A 33-year-old woman was admitted due to an 8-month history of multiple solitary subcutaneous masses on bilateral thighs, lower abdomen and waist. At first, she developed a small painless subcutaneous nodule on the right thigh and the lesion grew larger with time. One month later similar lesions developed on the left thigh, lower abdomen and waist. An excisional biopsy performed in an outside facility was interpreted as lupus panniculitis, and the patient was treated with hydroxychloroquine 200 mg twice a day for 2 months without any improvement. Because of the recalcitrant disease course, the diagnosis of lupus panniculitis was questioned, and the patient was referred to our hospital for another biopsy.
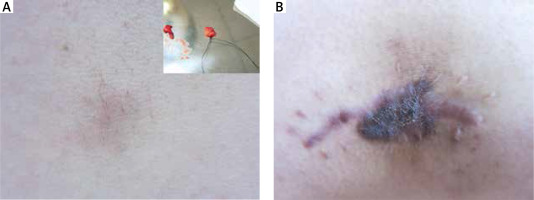
Physical examination revealed that firm non-tender subcutaneous masses were present on the bilateral thighs, lower abdomen and waist, ranging from 2 × 3 cm to 6 × 7 cm in diameter. The surface colour was dark red to brown. Increased hair growth was noted overlying the lesion (Figure 1 A). Previous biopsy scar was seen on the right thigh without recurrent lesions in the vicinity (Figure 1 B). There was no palpable lymphadenopathy or hepatosplenomegaly.
Figure 1
A – Firm non-tender subcutaneous masses with dark red surface and increased hairs on the left thigh, 4 × 5 cm in diameter. B – Previous operation scar on the right thigh without recurrent lesions in the vicinity
Her laboratory analysis disclosed the following values: antinuclear antibody (ANA) was positive with a titre of 1 : 320, while ds-DNA and the other autoimmune markers were negative. Serum protein electrophoresis levels were normal, and erythrocyte sedimentation rate was 15 mm/h. Results of the blood count, urine and biochemical profile were within normal limits. Other studies including rapid plasma regain (RPR), treponema pallidum particle agglutination assay (TPPA), human immunodeficiency virus (HIV), hepatitis B virus (HBV) and antibody against cytomegalovirus were all negative. Imaging studies including X-ray, computed tomographic scan and echocardiography were normal.
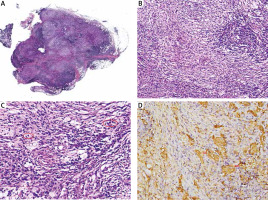
Histology of the representative lesion revealed normal epidermis, dermis and sheets of histiocytes with a pale pink cytoplasm surrounded by dense infiltrate of lymphocytes and plasma cells in the fat lobules. The large histiocytic cells had indistinct borders, abundant pale pink cytoplasm and large vesicular nuclei (Figure 2 A–C). The stain for S-100 protein highlighted these histiocytes and emperipolesis (Figure 2 D). Staining for CD68 was also positive but CD1a was negative. Direct immunofluorescence was negative. On the basis of the histiocytic infiltrate with emperipolesis and immunohistochemical staining results, the diagnosis of Rosai-Dorfman disease was made.
Figure 2
A – Lobular panniculitis infiltrate at low magnification (H&E, original magnification 10×). B – Sheets of pale histiocytes surrounded by dense infiltrate of lymphocytes and plasma cells (H&E, original magnification 100×). C – Large histiocytes with indistinct borders, abundant pale pink cytoplasm and large vesicular nuclei, displaying emperipolesis (H&E, original magnification 200×). D – Large histiocytes positive for S-100, highlighting emperipolesis
The patient received re-excision for the lesion on the waist, but refused other for cosmetic reasons. The patient had no fertility requirement, then she was given thalidomide 50 mg twice a day for 3 months without remission and then the treatment was stopped. During 1-year follow-up, no new lesions developed, however, the previous lesions persisted.
Rosai-Dorfman disease (RDD) is a benign proliferation of histiocytes that primarily presents with lymphadenopathy with unknown aetiology. Cutaneous Rosai-Dorfman disease (C-RDD) is a rare form limited to the skin, which was first reported by Thawerani in 1978. Its clinical features are heterogeneous and include single or, more commonly, multiple, indurated papules, plaques or nodules of different sizes with no anatomical predilection site. It has also presented as subcutaneous masses (panniculitis), which is a rare clinical manifestation [1]. Our case presented with multiple subcutaneous masses mimicking panniculitis. Another rare manifestation of our patient was increased hair confined to the lesional areas without any obvious cause, which we were unable to find any previous reports described in the literature.
Histological findings in Rosai-Dorfman disease are characteristic. A dense histiocytic infiltrate is accompanied by a background infiltrate of lymphocytes and plasma cells. The large histiocytic cells have indistinct borders, abundant pale pink cytoplasm and large vesicular nuclei, exhibiting the phenomenon of emperipolesis (cytophagocytosis of lymphocytes and plasma cells). The histiocyte stains positively for S-100 protein and CD68, but negatively for CD1a, which rules out the possibility of Langerhans cell histiocytosis. S-100 staining often highlights the histiocytic cells and emperipolesis. The unique feature of our case is that the epicentre of the lesions is localized entirely in the subcutaneous fat mimicking lobular panniculitis and sparing the dermis. Fibrosis can be seen in the septa. Pathologically subcutaneous Rosai-Dorfman disease should be differentiated from lupus panniculitis and cytophagic histiocytic panniculitis. Although these two entities show panniculitis, they are quite different in pathology. As for lupus panniculitis, it lacks histiocytes, and S-100 is negative. Cytophagic histiocytic panniculitis shows infiltration of histiocytes and cytophagocytosis, but plasma cells are not as many as in Rosai-Dorfman disease and S-100 for histiocytes is also negative.
Cutaneous Rosai-Dorfman disease has a good prognosis and usually does not require treatment but surgical excision may be indicated for cosmetic reasons or symptomatic relief. It also responds to radiotherapy, thalidomide [2], dapsone [3], methotrexate [4] and intralesional corticosteroid [5]. Unlike most reported patients, our patient has not shown any signs of spontaneous regression, nor has her disease caused significant morbidity during the follow-up, so there was no further treatment given.








