Introduction
Uterine fibroids are the most common pelvic tumours occurring in women of reproductive age. It is a benign lesion that originates from smooth muscle tissue. Risk factors for developing uterine fibroids include, among others, African American race, premenopausal state, nulliparity, and obesity [1, 2]. In up to half of the cases, uterine fibroids are asymptomatic and require only regular gynaecological observation. The most common symptoms of uterine fibroids are heavy or prolonged menstrual bleeding, anaemia, pelvic pain, back pain, urination disorders, and constipation [3]. Current treatment options include surgical procedures, pharmacological therapies, and minimally invasive procedures [2, 4]. The most commonly applied and accepted minimally invasive procedure used in the treatment of symptomatic uterine fibroid is uterine arteries embolisation (UAE). Initially, UAE was performed to reduce blood loss during surgical treatment of uterine fibroids. Nowadays, UAE can be used both as an auxiliary method and as the main treatment method for uterine fibroids [5–8]. We present the application of pre-operative UAE before subtotal abdominal hysterectomy in a woman with giant uterine fibroid and HIV-associated nephropathy (HIVAN). Written informed consent was obtained from the patient for publication of this case report and any accompanying images.
Case report
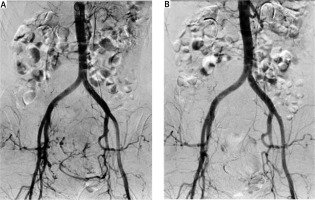
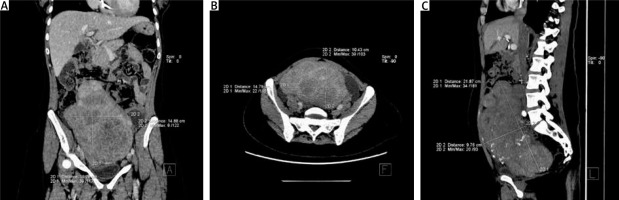
A 45-year-old, unmarried, nulliparous African American woman with a BMI of 27.0 was referred to the Gynaecology and Obstetrics Department, University Hospital No. 4 in Lublin, Poland with a suspicion of uterine fibroid. The main symptoms of this patient were anaemia (haemoglobin [Hb] 8.5 g/dl upon admission), abnormal uterine bleeding (meno- and metrorrhagia), and pressure symptoms (pelvic pain, back pain, urination disorders, constipation). The patient was undergoing chronic treatment for HIV infection (abacavir, lamivudine, and dolutegravir) and regular dialysis due to HIVAN (creatinine serum level at the time of admission – 679.07 µmol/l, estimated GFR – 6.1 ml/min/1.73 m2). Due to the size of the fibroid, the transvaginal ultrasonography was non-diagnostic. Computed tomography revealed a huge fibroid filling the pelvis and partly the abdominal cavity, measuring 21.9 ´ 14.9 ´ 10.4 cm (Figs. 1 A–C.) The patient was qualified for abdominal subtotal hysterectomy via laparotomy. Because of the reduced Hb level and clinical signs of anaemia, due to which the operation had already been postponed once, after consultation with nephrologists and transfusiologists, 2 units of leukoreduced and irradiated packed red blood cells were transfused on the day of admission, resulting in an increase in Hb to 10.0 g/dl. On the same day, the patient underwent haemodialysis. Haemodialysis was also performed 2 days later – one day before the planned hysterectomy. After consultations with nephrologist, anaesthesiologist, and interventional radiologist, the surgical risk in this patient was qualified as extremely high and pre-operative UAE was planned to reduce this risk.
Fig. 1
Uterine fibroid filling the pelvis and abdominal cavity visible in computed tomography in frontal (A), axial (B), and sagittal planes (C)
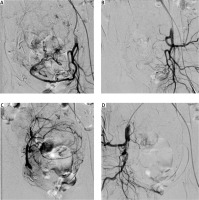
On the day of the procedure, double J stents were placed in both ureters, due to the high risk of injury during surgery because of the size and localisation of the fibroid. This was proposed by nephrologists because injury of the ureters would disqualify the patient from any potential future kidney transplantation she may require. To avoid urinary tract infection, the entire procedure was performed in perioperative antibiotic prophylaxis, proposed by nephrologists. Next, the patient was referred to the Department of Interventional Radiology and Neuroradiology to perform pre-operative UAE before a hysterectomy. The procedure was carried out under local anaesthesia. The right femoral artery was punctured with Seldinger Technique. A vascular 5 French sheath was inserted. Aortography was performed using a pigtail catheter placed at the level of kidney arteries. The contrast agent Visipaque 320 was administered in a volume of 30 ml with a flow rate of 15 ml/sec. Once the presence of the uterine artery was confirmed (Fig. 2 A), embolisation was performed (Fig. 2 B). Both internal iliac arteries were catheterised using a Roberts uterine catheter, then a microcatheter was used to selectively catheterise the uterine arteries (Figs. 3 A, C). Both uterine arteries had been embolised using Glubran 2 cyanoacrylate glue (a liquid embolic agent used to block blood vessels endovascularly) mixed with iodised oil (Lipiodol). The final aortography was performed to confirm the effectiveness of the treatment (Figs. 3 B, D). Immediately after UAE, a subtotal hysterectomy with bilateral salpingectomy was performed through a midline incision. Four units of leukoreduced and irradiated packed red blood cells and 4 units of fresh frozen plasma were secured for the surgical procedure. Blood loss during the procedure was estimated to be 300 ml; therefore, no decision was made to transfuse blood products in the perioperative period. The total duration of hysterectomy and general anaesthesia was 59 minutes. The total duration of double J stent placement, pre-operative UAE (both local anaesthesia), and hysterectomy (general anaesthesia) was 1 hour and 54 minutes (2 hours and 20 minutes including transport between departments). The haemoglobin level immediately after the procedure was 9.1 g/dl. One day after the procedure, the patient underwent haemodialysis. Both in the perioperative period and 30 days after the procedure, low-molecular-weight heparin at a dose of 40 mg was used for thromboprophylaxis. Typical pain management strategies were applied (morphine PCA, paracetamol, metamizole). During the entire hospitalisation period, the patient remained under constant nephrological supervision. The patient was discharged on the fifth day after surgery. The only postoperative symptoms were transient nausea and vomiting that appeared on the first day after the procedure and stopped after typical treatment with a proton pump inhibitor. The haemoglobin level at the time of discharge was 8.2 g/dl, so a decision was made to start oral iron supplementation for 30 days (ferrous sulphate – 80 mg per day). One month after surgery, the patient remains in good general condition. Complete resolution of the previously mentioned symptoms caused by uterine fibroid was achieved. After prescribed oral iron supplementation, an increase in haemoglobin level to 10.4 g/dl was achieved after 30 days. Histopathological examination confirmed the diagnosis of uterine fibroid (uterine leiomyoma).
Conclusions
The above case presents a method of reducing the risk of perioperative complications in a patient with giant uterine fibroid and high surgical risk. Among the possible treatment options for uterine fibroids (surgical procedures, pharmacological therapies, and minimally invasive procedures), in the above case, hysterectomy was the treatment of choice. However, surgical treatment in a patient with severe comorbid conditions and giant uterine fibroid carries a serious risk of perioperative complications. Pre-operative UAE allows us to reduce such risks by reducing blood loss during hysterectomy and shortening operation/anaesthesia time [5–7]. We are aware that all the procedures described above are not without risk. However, together with nephrologists and anaesthesiologists, we decided to apply unusual perioperative management to avoid critical deterioration of the patient’s medical condition caused mainly by hypovolaemic shock during the hysterectomy itself and prolongation of the general anaesthesia. In our opinion, this course of action was associated with lower risk.
The subject of discussion may be why a subtotal hysterectomy was performed instead of a total hysterectomy. Various methods of treatment were presented and explained to the patient, and even though a total hysterectomy was proposed to this patient, she only gave informed consent for a subtotal hysterectomy procedure. The patient was informed that subtotal hysterectomy would not reduce the risk of cervical pathologies in the future [9, 10]. During the operation, the fibroid localised low in the uterine isthmus was enucleated.
Another point of debate may be why Glubran 2 cyanoacrylate glue (a liquid embolic agent used to block blood vessels endovascularly) mixed with iodised oil (Lipiodol), and not polyvinyl alcohol (PVA) particles, was used in this particular case. First of all, as mentioned earlier, the patient suffered from HIV-associated nephropathy, and the results of renal parameters were already so critical that the patient was on regular dialysis. The use of PVA particles would involve the use of a much larger dose of contrast agent, which would unnecessarily burden the already ineffective kidneys. Moreover, because it was a preoperative UAE before the hysterectomy procedure, the use of cyanoacrylate glue mixed with iodised oil was faster and, above all, a much cheaper method in comparison to PVA particles. The primary goal was to remove the uterus and fallopian tubes, and pre-operative UAE was performed to reduce blood loss.
We are aware that there are already many papers in the literature regarding the use of pre-operative UAE before hysterectomy. However, we would like to present this case and the exact procedure that was used in this high-risk surgical patient. In this case, close cooperation between gynaecologists, interventional radiologists, nephrologists, and urologists was required. Without this, a regular hysterectomy procedure would be impossible to perform or would be associated with a high risk of complications.
Although the benefits of pre-operative UAE before planned myomectomy or hysterectomy in high-risk surgical patients with large fibroids have to be confirmed in well-designed clinical trial, this procedure seems to be a promising tool to reduce the risk of perioperative complications in such patients [5].