Clear cell papulosis (CCP) is a rare skin disease which predominantly develops in Asian population during their early childhood especially under 6 years old. Since it was first recognized by Kuo et al. [1], there have been more than 50 cases of CCP published in the literature. The disease is characterized clinically by a number of asymptomatic white or hypopigmented papules which are mainly in the lower part of the abdomen and pubic area. Histopathology is generally needed to make a definite diagnosis. Available non-invasive imaging techniques in dermatology show opportunities to assist diagnosis of this skin disease. Dermatoscopic features of CCP have been reported by Leerunyakul et al. [2]. Reflectance confocal microscopy (RCM) enables capture of cellular-resolution images of lesions, parallel to the skin surface, at different depths from the stratum corneum to the superficial dermis in vivo, which is a promising imaging tool for the histological evaluation of skin structures in vivo. It has been extensively studied for use in evaluation of cutaneous neoplasms to decrease the biopsy of benign lesions [3]. However, to our knowledge, the RCM findings of CCP have not been previously described in the literature. Herein, we report the RCM features and their histological correlations in CCP.
A 28-month-old girl presented with a 6-month history of asymptomatic hypopigmented papules on the abdomen and pubic skin (Figure 1). The lesions had been increasing in number over time. There was no history of prior rash or trauma in the area. She was otherwise healthy without any pertinent medical or family history. The lesions were given no treatment before she was referred to the dermatology department. On examination there were multiple 2–3 mm, fat-topped, oval hypopigmented papules on the abdomen and pubic skin, which appeared to cluster around the milk lines. Some papules showed a tendency to coalesce. On reflectance confocal microscopy, we discovered the appearance of singly round target shaped cells almost two times larger than the neighbouring keratinocytes near the basal layer of the epidermis (Figure 2 A). Histopathologic examination reviewed a proliferation of oval to round cells with abundant clear cytoplasm arranged singly along the basal cell layer of the epidermis (Figure 2 B), which corresponded to the reflectance confocal microscopy. By immunohistochemistry, these clear cells were positive for CEA, EMA and CK7, but negative for Melan-A and SOX-10. The histopathological and immunohistochemical findings confirm the diagnosis of CCP. The patient was given regular follow-up without treatment. Over a 14-month follow-up period, no significant change of the lesions was noted.
Figure 1
Multiple 2–3 mm, fat-topped, oval hypopigmented papules on the abdomen and pubic skin, which appeared to follow the milk lines

Figure 2
A – Confocal 0.5 × 0.5 mm image of the epidermal layer showing with bright single cells centred in dark holes, appearing as ‘target’ structures (red arrows) near the basal layer of the epidermis in our case of CCP. B – Histopathology of the lesion revealing a proliferation of oval to round cells with abundant clear cytoplasm as clear cells (yellow arrows) arranged singly along the basal cell layer of the epidermis. H&E, 400×
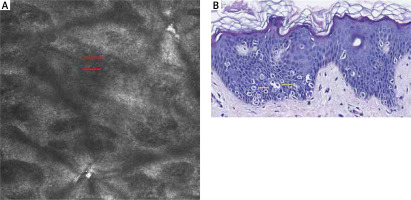
The pathogenesis of CCP is still not exactly elucidated. The hypopigmented change may be related to reduced melanization in the epidermis or dysfunction of melanocytes. Due to the distribution along milk lines and the presence of clear cells in lesions, a histogenetic relationship with Toker cells has been suggested. Some reports have suggested that CCP is a benign counterpart to extra‐mammary Paget’s disease and may be transformed via Toker cells [4]. However, a long-term follow-up study of CCP by Tseng et al. demonstrated that there is no direct relationship between CCP and mammary Paget’s disease/extra-mammary Paget’s disease [5]. More investigation is still needed to determine its pathogenesis. The most characteristic histologic feature of CCP is the presence of clear cells along the basal and suprabasal layers of the epidermis. The clear cells were larger than the adjacent keratinocytes, with ample clear cytoplasm and pale round nuclei. The clear cells of CCP have histologic and immunohistochemical similarities with both Toker cells and Paget cells. For our patient, we discovered the appearance of round target shaped cells larger than the neighbouring keratinocytes near the basal layer of the epidermis by RCM in a pattern similar to that observed in pathology. The RCM features of CCP has similarities with Paget’s disease. However, round target shaped cells of CCP are always scattered, without any disordered epidermal structure, appearance of high-refractive dendritic cells, abnormal honeycomb appearance in the basal layer, as well as tortuous blood vessels in the superficial dermis, which are distinguished from Paget’s disease [6].
CCP could be distinguished from other hypopigmented dermatoses including papular elastorrhexis, papular scars, postinflammatory hypopigmentation, vitiligo, nevus depigmentosus, tinea versicolor, and hypopigmented mycosis fungoides based on its clinical characteristics: 1) the age of onset, 2) lesions’ distribution, size and amount, 3) the benign behaviour nature, 4) no evidence of inducement, as well as its typical histopathology. As the dermatoscopic features of CCP represented as depigmented homogeneous structureless area macules with smooth surface and irregular borders, without other abnormal structure and colour, our findings of RCM for CCP are more sensitive. In this case, we demonstrated that singly round target shaped cells larger than the neighbouring keratinocytes near the basal layer of the epidermis correspond to clear cells.
In conclusion, our study demonstrated that RCM could be helpful to detect the histologic clues of CCP. If confirmed on a larger series, RCM might address the diagnosis, when invasive biopsy is not easy to accept for patients.








