Paravertebral block (PVB) is generally used in breast cancer surgery in combination with general anesthesia [1]. In a single injection PVB, 15 to 25 mL of local anesthetic (LA) is injected, whereas, in a multi-injection PVB, 3.0 to 6.0 mL of LA is used for each nerve being blocked [2, 3]. Marhofer et al. [4] found that in 40% of PVBs, LA distributed beyond the paravertebral space: epidurally, paravertebrally, and to the contralateral side.
We associate a number of undesirable effects in PVB (systemic toxicity of LA, hypotension, or block failure) with the use of large LA volumes and unpredictable pattern of its distribution from the injection site.
Only multi-injection PVB can decrease the volume of LA while maintaining the efficacy of the block. The use of low LA volumes in PVB prevents its undesirable distribution from the injection site. The risk of systemic toxicity will also be reduced.
The objective of this study was to compare the effects of multi-injection paravertebral block plus general anesthesia (GA) versus GA alone for radical mastectomy in breast cancer patients.
The primary outcome was fentanyl consumption. The secondary outcomes were perioperative venous cortisol levels, Visual Analogue Score (VAS) pain scores after the surgery, and the need for additional analgesia in the post-operative period.
METHODS
The study was approved by the Ethics Committee. Each patient gave written informed consent to be enrolled in the study and to undergo anesthesia. All patients required breast cancer surgery (radical mastectomy).
Inclusion criteria were female sex, aged 18 years and more, and stage I to III breast cancer. Exclusion criteria were severe hepatic and renal dysfunctions, endocrine diseases, hormonal therapy, and stage IV breast cancer.
This prospective randomized study included 130 women scheduled for radical mastectomy. Using a random number generator, the patients were randomized to two groups: Group 1 (n = 65) received GA, whereas Group 2 (n = 65) received PVB (Th1 to Th6) with GA.
All patients received premedication as follows: 7.5 mg of zopiclone orally the day before the surgery, as well as 0.5 mg of atropine and 10 mg of diphenhydramine intramuscularly 30 minutes before the surgery. Upon admission to the operating room, a peripheral venous catheter was inserted, and a monitoring system attached. Group 2 patients received PVB while sitting on the operating table. In the aseptic setting, skin and subcutaneous tissue were infiltrated with 6 to 8 mL of 1% lidocaine solution, 2.5 cm more laterally from the spinous processes of the vertebrae (Th1 to Th6) on the side of the surgery; in some patients, 10% lidocaine spray was used.
Under the out-of-plane ultrasound guidance using HITACHI EUB-405 (Hitachi Medical Corporation, Tokyo, Japan) with a 7.5 MHz linear probe, an injection needle was inserted into the paravertebral space at the desired level. 90 mm long 22–23 G Quincke needles (Greatcare Medical Instruments Co., Ltd., Ningbo, China) were used. Once the needle tip was positioned between the costal-transverse ligament and the parietal pleura, LA was injected (Figure 1).
Following aspiration, 0.5 mL of 0.75% ropivacaine solution was injected with ultrasound monitoring of LA distribution. Then, upon repeated aspiration, 0.75% ropivacaine solution was additionally injected to a total of 1.5 to 3.0 mL per spinal nerve at levels Th1 to Th6. A total of six ultrasound-guided single injections were performed. The median PVB time from the first injection to the application of aseptic dressing was 15 (10; 15) minutes.
Patients in both groups received GA as follows: pre-oxygenation with 100% oxygen for 3 minutes, 0.1 mg of fentanyl and 2.5 mg of droperidol intravenously, followed by thiopental or propofol in 2 to 3 minutes.
Muscle relaxation for tracheal intubation was achieved using intravenous suxamethonium or atracurium (in patients scoring not higher than 2 points in the intubation difficulty score).
ALV (artificial lung ventilation) was carried out as volume-controlled ventilation (semi-closed system) using premixed oxygen and nitrous oxide (1 : 1) and isoflurane. Isoflurane concentration was adjusted based on hemodynamic parameters. Intraoperatively, mean BP (blood pressure) and heart rate were maintained within ± 20% of preoperative baseline.
Intra-operative analgesia in Group 1 and Group 2 was achieved by fentanyl bolus injections, and paravertebral block supplemented (where necessary) with fentanyl bolus injections, respectively.
Fentanyl boluses of 1.0 to 1.5 μg kg-1 were given if the heart rate or the mean BP increased by more than 20% of the preoperative baseline.
Muscle relaxation was maintained with atracurium bolus injections.
During the anesthesia, continuous monitoring was performed according to the national anesthesia protocols. The resulting data were recorded in the “Anesthesia Record” chart at 5-minute intervals.
In 80 randomly selected patients from both groups, serum cortisol levels were monitored. The assay was carried out by enzyme-linked immunosorbent assay (ELISA) using an ELx800 microplate reader (BioTek Instruments, Inc., Winooski, VT, USA). The reference value for the reagent kits used was 378 nmol L-1 (150–660 nmol L-1).
Blood was sampled for laboratory testing at four stages: stage 1 – admission to the operating room, stage 2 – 30 minutes after the start of the surgery, stage 3 – 2 hours after surgery, and stage 4 – 20–24 hours after surgery.
After surgery, patients received intramuscular ketorolac at 30 mg every 8 hours for analgesia. In persistent pain, 2.0 mL of 5% tramadol solution or 1.0 mL of 1% trimeperidine solution was used at the patient’s request.
Also, in the post-operative period, the acute pain perception was measured using a 100-point linear VAS. The acute pain was measured 2, 6, 12, 24, 48 and 72 hours after surgery.
Based on initial data on intra-operative fentanyl dose, we calculated the minimum sample size required to deem the differences between the groups significant. The minimum sample size was 14 patients per group. The accepted significance level is 5%, and the power is 80%. The clinically significant difference between the group means for fentanyl dose was determined as 1.88 μg kg-1, and the total SD was 1.72.
Statistical analysis was performed using Stat-Plus Pro version 6 (AnalystSoft, Walnut, CA, USA) and Libre-Office 5.0 (Free Software Foundation, libre-office.org). To evaluate the normality of distribution, the ShapiroWilk test was used. For non-normal distribution, the median and the first and third quartiles were calculated. To compare independent groups, the Mann-Whitney U test (two groups) was used. To compare two related groups, the Wilcoxon test was used. When comparing categorical data, Pearson’s χ2 test was used. If the number of expected frequencies was less than five, the two-sided Fisher’s exact test was performed. The differences between the groups were considered statistically significant at P < 0.05.
RESULTS
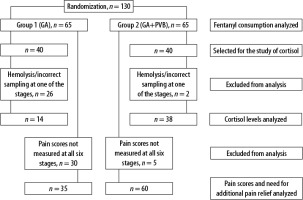
The study flow diagram is shown in Figure 2.
Results are presented as median and first quartile; third quartile (quartiles in brackets). The range of patients’ age was 33-89 years, with a median age of 62.0 (54.3; 68.6) years. The body mass was 79.5 (68.6; 88.0) kg, the height was 160.0 (156.1; 164.0) cm, and the body mass index (BMI) was 30.1 (26.9; 35.1) kg m–2.
No statistically significant differences were observed between the two groups in terms of age, body weight, height, BMI, the extent of surgery, the side of the surgery, and the American Society of Anesthesiologists physical status classification (P > 0.05). For baseline characteristics of individual groups, see Table 1.
TABLE 1
Patient characteristics in Groups 1 and 2
All patients underwent successful radical mastectomies. No complications of anesthesia were reported. Post-operative chest X-rays were performed in all PVBs. Pneumothorax was ruled out.
The duration of the surgery was 60 (35.0; 70.0) min and 65.0 (55.0; 80.0) min in Group 1 and Group 2, respectively; no significant difference between the groups was found (P > 0.05).
The total fentanyl dose was 4.17 (3.33; 5.56) μg kg-1 and 2.50 (1.85; 3.39) μg kg-1 in Group 1 and Group 2, respectively. Fentanyl dose in Group 1 was 1.7 times that in Group 2 (P < 0.05). Thiopental dose was 5.88 (4.95; 6.50) mg kg-1 and 5.32 (4.81; 5.88) mg kg-1 in Group 1 and Group 2, respectively (P > 0.05). The propofol dose was 2.31 (1.99; 2.61) mg kg-1.
Suxamethonium dose was 1.92 (1.69; 2.09) mg kg-1 and 1.72 (1.61; 1.87) mg kg-1 in Group 1 and Group 2, respectively (P < 0.05).
At the maintenance stage, isoflurane concentration was 1.0 (0.8; 1.0) %vol and 0.8 (0.8; 0.8) %vol in Group 1 and Group 2, respectively; the difference was statistically significant (P < 0.05).
The atracurium dose was 0.52 (0.39; 0.65) mg kg-1 and 0.57 (0.51; 0.63) mg kg-1 in Group 1 and Group 2, respectively (P > 0.05).
The time to extubation was 15 (10; 25) min and 10 (5; 15) min in Group 1 and Group 2, respectively; the difference was statistically significant (P < 0.05).
In 28 patients, cortisol was not detected at all four stages (Stage 1 – admission to the operating room, Stage 2 – 30 minutes after the start of the surgery, Stage 3 – 2 hours after surgery, and Stage 4 – 20–24 hours after surgery) because there was hemolysis or incorrect sampling. Samples from 52 patients were determined at all four stages and were finally analyzed.
In both groups, significant differences in cortisol levels between Stage 3 and all other stages were seen (P < 0.05). No differences in cortisol levels were found between Stages 1, 2, and 4 (P > 0.05).
No differences in perioperative peripheral venous cortisol levels were detected between the groups at Stages 1, 2, and 4 (P > 0.05). At Stage 3 (2 hours after surgery), the differences were statistically significant (P < 0.05).
Cortisol levels at Stage 3 were 3.3 times and 2.7 times higher than the baseline (at Stage 1) in Group 1 and Group 2, respectively. For cortisol levels measured in Groups 1 and 2, see Table 2.
TABLE 2
Cortisol levels over time in Groups 1 and 2*
Acute pain was measured 2, 6, 12, 24, 48 and 72 hours after surgery. In 35 patients, the acute pain score for VAS was not measured at all six stages after surgery. The results of acute pain assessment in these 35 patients were excluded from the analysis. Acute pain scores of 95 patients were determined at all six stages and were analyzed. 35 (54%) and 60 (92%) patients in Group 1 (GA) and Group 2 (GA + PVB) were interviewed.
Data analysis has shown significantly lower VAS scores in Group 2 at 2, 6, 12, and 48 hours after surgery (P < 0.05). At 24 and 72 hours after surgery, no significant differences in pain scores were seen between the groups (P > 0.05).
For acute pain scores (VAS), see Table 3.
TABLE 3
Post-operative VAS scores in Groups 1 and 2
For post-operative VAS scores over time and maximum VAS scores, see Figure 3.
FIGURE 3
Comparison of VAS scores between groups with different anesthesia methods. Me (first quartile; third quartile), max and min

Given that the highest VAS pain scores were seen on the first post-operative day, post-operative analgesia was analyzed in these women.
In Groups 1 and 2, in the first 24 hours after surgery, analgesia was not required for 14.3% and 54.3% of patients, respectively. Opioid use was needed in Group 1 for 40.0% of patients, in Group 2 for 7.1%. NSAIDs for pain relief were used in 45.7% and 38.6% of cases in Groups 1 and 2, respectively. The revealed differences between the groups were statistically significant (P < 0.05).
In both groups, the highest acute pain scores were seen on the first day after mastectomy. They were significantly higher in women without PVB.
DISCUSSION
In a number of publications, the use of regional anesthesia as one of the components of anesthetic management was noted to decrease the need for narcotic analgesics and inhalation anesthetics during surgery [5, 6]. This study also found a decrease in fentanyl consumption during radical mastectomy under GA with PVB.
The pattern of LA distribution in the paravertebral space is often unpredictable [7, 8]. The number of nerves being blocked when using large LA volumes cannot be predetermined. Even though there are numerous articles on cortisol levels in various procedures, few publications provide data on its levels in radical mastectomy over time. For example, a meta-analysis by Prete et al. [9] found that during the first 24 hours after moderate surgery (Johns Hopkins surgical severity criteria), the cortisol levels could be four times higher than those of healthy people. Additionally, with regional anesthesia, the increase in cortisol levels was on average 17% lower as compared to GA alone.
Bakr et al. [10] observed that in radical mastectomy, the baseline cortisol level was 17.00 ± 3.70 μg dL-1 (~ 469.2 nmol L-1), and 40 minutes after the start of the surgery, it significantly increased to 26.40 ± 1.96 μg dL-1 (~ 728.64 nmol L-1); at 24 hours after surgery, cortisol levels showed no significant difference from the baseline. However, in our study, there was no significant increase in cortisol levels 30 minutes after the start of surgery.
Contrary to the abundant evidence on cortisol level dynamics, in this study, there was no intraope-rative increase in cortisol levels during the radical mastectomy with either of the anesthetic techniques used.
The study shows that cortisol levels may be used as a marker of sufficient intra-operative analgesia. With sufficient analgesia, intra-operative cortisol levels do not increase. The methods of anesthesia applied ensured adequate protection from pain during surgery in both groups. At 2 hours after surgery, a smaller increase in cortisol levels is seen with PVB, which indicates a persistent analgesic effect of the block.
The pain score on the first day after radical mastectomy (using a numeric rating scale, 0–10) averaged 3.8 points [11]. The use of PVB with GA improves the quality of pain relief after a radical mastectomy. This improvement is indicated by a decrease both in acute pain scores and in the need for narcotic analgesics [6, 12]. Qian et al. [12] also note that PVB reduces the pain intensity in the early post-operative period and reduces the incidence of chronic pain at 3 and 6 months after a radical mastectomy. Björnsson et al. [13] found that with PVB, VAS pain scores did not exceed 20 points within 72 hours after a radical mastectomy. Our data confirm that the use of multi-injection PVB in combination with GA reduces the acute pain scores on the first day after a radical mastectomy. In our study, the highest median VAS pain score within 24 hours after mastectomy were 5 points and 22 points with and without PVB, respectively.
CONCLUSIONS
Supplementation of GA with multilevel PVB decreased the intra-operative fentanyl consumption. In radical mastectomy with GA and GA with PVB, the intra-operative cortisol levels do not increase. At 2 hours after surgery, a significantly smaller increase in cortisol levels was found in PVB patients versus patients without PVB. The highest VAS pain scores were seen within the first 24 hours after mastectomy. The use of PVB improves the quality of anal-gesia on the first day after a radical mastectomy.