Due to demographic aging and increasing comorbidities, cardiac surgery may still be associated with high morbidity, mortality, and prolonged postoperative stay, despite significantly increased knowledge and modern, much less invasive techniques [1–4]. The population of patients with cardiovascular disease planned for cardiac surgery has a high prevalence of advanced age, frailty, low cardiac fitness and severe extracardiac comorbidities, which may exacer-bate the decline in physiological reserve and influence the final outcome [1–2, 5]. The loss of functional capacity often observed during the preope-rative waiting period has an additional negative impact on postoperative problems, including pulmonary and neurological complications [2–4].
The main objective of this study was to evaluate the impact of comprehensive preoperative interdisciplinary assessment by the Pre Surgery Check (PreScheck) Team on optimizing the final selection for elective cardiac surgery.
METHODS
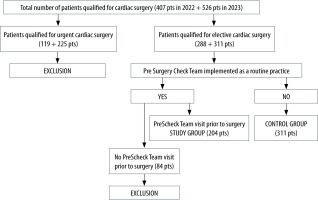
This is a single-centre, prospective, observational study conducted in the Department of Cardiac Surgery. The study population consisted of 933 adult patients (over 18 years) planned for cardiac surgery (elective and emergency) during 1.01.2023–30.03.2023 (407 patients) and 1.03.2022–30.06.2022 (526 patients). Exclusion criteria were: 1) eligibility for emergency/urgent cardiac surgery and 2) time to surgery less than one month (for the study group). The study protocol was approved by the local bioethics committee (decision number 1072.6120.78.2023). All study participants signed an informed consent form.
The flowchart of the study and control group selection is summarized in Figure 1.
Initial eligibility for elective cardiac surgery was based on the recommendation of the Heart Team, which was then always verified after personal exami-nation of the patient by at least the anaesthesiologist and the cardiac surgeon. The following factors were considered before making the final decision: Heart Team recommendations, individual risk profile, technical aspects, and patient opinion.
The PreScheck Team started working in our hospital in October 2022 and all patients scheduled for elective cardiac surgery after 1 January 2023 were routinely referred for an outpatient visit prior to hospitalization. All patients in the study group were then personally reassessed and thoroughly examined by the PreScheck Team during their 2-hour clinical appointments organized 1–3 months prior to their planned cardiac surgery. Patients in the control group, who underwent surgery prior to the introduction of the PreScheck assessment as a standard of preoperative care in our hospital, were not seen by the multidisciplinary medical team prior to their planned surgery.
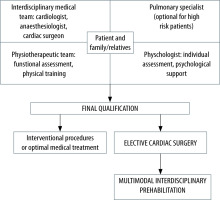
The PreScheck Team is an original concept that combines traditional preoperative assessment and an outpatient prehabilitation clinic. PreScheck involves the collaboration of a number of specialists and aims to prepare the patients for elective cardiac surgery by increasing their functional reserve. The PreScheck Team also aims to confirm eligibility for cardiac surgery on the basis of an individual risk assessment. The process includes: 1) interdisciplinary medical assessment by a cardiologist, anaesthesiologist and cardiac surgeon who meet the patient and verify all data with physical examination; 2) pulmonary assessment (for patients with high risk of postoperative pulmonary complications); 3) physiotherapeutic assessment and training; 4) psychological assessment.
The organization of the PreScheck Team is summarized in Table 1 and Figure 2.
TABLE 1
Components of Pre Surgery Check Team assessment
[i] ASA – American Society of Anaesthesiologists, BMI – body mass index, CABG – coronary artery bypass grafting, CCS – Canadian Cardiovascular Society, CSF – Clinical Frailty Scale, CT – computed tomography, EuroSCORE II – European System for Cardiac Operative Risk Evaluation, NRS 2002 – Nutritional Risk Score 2002, NYHA – New York Heart Association
The following parameters were assessed and compared between the groups: demographic and clinical data, the need to postpone surgery due to extension of diagnostics and percentage of exclusion from elective cardiac surgery.
Statistical calculations were performed using STATISTICA v 13.3 software. Categorical variables were expressed as numbers (%) and when the assumption for the chi-squared test was not met, Fisher’s exact test was used. A P-value less than 0.05 was considered significant. Continuous variables were expressed as mean (standard deviation) or median (interquartile range) and compared using Student’s t-test. The Kolmogorov-Smirnov test was used to test for normality.
RESULTS
The study group (PreScheck Team group) consisted of 204 consecutive patients (143 male), aged 27–82 years (mean age 64.8 years), planned for elective cardiac surgery in our department within 3 months from 1 January 2023, who underwent a comprehensive assessment by the PreScheck Team 1–3 months prior to their planned cardiac surgery. The control group (No PreScheck Team group) consisted of 311 consecutive patients (197 male), aged 22–83 years (mean age 65.1 years), scheduled for elective cardiac surgery between 1 March 2022 and 30 June 2022 (4 months), without preoperative interdisciplinary assessment. There were no statistically significant differences between the groups with respect to sex, age, BMI, LVEF, nutritional status and comorbidities. The characteristics of both groups are summarized in Table 2.
TABLE 2
Demographic and clinical characteristics of the study group (surgery in 2023) and the control group (patients planned for surgery in 2022)
Forty-six patients (22.6%) from the study group were finally excluded from the surgery on a scheduled date. In all patients temporary or permanent exclusion from surgery was a result of the PreScheck Team assessment. Twenty-five patients (12.3%) were permanently excluded from cardiac surgery. Only 3 patients in the study group required hospital admission prior to planned surgery and additional tests. The total hospital stay for these 3 patients was only 7 days. In the control group 42 patients (13.5%) did not have surgery on the scheduled date and 27 patients (9.0%) were permanently excluded from cardiac surgery. All patients were admitted to the hospital and required additional tests before the final clinical decision was made. In the control group, the total length of hospital stay prior to exclusion was 146 days (Tables 3 and 4).
TABLE 3
Results of final clinical decision in both groups
TABLE 4
Characteristics of the patients permanently excluded from surgery (in the study group and control group)
The main reason for permanent exclusion from cardiac surgery in both groups was extremely high individual surgical risk, associated, with e.g., advanced age, high CFS score, pulmonary status, and morbid obesity. Other reasons included technical surgical aspects, e.g., thoracic malformation, lack of venous and arterial material for CABG, which limited the possibility of surgery. After extensive discussion with patients and the family members about the very high surgical risk and questionable benefit, some patients decided to withdraw consent for surgery. The decision to permanently exclude a patient from any procedure was always a joint decision of the PreScheck Team and the Heart Team.
DISCUSSION
The Royal College of Anaesthetists’ 7th National Audit Project (NAP7) revealed many unfavourable trends in the population of non-obstetric surgical patients since NAP5 in 2014 [1]. Data from the survey showed increasing trends in age, obesity, and comorbidities, leading to an increasingly complex perioperative workload [1]. Similar trends, with an increasing prevalence of high-risk patients, have been observed in cardiac surgery [2–4]. The population of patients with cardiovascular disease planned for cardiac surgery is characterised by advanced age, frailty, low cardiac fitness and severe extracardiac comorbidities, which can exacerbate the severe decline in patients’ physiological reserve [2–4]. Analysis of cardiac surgery procedures performed between 2002 and 2016 from the UK National Adult Cardiac Surgery Audit database [2] showed a statistically significant increase in mean age (66.4 ± 12 years), incidence of pulmonary disease and logistic Euro-SCORE [2]. Data from the Polish National Cardiac Surgery Database [3] showed a statistically significant increase in the mean age of patients during 10 years of observation, from 61.4 years in 2006 to 66.1 years in 2016. The authors also reported a high incidence of arterial hypertension (70.3%), diabetes (75.6%) and COPD (7.7%). Analysis of our data strongly confirms these findings and shows a significantly higher percentage of older patients, obesity, arterial hypertension, diabetes, extracardiac arteriopathy and chronic lung disease (Table 1).
According to the current guidelines from both the European Society of Cardiology [8, 9] and the American Heart Association [10], the multidisciplinary Heart Team approach is a class 1 recommendation and a key component of modern patient care. The collaboration of different specialists (cardiac surgeon, interventional cardiologist, and imaging specialist) enables decision-making in both valvular disease and coronary syndromes. In our hospital, the Heart Team consults about 5000 potential surgical candidates per year, and from 2021 all patient referrals have been submitted electronically, allowing the Heart Team to view imaging studies online, albeit with very limited access to the summary clinical data [5]. Unfortunately, a discrepancy between the data in the eligibility forms and the actual condition of the patient was often observed. This discrepancy led to postponement or cancellation of the planned procedure in 13.5% of patients in 2022 (between 1 March and 30 June 2022). Temporary or permanent cancellation affected 22.55% of patients planned for elective cardiac surgery in our centre in the first quarter of 2023 (Table 3).
Enhanced Recovery After Surgery (ERAS; ERACS for cardiac surgery) is a multidisciplinary initiative to promote recovery after surgery [11–13]. Prehabilitation is a concept based on three pillars: physical fitness improvement, nutritional optimization, and cognitive intervention prior to surgical treatment [14]. It is defined as the process of improving a patient’s functional capacity prior to surgery [14–18]. Prehabilitation has the potential to improve surgical outcomes in patients undergoing cardiothoracic surgery, but few studies have investigated the impact of prehabilitation in this patient population [17, 18]. The PreScheck Team is the first regular preoperative unit in our hospital. Until the end of 2022, routine standard preoperative clinical care in our institution did not include nutritional, rehabilitation or psychological support [5].
The PreScheck Team has been working in our hospital since October 2022 [5]. In general surgery, the prehabilitation clinic is usually reserved for high-risk patients. Therefore, in most centres, patients are first seen in the pre-anaesthesia unit, and then only high-risk patients (about 10%) are subsequently followed up in the prehabilitation clinic. However, there are several important issues that need to be considered in prehabilitation and ERAS for cardiac surgery. In cardiac surgery we usually have a limited time frame between the selection process and the date of the surgery, so the time for preoperative clinical evaluation is also significantly limited. It should also be noted that all patients selected for cardiac surgery are at high risk both because of the patients’ baseline clinical status and the procedural risk. Among the various complications following open heart surgery, one of the most common and important difficulties is pulmonary complications, which are associated with subsequent morbidity and mortality. The preoperative modifiable factors should be carefully considered and evaluated in this population. Among the most important factors affecting the postoperative course and long-term outcome after cardiac surgery, special attention should be paid to: diabetes and its complications, obesity, and chronic lung disease. Based on these data we have adopted the following principles for the PreScheck Team: 1) all patients scheduled for elective cardiac surgery should be assessed by the PreScheck Team (if possible); 2) the PreScheck visit consists of two distinct elements: comprehensive multidisciplinary clinical assessment (equivalent for pre-anaesthesia clinic) and a prehabilitation visit at the same time; and 3) special attention should be paid to the preoperative assessment of pulmonary status and dedicated pulmonary rehabilitation.
The PreScheck Team model is actually a hybrid of a short-term outpatient preoperative ward and a prehabilitation clinic. It allows the simultaneous multidisciplinary assessment of different health professionals: cardiologist, cardiac surgeon, anaesthesiologist, pulmonologist, physiotherapist, and psychologist (Figure 2). Unlike other types of surgery, cardiac surgery patients should be evaluated as soon as possible after selection for the procedure. We believe the optimal time between evaluation and surgery is 3–6 weeks. This allows for additional testing, treatment optimization, as well as nutritional and physical therapy interventions. The following laboratory tests are recommended before the PreScheck Team visit: blood count, creatinine and eGFR, INR, APTT, HbA1c (in diabetes). Additional tests are often recommended by the PreScheck Team depending on the patient’s comorbidities.
The main aim of the PreScheck Team is to prepare the patients for elective cardiac surgery by increasing their functional reserve, providing nutritional intervention, reducing anxiety, and optimizing disease compensation during the waiting period. A direct discussion with the patient and his or her family allows for clarification of any doubts about the patient’s upcoming procedure. Patients scheduled for elective cardiac surgery in our centre have been personally examined (in the presence of their relatives) 1–3 months before the planned hospital admission. In case of any clinical doubts, it is possible to perform additional diagnostic tests or specialist consultations on an outpatient basis. In our hospital, 70.8% of the patients planned for elective cardiac surgery between 1 January and 31 March 2023 were seen by the PreScheck Team visit prior to surgery (Table 2).
By the end of 2022, approximately 10% of patients in our clinic were seen in the outpatient cardiac surgery clinic prior to the planned procedure. Therefore, for the majority of patients, elective surgery eligibility was based on the limited clinical data available and was determined only on the recommendation of the Heart Team. The final assessment of the patient’s condition and ability to undergo the procedure took place after admission to hospital. During 4 months in 2022 (1.03–30.06.2022), 42 patients (13.5% of the control group) were temporarily or permanently excluded from elective cardiac surgery on the planned date. 4.98% of patients had their surgery postponed due to additional tests or changes in treatment. 8.97% of patients were permanently excluded from cardiac surgery (48.2% of this group were eventually referred for optimal medical treatment only). Hospitalization (median 4 days, interquartile range 2–7 days) was necessary to perform additional diagnostics and to make the final decision on optimal therapy. Finally, the need to verify the diagnosis and the decision of the Heart Team resulted in 146 days of hospitalization for 42 patients. Following the introduction of the PreScheck Team in our hospital, in the first quarter of 2023, 46 patients were excluded from elective surgery on the planned date (22.6% of the study group). 13.3% of patients were postponed and 12.3% were permanently excluded from cardiac surgery. Importantly, in all patients from the study group additional diagnostics were performed on an outpatient basis and the final clinical decision regarding the type of treatment was made during the PreScheck Team visit. Only 3 patients required hospitalization prior to final exclusion from cardiac surgery, resulting in a statistically significant reduction of pre-surgery hospital length of stay (median 0 days, total hospital length of stay for the study group 7 days). Extrapolating the data from 2022 (median hospital length of stay 4 days), it can be assumed that these 46 patients would have generated 184 days of hospitalization before the PreScheck era. The potential “savings” of about 180 days of hospitalization allowed more patients to be admitted for cardiac surgery and much lower hospital costs, which will be analysed separately in the future publications. The PreScheck Team visit takes place in the outpatient clinic and does not require hospital admission. In our centre, the implementation of the PreScheck Team did not generate any additional costs. The PreScheck Team involves ward staff: doctors, psychologists and phy-siotherapists who have agreed to take on additional duties. However, we realize that in the future the PreScheck Team should be a separate outpatient clinic with its own staff.
PreScheck Team visit and length of hospital stay are the only statistically significant differences between the study and control groups for patients permanently excluded from cardiac surgery (Table 2). The main reason for permanent exclusion from cardiac surgery in both groups was unacceptably high operative risk associated mainly with advanced age, frailty, morbid obesity, and pulmonary status.
Decision-making in patients with cardiovascular disease should include accurate diagnosis and timing of intervention [8–10]. Individual risk assessment is mandatory before selecting the most appropriate type of procedure. Unfortunately, most perioperative algorithms have inadequate diagnostic accuracy and tend to overestimate the baseline risk. In addition, they are not widely used worldwide. The EuroSCORE II scale has been validated to predict the risk of death in patients undergoing cardiac surgery [6]. The EuroSCORE score (expressed as a percentage) is a probability that the patient will die during or shortly after the proposed surgery. EuroSCORE does not reflect the likelihood of non-fatal postoperative complications, which often limit the benefit of surgery [19]. The Society of Thoracic Surgeons (STS) score calculator [19] allows calculation of a patient’s risk of mortality and morbidity for the most commonly performed cardiac procedures but it is complicated and time-consuming. It should be emphasized that no risk model predicts the outcome for an individual patient. At the same time, the only universal index is still the American Society of Anesthesiologists (ASA) Physical Status Classification System [7, 21]. It is important to remember that EuroSCORE II or STS calculators are only complementary methods for patient risk assessment.
It should be noted that none of the perioperative risk scales take into account obesity (BMI values) or frailty in elderly patients [6, 7, 20]. Postoperative pulmonary complications remain the leading cause of surgery-related morbidity and mortality in cardiac surgery [22]. Obesity is a significant and increasingly common cause of respiratory compromise. It can alter lung function and reduce exercise capacity through its adverse effects on respiratory mechanics and respiratory muscle function [22–24]. Obese patients are at risk of aspiration pneumonia, pulmonary thromboembolism, and respiratory failure after cardiac surgery [22]. Gao et al. [25] reported that extreme obesity (BMI ≥ 40 kg m–2) was significantly associated with severe major adverse clinical outcomes (deep sternal infection, prolonged ventilation and need for renal dialysis), mortality, and readmission in patients after CABG. In our study obesity (BMI > 30 kg m–2) was observed in 33.33% of patients in the study group and 40.31% in the control group. At the same time, despite this significant proportion of people with obesity, 36.01% of the control group and 35.29% of the study group were at risk of malnutrition according to the NRS 2002 (NRS 2002 ≥ 3 points). In the study group, all patients at high risk of malnutrition received nutritional support from the multidisciplinary medical team in consultation with the hospital dietitian during the Pre-Scheck Team visit. It is reported that approximately 44% of all patients hospitalized for an elective surgical procedure are at risk for malnutrition. Preoperative malnutrition is associated with increased risk of postoperative complications, increased mortality and prolonged hospital stay [26]. Obese patients require a comprehensive assessment of nutritional status, and malnutrition often goes undiagnosed [26].
Frailty leads to continuous depletion of functional reserve after surgical stress [27]. It is recognized as contributing to adverse postoperative outcomes in cardiothoracic patients [28, 29]. The Clinical Frailty Scale (CFS) has been validated in adults aged over 65 years of age and is a commonly used tool to screen for frailty. However, the CFS is not a direct measure of frailty but a set of descriptions, often based on a patient report, which by definition is not objective [30]. Furthermore, it is a judgement-based frailty tool that assesses specific domains including comorbidity, function, and cognition. Flaaten et al. [31], in a prospective study testing the reliability of the CFS in ICU patients, found a high compliance rate and good overall inter-rater agreement, with small variations in performance between different healthcare professionals, countries and data sources. We believe that an individualized assessment should be recommended in all cases where the CFS is inappropriate or ineffective. The physiotherapeutic assessment proposed in the PreScheck Team concept includes not only the CFS score but also the Timed Up and Go test, respiratory muscle strength, chest expansion and shoulder range of motion. This type of comprehensive assessment seems to reflect the actual functional status of the patient more reliably.
An individualized and comprehensive surgical risk assessment performed by a group of specialists should always be recommended, especially for high-risk patients. Based on our own experience, we believe that a comprehensive personal assessment by an experienced multidisciplinary team cannot be replaced by any available risk calculator.
LIMITATIONS
The study and control groups were not followed simultaneously. The patients were recruited at different times (2022 and 2023), which may have influenced the different characteristics of the groups.
The article does not compare the two groups in terms of immediate and long-term outcomes of cardiac surgery. Analysis of the short and long-term outcomes in the PreScheck Team era compared to these outcomes before the PreScheck Team requires analysis of larger patient groups and longer follow-up.
CONCLUSIONS
The purpose of the PreScheck Team visit is to confirm the Heart Team selection for cardiac surgery based on the individual risk assessment. Multimodal patient assessment by a multidisciplinary team (including a cardiologist, cardiac surgeon, anaesthesiologist, pulmonologist, and physiotherapist) identifies potential risk factors that may affect the postoperative course. A single visit to the Pre-Scheck clinic allows for additional diagnostic testing and prevents unnecessary hospitalization. The approach we propose here should be a complementary step in the process of selection for elective cardiac surgery, in addition to the Heart Team recommendation. This two-step decision-making process allows for individual risk assessment, selection of the most appropriate intervention, as well as better use of medical resources.