision-making process because in less elderly patients the surgical option must be considered earlier due to the speed at which symptoms worsen. Even in the case of a surgical decision, opioid therapy must be continued until the time of surgery because maintaining the patient with sufficient walking autonomy and an acceptable muscular tone of the lower limbs guarantees a good postoperative outcome.
Finally, the future perspective of expanding the multidisciplinary approach by inputs from the psychologists, physiotherapists, and patients should be seriously considered.
CONCLUSIONS
Lumbar stenosis is a chronic pathological condition that is often disabling in elderly people. In this survey, this condition was chosen as a model for discussing therapeutic orientations in patients affected by mixed pain. Despite limitations, the results confirmed that the therapeutic approach must be multidisciplinary, involving the orthopaedist, the physiatrist, the pain therapist, and the neurosurgeon. The analysis of the results of the questionnaires before and after the discussion shows that the therapeutic attitude of the individual specialist changes after discussion among experts. Thus, the interaction between the pain therapist and neurosurgeon is always desirable even if their opinions do not agree. Regarding pharmacological approaches, the use of opioids in non-cancer chronic pain must follow a careful case-by-case analysis, and clinicians must focus on basic concepts such as the expected duration of treatment and the rules that must be imposed to limit the rate of dose escalation. Again, the patient’s lifestyle must be modified according to the type and severity of the lesion. Finally, doctor-patient communication is essential to ensure adherence to therapy.