Dear Editor,
Preoxygenation is an essential procedure to prolong the safe apnoea time before tracheal intubation [1]. High-inspired oxygen fraction (FiO2) in the gas flow replaces the residual nitrogen in the pulmonary alveoli and fills the functional residual capacity with oxygen [2]. More than 90% of the end-tidal oxygen concentration (ETO2) minimizes the risk of hypoxia during intubation [3]. In healthy adult patients, preoxygenation can extend the safe apnoea time to up to 8 minutes [4]. Preoxygenation is particularly crucial in critically ill patients who do not have any physiological reserves with a high risk of immediate desaturation [5]. Studies such as those conducted by Farmery et al. [6] have demonstrated that this patient demographic can desaturate to as low as 85% within 23 seconds of apnoea.
Given the myriad physiological challenges such as reduced cardiac output, anaemia, acidosis, severe hypo-tension, and the frequent occurrences of shunts due to conditions like pulmonary oedema or pneumonia, all intubations within intensive care settings should be considered as a high-risk procedure. These factors exponentially elevate the metabolic demand and risk of cardiopulmonary collapse during tracheal intubation, contributing to a higher incidence of cardiac arrest compared to procedures conducted within the operating theatre [6, 7]. In a retrospective review, Mort et al. [8] described a 2% incidence of cardiac arrest during emergency intubations outside of the operating theatre, a risk 100-fold higher than that associated with intubations conducted within it.
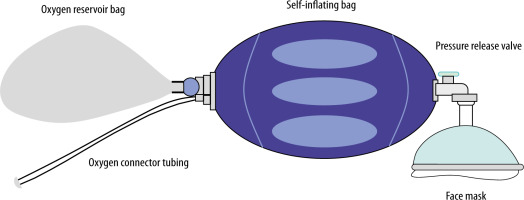
Commonly utilised outside of the operating room, self-inflating bag valve masks (BVMs) serve as a critical tool for manual ventilation in prehospital settings and during cardiopulmonary resuscitation [2, 9]. The components of a BVM include a self-expanding bag, a patient connection port, an oxygen reservoir bag, a pressure control system, and a positive end-expiratory pressure (PEEP) valve (Figure 1) [10].
BVMs facilitate positive pressure ventilation for apnoeic patients and are also commonly employed for preoxygenation in spontaneously breathing patients both during transport and in intensive care units (ICU) [11, 12]. Boulton et al. [13] reported that the most common preoxygenation stra-tegy from all UK Helicopter Emergency Medical Services was a BVM with a PEEP valve.
This equipment offers a significant advantage in medical transport: it requires no fresh gas supply. In the event of any accidents or issues with oxygen supply, room air ventilation remains feasible. However, its use demands significant respiratory effort from the patient, which, coupled with the high work of breathing reported during spontaneous ventilation with adult BVMs, could lead to ineffective preoxygenation and further deplete the patient’s respiratory reserves [9].
While BVMs can provide 100% oxygen concentration under positive pressure ventilation with a well-sealed face mask and high fresh gas flow, their efficiency varies. Not all BVMs are created equal; some lack an expiratory valve, allowing room air to enter during inspiration and significantly reducing oxygen concentration. Additionally, in scenarios where the patient’s minute ventilation surpasses the fresh gas flow, room air entry can dilute the FiO2 to levels below 0.5. Given that critically ill patients often exhibit hyperventilation, the suitability of BVMs for preoxygenation in such contexts is questionable [14].
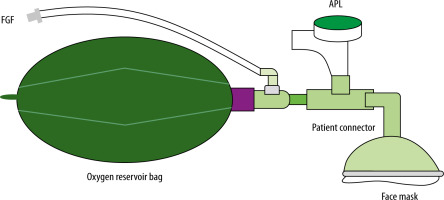
The Mapleson C circuit represents an alternative for preoxygenation, especially during spontaneous breathing (Figure 2). The Mapleson C circuit can be employed during both spontaneous and controlled ventilation, requiring a fresh gas flow of twice the patient’s minute ventilation for the former and up to 2.5 times for the latter to prevent rebreathing and hypercapnia. During inspiration, fresh gas enters the circuit between the reservoir bag and the APL valve and flows to the patient. The APL valve should be open, which makes circuit pressure inappreciable. In controlled ventilation the APL valve should be partially closed to generate positive pressure squeezing the bag [15].
Stafford et al. [15] conducted a comparative study between BVM and the Mapleson C system for preoxygena-tion, noting higher mean and end- expiratory oxygen concentrations with the Mapleson C system. The subjective ease of breathing also favoured the Mapleson C circuit, reflecting the reduced work of breathing. These findings suggest that the Mapleson C circuit might offer an advantage in maintaining higher FiO2 levels and improved patient comfort, especially pertinent for critically ill patients in respiratory failure.
The Mapleson C circuit can be directly connected to a ventilator circuit for advanced respiratory monitoring. This capability allows for real-time tracking of minute ventilation, tidal volumes, capnography, pressures, and waveforms, enhancing patient safety during preoxygenation and intubation. Clinicians can seamlessly transition from spontaneous to controlled ventilation by adjusting the APL valve, benefiting from the tactile feedback from the soft reservoir bag. This ensures effective ventilation and secure preoxygenation, particularly crucial in high-risk intubations [11]. While the Mapleson C circuit offers certain advantages, it is crucial to note its weaknesses. It requires trained personnel familiar with this equipment and a continuous gas supply.
In conclusion, the significance of optimal preoxygenation cannot be overstated, particularly in critically ill patients where tracheal intubations are fraught with risk. The choice of preoxygenation device is paramount, necessitating thoughtful consideration of the patient’s clinical status and the specific procedural requirements. While BVMs are invaluable in emergency settings, their efficacy in preoxygenation varies, influenced by patient effort, expiratory valve presence, and gas flow rates (Table 1). The Mapleson C circuit appears to be a viable alternative, potentially offering superior oxygenation and reduced work of breathing. Nonetheless, more research is required to validate its application across diverse clinical scenarios and establish evidence-based guidelines for device selection in critical care settings.
TABLE 1
Differences between the self-inflating bag valve mask and the Mapleson C circuit