Introduction
Psoriasis is a chronic multifactorial dermatosis with an autoimmune and genetic background, with characteristic periods of remission and exacerbation, affecting up to 3% of the population; it is currently regarded as a systemic disease [1–3]. The aetiology of the disease remains unclear; however, excessive activation of T-helper lymphocytes, which differentiate depending on the stimulus and cause excessive proliferation and differentiation of epidermal keratinocytes, is regarded as an essential factor in disease development [3, 4]. Various local and systemic factors such as trauma, stress, obesity, streptococcal infections, and tobacco smoking may trigger the onset or the exacerbation of the disease [1, 2, 5]. Five types of psoriasis have been described: plaque, guttate, pustular, inverse, and erythrodermic [5].
Management of the disease includes topical therapy with corticosteroids, vitamin D3 derivatives, or calcineurin inhibitors in the case of mild psoriasis, and phototherapy or systemic therapy (cyclosporine, fumarates, methotrexate, and retinoids) in moderate-to-severe cases. A better understanding the immunological background of the disease and developments in biotechnology have enabled the introduction of new drugs, such as proteins that target a selected stage of the immune response; in addition, anti-TNF-α inhibitors, interleukin blockers, and T-cell agents are being used [3–8].
Although the oral cavity is considered a potential source of inflammation that influences overall health and may impact skin conditions, minimal data describe the oral health condition and dental needs in psoriatic patients.
Aim
The aim of this study was to investigate the oral health status including oral mucosal lesion frequency and dental treatment requirements in psoriatic patients managed with biological therapies.
Material and methods
Forty-two patients diagnosed with psoriasis and undergoing biological treatment in the Dermatology Department of Poznan University of Medical Sciences were enrolled in this study. The data collection took place from November 2018 to September 2019. The inclusion criterion involved a therapeutic regimen for at least 12 weeks before examination in order to evaluate the effects of the treatment. Every subject who qualified for biological therapy was obliged to present a dental certificate, indicating the absence of a chronic inflammatory process in the oral cavity in order to qualify for therapy.
Patients with no definitive diagnosis of psoriasis and who did not sign the informed consent form were excluded.
A qualified dental specialist experienced in oral disease diagnostics and treatment performed a detailed oral examination consisting of anamnesis and clinical evaluation of all the recruited subjects. The history of the patients included age, gender, dental hygiene habits, subjective complaints related to the oral cavity, and addictions. Oral cavity examinations were performed in artificial light with a dental mirror and a WHO periodontal probe.
The following indices were used to evaluate the oral hygiene, and the dental and the periodontal status: Approximal Plaque Index according to Lange et al. (API), the Decayed, Missing, and Filled Teeth (DMFT) index, and the Community Periodontal Index (CPI) [9, 10]. The oral mucosa evaluation was based on the appearance of the lesions, their location, and morphology. Denture stomatitis (DS) was categorized according to the Newton classification and described as Type 1, Type 2, or Type 3.
The Psoriasis Area and Severity Index (PASI) score was used to assess the severity of the disease as remission (score 0), mild (< 10), moderate (10–18), or severe (> 18). Additionally, all patients completed a general medical history and Dermatology Life Quality Index (DLQI) questionnaire, which classified the effect of the disease on the quality of life as none (score 0–1), small (2–5), moderate (6–10), very large (11–20), and extremely large (21–30) [11].
Results
The study group comprised 24 men and 18 women, with an average age of 47 years (range: 20–69 years, SD = 24.5). The mean duration of the disease was 28 years (range: 5–60 years, SD = 27.5). The majority of the group suffered from psoriasis vulgaris (27; 64.3%), whereas co-occurrence of psoriatic arthritis appeared in 15 cases (35.7%). Half of the participants reported a positive family history of psoriasis. Most patients (30; 71.4%) received tumour necrosis factor (TNF) inhibitors. The biological management was as follows: adalimumab (20), ustekinumab (7), infliximab (6), secukinumab (5), golimumab (2), and etanercept (2).
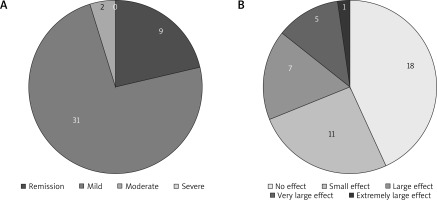
According to the severity of psoriasis, most patients were classified as mild, and in most cases, the disease had no or little effect on their quality of life (Figure 1).
Figure 1
The distribution of study population according to the severity of psoriasis (PASI scale, A) and the effect on the quality of life (DLQI, B)
Twelve subjects (28.6%) smoked tobacco. The mean duration of tobacco use was 17 years (range: 5–40 years, SD = 10.1). Nine patients (21.4%) used acrylic removable denture appliances, and 1 of them also wore the denture during the night. The types of appliances used are presented in Table 1.
Table 1
The types of removable denture appliances used by the psoriatic patients
Most of the patients used acrylic denture appliances; only 3 of them used frameworks.
Three (7.1%) subjects were diagnosed with denture-related stomatitis (DS), and 1 patient (2.4%) presented with angular cheilitis. In the present study we found that the diffuse type of inflammation was most frequently observed in psoriatic patients, the lesion being located on the hard palate and confined to the mucosa in contact with the acrylic denture plate.
Burning sensation of the mouth and dryness of the oral mucosa were found to be frequent complaints in DS.
Only 2 patients (4.8%) from the study group reported subjective complaints, which included: gum bleeding (1 patient; 2.4%) and a burning sensation of the tongue (1; 2.4%).
The oral health status was determined from the following indices: Approximal Plaque Index according to Lange et al. (API), the Decayed, Missing, and Filled Teeth (DMFT) index, and the Community Periodontal Index (CPI). The results are shown in Table 2.
Table 2
The oral health status of psoriatic patients managed with biologic therapy
| Parameter | Mean | Min. | Max. | SD |
|---|---|---|---|---|
| D | 0 | 0 | 4 | 1.0 |
| M | 13 | 0 | 32 | 8.5 |
| F | 7 | 0 | 15 | 4.2 |
| DMFT | 20 | 4 | 32 | 6.5 |
| API | 69.5 | 18 | 100 | 21.5 |
| CPI | 2.5 | 0 | 4 | 1.1 |
The mean value of the Approximal Plaque Index was 69.5, which indicates average hygiene in the study group, which requires improvement. The mean value of decayed teeth (D) was 0, pointing to good caries management and resulting in a low need for conservative treatment. On the other hand, the high mean value of missing teeth (M) required many prosthetic interventions.
Oral mucosal lesions were present in 29 individuals (69%). The most commonly found alterations included the following: fissured tongue (18 cases, 42.9%), white coated tongue (11 cases; 26.2%), and linea alba (9 cases; 21.4%). Thirteen patients (31%) presented with clinically healthy oral mucosa. In some cases, more than one type of pathologic change was observed in a subject concurrently.
Table 3 shows the prevalence of oral mucosal lesions in the study population. Fissured tongue was the most commonly observed oral pathologic lesion.
Table 3
The prevalence of mucosal lesions in patients with psoriasis managed with biologic therapy (N = 42)
Fissured tongue was a common manifestation of the tongue observed in patients with psoriasis. It is distinguished by a deep, prominent groove on the dorsum of the tongue (Figure 2).
Type II (diffuse type) of DS was found most frequently amongst patients with psoriasis who were also wearers of acrylic removable dentures. All patients exhibited a lesion in the upper jaw – type 2 of DS in subjects with psoriasis, as illustrated in Figure 3.
Figure 3
Type 2 DS, diffuse hyperaemic mucosa extending over the entire denture-bearing area in an acrylic complete denture wearer with psoriasis

The need for dental treatment was observed in 30 (71.4%) patients. In some cases, more than one dental procedure was recommended. Most of the subjects required prosthetic treatment (24 cases; 57.1%) and the removal of calculus (17 patients; 40.5%). Also, a prevalence for caries management was noticed (12 patients; 28.6%); however, no one required surgical treatment (Table 4).
Discussion
A better understanding of the immunological background of autoimmune inflammatory diseases and the development of biotechnology has enabled the introduction of new drugs – such as proteins with a target at selected stage of the immune response. Excessive activation of T-helper lymphocytes, which differentiate depending on the stimulus and cause excessive proliferation and differentiation of epidermal keratinocytes, is essential in psoriasis development. IL-12 is responsible for the differentiation of Th1 cells, whereas IL-23 influences the maturation of Th17 lymphocytes, which are also associated with inflammatory bowel diseases, rheumatoid arthritis, multiple sclerosis, and inflammatory response in obesity. Large molecular-weight proteins, administered as injections in targeted therapy, are known as biologics and include receptor fusion proteins and monoclonal antibodies [3, 4, 8]. They were introduced in psoriasis treatment in 2002 and led to significant improvement in management efficacy [12].
With its high microbiome content, the oral cavity is considered a potential source of inflammation that influences overall health and may impact skin conditions and provoke the first manifestation or exacerbation of psoriasis. The structural similarities between streptococcal M protein and epidermal keratins inducing cross-reactivity are present in the psoriasis pathogenesis [13, 14].
The association between psoriasis and periodontitis is described in the literature and even includes periodontitis as a new comorbidity of psoriasis. The elevated levels of cytokines, such as tumour necrosis factor-α (TNF-α), IL-17, and IL-22, are described in the pathogenesis of the periodontal disease, which are also targeted by biologics. That may lead to the improvement of periodontal parameters in patients managed with these new drugs [15–18].
There are minimal data on the oral health condition in psoriatic patients. However, some authors have reported a high number of missing teeth in this population [18–20]. Our study seems to confirm this observation, as more than half of subjects required prosthodontic treatment, probably as a result of the removal of the inflammation foci before the commencement of therapy, which is essential in order to avoid harmful side effects of biological agents and the exacerbation of psoriasis [3, 13].
The use of removable denture appliances, especially for a prolonged period, may lead to the overgrowth of Candida albicans, a fungus that is one of the many oral microflorae [21–23]. In our study, type II of DS – diffuse hyperaemic mucosa extending over the entire denture-bearing area – was found most frequently amongst patients with psoriasis. All patients exhibited a lesion in the upper jaw. This may be attributed to the isolation of oral mucosa tissues under a maxillary complete denture, particularly when the maxillary denture forms a good seal, resulting in its own microenvironment, disturbing the normal microbiological balance in the space. Additionally, DS in the maxilla may be associated with the amount of tissue covered by the maxillary denture plate and its strong retention [23].
It is advantageous to administer a combination of miconazole and antimicrobial photodynamic therapy to manage Candida biofilm in patients with Candida-associated DS [24, 25].
This condition may spread the infection from the denture-covered oral mucosa to the angles of the mouth. It is assumed that in angular cheilitis, the lesions are infected by either Candida albicans and Staphylococcus aureus, or both [23–25].
The oral mucosal lesions associated with psoriasis are mainly limited to the tongue. Fissured tongue described as the presence of anteroposteriorly or laterally oriented fissures on the dorsal surface of the tongue affects 2–5% of the general population and seems to be the most common oral lesion in psoriatic patients [26–29]. The geographic tongue, characterized as well-demarcated zones of erythema at dorsal tongue mucosa, because it is associated with increased levels of TNF-α and IL-6, occurs less frequently in a population managed with biologicals [26, 30].
This study presents the oral health status in psoriatic patients managed with modern biological drugs. The elimination of foci inflammation led to loss of teeth, which resulted in an urgent need for prosthetic intervention. Further investigation, including the measurement of periodontal parameters and serum and saliva levels of inflammation markers, is required to confirm the influence of the drugs on the periodontal condition. A detailed oral mucosa examination performed before and after the biologic treatment may be necessary to verify the improvement of the tongue condition. Because the oral cavity is a potential source of inflammation, which may enhance psoriasis, meticulous oral and denture hygiene in addition to regular dental visits should be recommended to all psoriatic patients.
Conclusions
This study showed that fissured tongue seemed to be associated with skin lesions in psoriatic patients managed with biological therapies. The study also indicated that the diffuse type of denture stomatitis occurred amongst subjects with psoriasis, who were also wearers of acrylic removable dentures. Moreover, the need for dental treatment was observed in 71.4% of the patients, with most subjects requiring prosthetic treatment. The use of dental indexes to assess oral health should be recommended in addition to standardized Psoriasis Area and Severity Index (PASI) and general medical history of psoriatic patients.









