Dear Editor,
This letter describes an extravasation problem case of an Edwards PreSep Oximetry Catheter (Edwards Lifesciences Japan Ltd., Tokyo, Japan) inserted via the right supraclavicular approach and discusses the incompa-tibility between an oximetry central venous catheter (CVC) and the right supraclavicular approach.
A 37-year-old female patient (height 163 cm; body mass 42 kg) underwent a pulmonary valve replacement due to stenosis and regurgitation of the transannular patch after corrective surgery for tetralogy of Fallot about 30 years ago. While a Swan-Ganz pulmonary artery catheter provides considerable information concerning patients’ circulatory status such as mixed venous saturation (SvO2) [1] and cardiac output (CO) [2] for the perioperative management, the stay time in the intensive care unit (ICU) is extended and medical costs increase because of its use [3]. Moreover, Swan-Ganz pulmonary artery catheters were reported to increase risks of adverse events, including bacteraemia and pulmonary embolism [4, 5]. Therefore, considering the operative procedure of a pulmonary valve replacement, we decided against the use of a Swan-Ganz pulmonary artery catheter. The perioperative anaesthesia management and haemodynamic monitoring were performed using transoesophageal echocardiography (TOE) in combination with a FloTrac Sensor (Edwards Lifesciences Japan Ltd., Tokyo, Japan) to analyse the CO. An Edwards PreSep Oximetry Catheter was used for the measurement of central venous oxygen saturation (ScvO2) in the superior vena cava (SVC) instead of a Swan-Ganz pulmonary artery catheter.
An 8.5 Fr Edwards PreSep Oxime-try Catheter, a widely used oximetry CVC in adult patients in daily clinical practice, was inserted using the real-time ultrasound-guided right supraclavicular approach [6–9] considering patient comfort, and fixed at an insertion depth of 10 cm (6% of the body height) based on the previous study examining the ideal CVC insertion length [10]. The central venous pressure (CVP) line was connected to the proximal lumen as per the standard protocol in our facility so that the changes in the CVP value and curve could be indicated immediately in case CVC became shallower accidentally. Blood was aspirated from the proximal lumen and the CVP value was within the normal range during surgery. Surgery and intraoperative anaesthesia management were uneventful. Postoperative chest X-ray confirmed that the catheter tip was located exactly at the carina level (Figure 1). The patient was extubated in the operating room and transferred to the ICU. However, after several hours in the ICU, the CVP value elevated gradually and exceeded the scale range of the monitor. Blood could not be aspirated from the proximal lumen of the inserted Edwards PreSep Oximetry Catheter; therefore, extravasation of the proximal lumen was suspected. It was also noticed that the patient’s neck swelled slightly, which was assumed to be due to the flushing fluid of the extravasated proximal lumen leaking into the subcutaneous tissue. As the postoperative haemodynamics of the patient were stable and the ScvO2 measurement was not essential for subsequent ICU management, a normal triple lumen CVC, 12G SMAC Plus (Covidien Japan Inc., Tokyo, Japan), was inserted into the right jugular vein and the inserted Edwards PreSep Oximetry Catheter was removed.
FIGURE 1
Postoperative chest X-ray showing Edwards PreSep Oximetry Catheter with the tip located exactly at the carina level. An 8.5 Fr Edwards PreSep Oximetry Catheter (∇) was inserted at a depth of 10 cm inside an adult patient with a height of 163 cm and weighing 42 kg, and its tip was located exactly at the carina level by the postoperative chest X-ray

In current clinical practice, systems for arterial blood pressure measurement such as the FloTrac Sensor that can calculate CO and echocardiography, including transthoracic echocardiography and TOE, are routinely used in emergency outpatient and ICU management and in perioperative management. These tools allow the choice of oximetry CVC, enabling continuous monitoring of ScvO2, instead of the Swan-Ganz pulmonary artery catheter which provides SvO2.
The subclavian and internal jugular vein approaches are commonly used as insertion sites for CVCs rather than the femoral vein owing to CVC-related deep venous thrombosis [11] and CVC-related infections [12]. However, problems, including intravenous thrombosis, can occur when the same approach is repeatedly used [6]. The diameter of the target brachiocephalic vein is significantly larger than that of the subclavian or internal jugular veins, as the brachiocephalic vein exists more proximal to the SVC after the confluence of the subclavian and internal jugular veins. In addition, the entire passage of the puncture needle into the target brachiocephalic vein can be visualized via a long-axis in-plane technique with a real-time ultrasound-guided supraclavicular approach [6–9, 13, 14]. Indeed, the real-time ultrasound-guided supraclavicular approach is reported to be superior to the real-time ultrasound-guided subclavian/axillary vein approach with respect to the success rate and reduced complications [15]. When using the supraclavicular approach, the right side is recommended because catheter tip malposition has been reported in CVCs inserted via the left side [10]. However, for positioning the catheter tip at the carina level, the CVC insertion length via the right supraclavicular approach (6% of the body height in patients > 90 cm tall) is significantly shorter than that via the right jugular vein or left supraclavicular approach, which is the same in the latter two approaches (8–9% of the body height in patients > 90 cm tall) [10]. Although this study is performed in paediatric patients, the tendency of the relationship of ideal CVC insertion depth to the % of body height does not change significantly when body height exceeds 90 cm [10]. It is probably because the ratio of the upper body does not change with further increases in body height and the results of this study are supposed to be applicable to adult patients. Indeed, from our clinical experience, the CVC tip is located around the carina level also in adult patients, as in the patient in this current case.
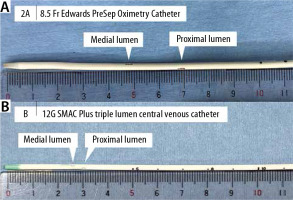
Although the catheter tip was located exactly at the carina level (Figure 1), the intravascular length of the proximal lumen opening seemed not to be long enough, because the opening of the proximal lumen is located at approximately 7 cm from the catheter tip, farther away from the tip than normal CVCs, in an 8.5 Fr Edwards PreSep Oximetry Catheter (Figure 2). As a result, the proximal lumen opening became extravasated during postoperative management in the ICU, and the patient’s neck swelled slightly due to its flushing fluid. This trouble was promptly noticed due to changes in the CVP value and curve because the CVP line was connected to the proximal lumen as a standard protocol in our facility.
FIGURE 2
The catheter tips of the 8.5 Fr Edwards PreSep Oximetry Catheter and a normal central venous catheter (CVC) (e.g. 12G SMAC Plus triple lumen CVC). The openings of the proximal lumen and medial lumen are located at approximately 7 cm and 5 cm, respectively, from the catheter tip in the 8.5 Fr Edwards PreSep Oximetry Catheter (A), farther away from the catheter tip than normal CVCs (B)
This case report highlights the possibility of extravasation of the proximal lumen when using oximetry CVC, especially when inserted via the supraclavicular approach, where the ideal CVC insertion length is significantly shorter than that of other approaches. As described in this paper, the right supraclavicular approach is not recommended when using oximetry CVC because of extravasation risk of the proximal lumen, even in adults of normal height. Similarly, attention should be paid to the insertion length when using the oximetry CVC also in approaches other than the right supraclavicular approach in small adults or paediatric patients.
Written informed consent was obtained from the patient for publication of this case report and an accompanying image.




