Dear Editor,
Advanced intraoperative neuromo-nitoring in anaesthesia is a common practice these days [1]. This includes monitoring of intracranial pressure, brain oxygenation, metabolism, and evoked potentials. The role of monitoring brain oxygenation in sitting position has been described in a series of patients undergoing non-neurosurgical surgery in beach chair position [2]. The decrease in blood pressure in the upright posture under anaesthesia may account for episodes of silent cerebral desaturation that can be reliably detected by cerebral oximetry. Jugular venous oximetry is a sensitive monitor for the detection of global cerebral ischaemia, against which other cerebral oximetry techniques are often compared [3]. However, what made us contemplate its role in neurosurgical cases being operated in a sitting position is the superadded maximal neck flexion done for the infratentorial supra-cerebellar approach to intracranial tumours. There is always an unwarranted possibility of impaired cerebral venous drainage along with cephalad migration of the oximetry catheter tip during positioning of the patient. Written informed consent was obtained from the patient for study and for publication of this case report.
A 34-year-old female, ASA 1, was scheduled for excision of a pineal region tumour by supra-cerebellar infratentorial approach in sitting position in January 2022. After induction and maintenance of anaesthesia in a standard manner, a catheter was placed, under ultrasound guidance, retrogradely through internal jugular vein into the jugular bulb for cerebral venous oximetry. The position was confirmed on X-ray, and maximal neck flexion was not seen to alter the position of the tip, which remained at the lower border of the C1 vertebra (Figure 1). The free aspiration of blood from all the ports was confirmed after final positioning, and the cathe-ter was secured in place. A central venous catheter (7F) was inserted in the right subclavian vein. The baseline value of jugular saturation was 72% at a fraction of inspired oxygen of 0.4, partial pressure of carbon dioxide of 37 mmHg, mean arterial pressure (MAP) of 98 mmHg, with end-tidal concentration of sevoflurane as 0.9%. After preloading the patient with 500 ml crystalloid and use of compression stockings in the lower limbs, the jugular bulb pressure (JBP) was 6 mmHg in a supine position with the head in a neutral position, while in the final sitting position it reduced to sub-atmospheric pressure (–1 mmHg). After placing the patient in a sitting position, the MAP decreased to 56 mmHg, and jugular venous oxygen saturation (SjVO2) decreased by 4%. Low-dose noradrenaline was started to keep MAP above 60 mmHg. During the rest of the surgery, SjVO2 remained between 62% and 72% and the highest JBP recorded was 1 mmHg. There were no clinical signs of intra-operative venous air embolism (VAE) or any resistance to aspiration suggesting kinking/cranial migration of the tip. The duration of anaesthesia was 7 hours, and the patient’s trachea was extubated at the end of surgery.
FIGURE 1
Lateral roentgenogram with white arrow depicting tip of jugular catheter at lower border of C1 vertebra: A) with head in neutral position, B) with maximal head flexion
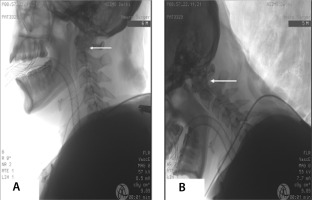
Insertion of jugular venous catheter not only helps to monitor cerebral oxygenation but can also aid in assessment of cerebral venous congestion. On maximal head flexion, the position of the catheter tip did not change in our patient. There was free aspiration of blood (no evidence of kinking) and no signs of compromised cerebral venous drainage (as shown by JBP). In addition to the cerebral oxygenation, estimation of JBP plays an important role in neurosurgical cases. Wang et al. [3] studied the influence of operative position and head flexion/rotation on JBP in 26 patients, which was taken as a surrogate of intracranial pressure. The JBP was found to be significantly increased when head was rotated 45° to the right side. The frequency and severity of VAE was greater in patients with negative JBP, suggesting it to be a fair predictor for risk estimation of VAE [4, 5]. However, the authors used a 14G intravenous catheter for SjVO2, and location of tip of catheter was not confirmed by X-ray, leaving us to speculate whether neck flexion leads to migration of the tip, causing it to abut the base of skull or vessel wall. Hence, we confirmed the position of the catheter tip using X-ray after insertion, as well as after neck flexion, to see the exact location of catheter tip in the jugular bulb.
To conclude, our case shows the feasibility of measurement of cerebral oxygenation and jugular bulb pressure even with maximal neck flexion during sitting craniotomy. The position of the catheter tip did not change with flexion of the neck. Moreover, JBP measurement is an important technique to assess venous pressure, especially in neurosurgical cases, that can aid in optimum head positioning. The insertion of the catheter did not compromise the cerebral venous outflow.




