The physiological transformations accompanying pregnancy, compounded by the implications of obesity, pose intricate challenges for anaesthesiologists attending to obese parturients [1]. This group of patients is clinically challenging and can be considered as one of the most difficult periope-rative case scenarios [2]. Obesity is prevalent in all age groups [3] and socio-economic groups [4]. It is especially concerning in women of childbearing age because maternal obesity is also dangerous to the foetus and makes them prone to complications. Multi-disciplinary management is now integral to managing the obese pregnant patient, and detailed planning is essential [5]. Anaesthesiologists working in obstetric departments always aim to implement the safest mode of analgesia and/or anaesthesia to an obese parturient, which should always be guided by best evidence-based practices.
Epidural analgesia is the gold standard for relieving the pain experienced while giving birth. Several studies have been undertaken worldwide to improve the success rate of epidural catheter insertion and make the experience as smooth as possible for the parturient [7]. However, in an obese parturient such intervention may be particularly challenging. Additionally, not all centres are adequately equipped with resources and staff, making both providing adequate care and carrying out clinical trials difficult [8]. Thus, the available literature on providing adequate analgesia in obese parturients is not vast, and this population remains to be studied extensively. We believe that, as challenging as it may be, it is the prime duty of anaesthesiologists and obstetricians to work together and come up with the best practices that can be followed safely in any obese parturient. Thus, we aimed to compose a narrative review with a comprehensive summary of all possible complications and safe anaesthesia practices to follow in these patients. We have also included recommendations from the experiences at our tertiary care centre, spanning over a decade.
STUDY DESIGN
Narrative reviews are helpful in complex fields where relevant literature for any particular study can be diverse, and yet the researcher aims to address the length, width, and depth of a question. Labour analgesia is one such field. Unarguably, remarkable work is being done in this field, but because obesity is a highly prevalent issue in the world population, it is the need of the hour to make labour analgesia as free of any difficulties and complications as possible for an obese parturient.
METHODS
We divided this review into 7 steps, which were followed methodically:
identifying and formulating a research question,
search for relevant published articles in PubMed and Google Scholar,
eliminating duplicate articles,
refining inclusion criteria and selecting final arti-cles,
extracting all the relevant data from each selected study,
collection, assimilation, drawing interpretation and inference,
reporting the conclusion.
OBJECTIVES
After performing a preliminary search of the lite-rature, we formulated the following research question: In obese parturients, what are the anticipated and unanticipated complications of epidural analgesia, and how can we impart it safely? This question was formulated to collate all the published data and report a comprehensive set of safety measures incorporated by all practicing and in-training anaesthesiologists.
INCLUSION CRITERIA
We selected all the published articles on obese (BMI ≥ 30 kg m–2) parturients who were given epidural analgesia as the preferred mode of pain relief during labour. We used the World Health Organization (WHO) classification of obesity.
The peripartum period was defined as the period from the initial pre-anaesthesia check-up (PAC) before inserting the epidural catheter to the final step of care provided by the anaesthesiologist following delivery.
Our primary focus was on randomised controlled trials (RCTs). Systematic reviews and meta-analyses were excluded. We did not restrict the sample size or number of studies that could be included.
INFORMATION SOURCES AND SEARCH STRATEGY
The search strategy was developed and advised by practicing anaesthesiologists who are well versed in conducting reviews. The electronic databases PubMed and Google Scholar were searched with keywords (Appendix 1). We included articles published only in English, restricted to the last 5 years.
Two anaesthesiologists reviewed the identified articles according to inclusion and exclusion criteria. Articles were screened by reading the title and abstract using the predetermined criteria. The selected articles were grouped into the ‘included’ and ‘reconsider’ category. The excluded articles were also reviewed to ensure that the exclusion criteria were met properly.
Following this stage, the complete text of all the selected studies was read to identify the complications encountered and safety measures used successfully (or unsuccessfully) by the anaesthesio-logists. We reviewed the included articles to ensure no additional relevant article was missed.
DATA CHARTING AND ASSIMILATION
A table was prepared with headings and sub-headings meant to facilitate data extraction.
RESULT GENERATION
This was achieved by preparing a summary of all important details in included studies and a detailed narration explaining the interpretation of the results. Attempts were made to identify significant and useful interventions. We also aimed to find gaps and suggest management ideas that can be applied to resource-limiting settings and can prove highly useful.
Selection
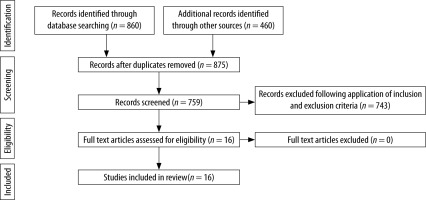
The PubMed and Google Scholar databases were searched for records from 2018 to 31 July 2022. After going through the title and abstracts of these articles and removing duplicates, 16 articles were selected that fit our inclusion criteria (Figure 1). Out of these, 12 were selected from PubMed and 4 from Google Scholar. We also reviewed the refe-rences of the review articles that appeared in our search results to ensure that no relevant study was missed, but no new research was identified.
Characteristics
Relevant details were extracted from these studies and were tabulated under the following headings – Author, Year, Country, Set-up, Study design, Subjects, Sample size, Outcomes, Results, and Conclusion. Each study was reviewed independently by 2 authors. Of the 16 studies, 15 reported data collection in a single country. One study reported data collection in 2 countries (Australia and New Zealand). Nine studies were reported from the USA. These 16 studies reported a total of 5702 participants (Table 1) [9, 24].
TABLE 1
Details of various articles on safety and complications of epidural labour analgesia in pregnant women
| Author, year | Country | Setup | Study Design | Classification of obesity | Number of patients/participants | Outcomes | Results | Conclusion |
|---|---|---|---|---|---|---|---|---|
| Tan et al. [9], 2022 | USA | Tertiary Healthcare Centre | RCT | BMI > 35 kg m–2 | 132 (66 per group) | Primary outcome was a composite of (1) asymmetrical block, (2) epidural top-ups, (3) catheter adjustments, (4) catheter replacement, and (5) failed conversion to regional anesthesia for cesarean delivery. Secondary outcomes time to a pain score of 1 or less, sensory levels at 30 min, motor block, maximum pain score, patient-controlled epidural analgesia use, medication consumption, duration of the second stage of labor, delivery mode, fetal heart tone changes, Apgar scores, maternal adverse events, and satisfaction with analgesia. | No statistically or clinically significant differences between the dural puncture epidural and standard epidural groups in the primary composite outcome (P = 0.766), its components, or any of the secondary outcomes. | A lack of differences in quality of labor analgesia between the dural puncture epidural and standard epidural in this study does not support the routine use of the dural puncture epidural technique in obese parturients. |
| Rote et al. [10], 2022 | USA | Tertiary Referral Centre | Retrospective and prospective quasi-experimental design | BMI 30 kg m–2 or greater | Retrospective – 373 Prospective – 50 | To assess the efficacy of an ultrasound-assisted technique and its use in minimising procedural complications in the obese parturient receiving neuraxial anaesthesia. | Significant decrease in procedural time for ultrasound-assisted epidural placement (P = 0.034), but no difference in subarachnoid blocks (P = 0.892). | Implementing an ultrasound-assisted technique for obese parturients receiving epidural anaesthesia reduced procedural time, zero paresthesias, and post-dural puncture headaches. |
| González-Tascón et al. [11], 2021 | Spain | Tertiary care Healthcare Centre | Retrospective observational descriptive study | BMI > 30 kg m–2 | 3653 | Variables related to the difficulty and complications of performing the technique and to analgesia failure rate. | Neuraxial techniques are difficult to be performed in obese obstetric patients, as shown by the number of puncture attempts (≥ 3 in 9.1% obese versus 5.3% in non-obese being, P < 0.001), but the incidence of complications, as haematic puncture (6.6%) and accidental dural puncture (0.7%) seems to be similar in both obese and non-obese patients. | An early performance of epidural analgesia is essential to control labor pain and avoid general anaesthesia in such high-risk patients. |
| Arnolds et al. [12], 2021 | USA | Tertiary Referral Centre | Retrospective study | BMI > 50 kg m–2 | 233 | Primary outcome was the failure rate of the first neuraxial catheter. Secondary outcomes were failure rates by neuraxial technique, at cesarean delivery, and rate of catheter replacement. | Thirty-two of 233 neuraxial catheters failed (13.7%). Epidural catheters placed using CSE or dural puncture epidural had a lower failure rate than those placed without dural puncture (9.2% vs. 28.6; P < 0.001). Catheter migration was documented for 29.4% (95% CI: 16.8–46.2%) of catheters that failed. | Epidural catheters placed using CSE or dural puncture epidural techniques were more reliable than those placed without dural puncture in super-obese parturients. Catheter migration was a major source of failure. |
| Chen et al. [13], 2021 | China | Tertiary Referral Centre | Randomised controlled study | Obese: BMI > 27 kg m–2 Control: BMI < 27 kg m–2 | 60 | The primary outcome was the effect of epidural ropivacaine when combined with dexmedetomidine for labor analgesia. Secondary outcomes were VAS score before administration, duration of first, second, and third stage of labor, parturient self-control degree, parturient satisfaction and amount of blood loss. | When co-administered with dexmedetomidine, EC50 of ropivacaine 0.095% (95% confidence interval [CI]: 0.090–0.100%) in control group vs. 0.070% (95% CI: 0.062–0.076%) in obese groups. (P < 0.001). EC95 values of ropivacaine 0.084% (95% CI: 0.077–0.122%) in control and 0.106% (95% CI: 0.101–0.128%) in obese group. | Patients with antepartum obesity may require decreased ropivacaine concentration for epidural labor analgesia when co-administered with 0.5 μg mL–1 dexmedetomidine. |
| Hoang et al. [14], 2021 | USA | Tertiary Referral Centre | Prospective study | – | 18 anaesthesia providers | To create a best-practice recommendation by bridging the gap in knowledge for anaesthesia providers concerning ultrasound technology and epidural placement in obese labouring patients. | Using ultrasound to help place the epidural in an obese parturient more accurate than using the traditional blind technique alone. | Placing an epidural catheter under ultrasound guidance improves overall patient satisfaction and outcomes in the obese parturient. |
| Vernon et al. [15], 2020 | USA | – | RCT | BMI > 40 kg m–2 | 16 | The primary outcome catheter placement time, defined as the time of palpation or ultrasound preparation, until epidural needle exit time. | Ultrasound evaluation took more time than palpation (1.8 ± 0.6 vs. 0.9 ± 0.1 min respectively; P < 0.001) Reduced placement time (mean 4.3 ± 3.5 min using ultrasound vs. 10.1 ± 5.4 min using palpation, P = 0.03), fewer attempts (median 1 attempt with ultrasound vs. 5 attempts with palpation; P = 0.02). Mean total procedure time in the ultrasound group was 6.1 ± 3.5 min compared to 11.0 ± 5.3 min in palpation group (P = 0.05). | Ultrasound-guided landmark clarification and needle insertion for epidural labor analgesia by an experienced provider in morbidly obese patients are associated with reduced placement procedure time. |
| Loebig et al. [16], 2020 | USA | Tertiary Referral Centre | Prospective, online survey | Obese parturients, BMI ≥ 35 kg m–2 | Survey distributed to 1882CRNAs and SRNAs; 109 respondents | To determine their knowledge, access, and perceptions of ultrasound used for epidural and spinal needle placement in obese parturients. | Of the 109 respondents, 100% agreement that ultrasound was helpful in needle placement when landmarks were indistinguishable. Barriers included a lack of knowledge, equipment, and privileges. | The survey data showed that CRNAs who utilised ultrasound for epidural/spinal needle placement found it useful; however, they did not find it necessary in every case despite the parturients size. |
| Ni et al. [17], 2020 | Japan | Tertiary Referral Centre | Randomised controlled study | BMI >30 kg m–2 | 80 | The primary outcome was the first insertion success rate. Secondary outcomes were the time taken to identify the needle puncture site, duration of procedure, the total time, parturients who require needle redirections, the number of skin punctures, changes in the intended interspace, and the incidence of complications. | Compared to the palpation group, the first insertion success rate was significantly higher in ultrasound group (72.5% vs. 40.0%; P = 0.003), and time taken to identify the needle puncture site was less (30 [26–36] vs. 39 [32–49] seconds; P = 0.001) in the ultrasound group. The rate of parturients who required needle redirections (40.0% vs. 72.5%; P = 0.003) and the incidence of paraesthesia was both lower (7.5% vs. 45.0%; P < 0.001) in the ultrasound group. | The Accuro ultrasound device can enhance the efficacy and safety of epidural anaesthesia in obese parturients. |
| Bright et al.[18], 2019 | Australia | Tertiary Referral Centre | Retrospective cohort study (over 5 years, single-centre) | Booking weight of parturients > 140 kg or BMI greater than 50 kg m–2 | 127 | To assess the anaesthesia, maternal and neonatal outcomes of women with extreme obesity delivery at the Royal Brisbane and Women’s Hospital (RBWH). These results were compared with published data for Australia and New Zealand | 79 (62.2%) delivered by caesarean delivery; 40 (31.5%) were elective deliveries. Neuraxial anaesthesia was the preferred technique, used in 76 women (96.2%), with 7 (9.2%) of these neuraxial blocks converted to GA. Of the 78 women commending active labor, 47 (60.3%) used epidural analgesia. 65 (50%) neonates were admitted to NICU. | A high rate of cesarean delivery and use of labor epidural analgesia compared with the general population, but similar to population-based data for obese women from Australia and New Zealand. A high proportion of neonates required admission to NICU. |
| Arnolds et al. [19], 2019 | USA | Tertiary Referral Centre | Retrospective study | BMI > 50 kg m–2 | 125 | The primary outcome was the percentage of catheters placed at or above L1/L2, determined by reviewing the retained foreign object radiograph. Secondary outcomes were agreement between the estimated and actual catheter location and subgroup analysis of catheters placed under ultrasound guidance. | Unintentional high placement occurred in 26/125 (21%; 95% CI: 15–29%) patients. Poor agreement between the estimated and actual catheter location (27% accurate, unweighted κ-statistic 0.02). 11 of 39 catheters placed with ultrasound (28%; 95% CI: 17–44%) were at or above L1/L2 compared with 15/86 catheters placed without ultrasound (17%; 95% CI: 11–27%). | A high rate of inadvertently high epidural or intrathecal catheter placement occurs in super-obese parturients. Ultrasound did not prevent this. |
| Canturk et al. [20], 2019 | Turkey | Tertiary Referral Centre | Prospective observational study | All parturients between May 2018 to August 2018 | 130 | To assess the correlation between ultrasound-estimated epidural depth (ED) with abdominal girth (AG), BMI, weight, height, and age. | Correlation coefficients: - between ED and AG were 0.797 (95% CI: 0.727–0.854, P < 0.001); - between ED and BMI were 0.543 (95% CI: 0.405–0.661, P < 0.001); - between ED and weight were 0.593 (CI = 0.466–0.695, P < 0.001). | Abdominal girth has a strong correlation with ultrasound-estimated epidural depth in parturients. |
| Rajagopalan et al. [21], 2019 | USA | Tertiary Referral Centre | Prospective observational study | Labouring parturients | 373 | First attempt success and Time to epidural placement. Variables studied: - BMI - Well palpable spinous process - Experience (> 20 epidural placements) | Mean BMI at the time of placement was 34. The first attempt success rate for the placement of epidural was 67% (n = 273). Women with well palpable spinous process were 3.3 times more likely to have a successful first attempt placement irrespective of the provider experience or BMI [3.39 (1.77–6.51), P < 0.001]. The time to placement was shorter in patients with good anatomical landmarks [1.58 (1.20–2.07), P < 0.001) and when performed by a trainee who had completed a minimum of 20 epidural procedures [1.57 (1.26–1.94), P < 0.001). | Inability to palpate the spinous process contributes to multiple attempts at epidural placement. |
| Eley et al. [22], 2018 | Australia | Tertiary Referral Centre | Prospective, 2-centre, case-control study | BMI > 40 kg m–2 vs. BMI < 30 kg m–2 | 100 (2 groups of 50 each) | Primary outcome failure of the labor epidural to be used as the primary anaesthetic technique. | Odds ratio (OR) of epidural extension failure was 1.69 in Group O (BMI ≥ 40 kg m–2) vs. Group C (BMI ≤ 30 kg/m–2) (20% vs. 13%; 95% CI: 0.88–3.21, P = 0.11). Risk factors for failure in obese women included ineffective labor analgesia requiring anaesthesiologist intervention (OR 3.94, 95% CI: 1.16–13.45, P = 0.028) and BMI > 50 kg m–2 (OR: 3.42, 95% CI: 1.07–10.96, P = 0.038). | The failure rate of epidural extension did not differ significantly between the groups. |
| Capogna et al. [23], 2018 | Italy | Tertiary Referral Centre | Prospective study | Difficult obstetric cases | 30 + 56 Study conducted in two parts | I part: Primary endpoint – successful concordance of identification of the ligamentum flavum and the epidural space during a standard epidural procedure. II part – to study the utility of CompuFlo® in difficult epidural placement. Primary endpoint was successful epidural placement after previous unsuccessful epidural insertion without the device. | In all cases, epidural analgesia was successful, and no complications were noted. Good correlation between the operator-s feelings and the delta of pressure recorded by the CompuFlo® for identifying the ligamentum flavum and the epidural space (Rho = 0.79; tau = 0.67). In the second part of the study, all the difficult blocks performed with the CompuFlo were successful after a single attempt. | CompuFlo was validated as a tool to identify the epidural space. It may also assist trainees in successful epidural placement in difficult cases. |
| Song et al. [24], 2018 | USA | Tertiary Referral Centre | Retrospective study | Obese parturients | 17,497 records reviewed | To determine whether obesity is associated with fewer PDPHs after an accidental dural puncture (ADP) during epidural placement for labor analgesia. | 164 patients identified who had an ADP. Of these, 51.2% developed PDPH, 35.7% of those with a PDPH required an epidural blood patch due to a persistent headache. Analysis found no statistical difference between the different BMI groups, the rate of PDPH after ADP with an epidural needle, and the severity of headache. | High BMI was not protective for developing PDPH after ADP in parturients who had a vaginal delivery with epidural analgesia. |
One study was carried out as an online survey where the questionnaire and study material were distributed to 1882 nurse anaesthetists, of whom 109 responded, and their knowledge, access, and perceptions towards using ultrasound for epidural needle placement in obese parturients were assessed [19]. In total, we found 5 retrospective studies, 10 prospective studies, and one was carried out in 2 parts: retrospective followed by prospective.
DISCUSSION
Obesity is an excessive or abnormal fat deposition that poses a serious health concern. The World Health Organization (WHO) defines and classifies levels of obesity based on BMI, as summarised in the table below [25] (Table 2).
TABLE 2
Classification of obesity
| BMI (kg m–2) | Classification |
|---|---|
| 18.9–24.9 | Normal |
| 25.0–29.9 | Overweight |
| > 30.0 | Obese |
| 30.0–34.9 | Class 1 |
| 35.0–39.9 | Class 2 |
| > 40.0 | Class 3 |
| 40.0–49.9 | Morbid obesity |
| 50.0–59.9 | Super obesity |
| > 60.0 | Super-super obesity |
There is no range defined as optimal for weight gain during pregnancy. The above classification is used to stratify the risk of pregnant women presenting to the clinics.
Significant complications associated with maternal obesity [26] are mentioned in the table below (Table 3).
TABLE 3
Maternal and neonatal complications associated with obesity
This narrative review highlights the current latest evidence relevant to anaesthesiologists who work with obstetric patients. We focussed on the best evidence-based interventions for obese patients receiving labour epidural analgesia. By identifying studies on safety and complications of labour epidural analgesia in obese parturients, this review also identifies areas for future research.
An obese parturient presents with the challenges associated with physiological changes of pregnancy and pathological changes of obesity [27]. When a pregnant woman presents to the antenatal clinic for their third trimester follow-up, we propose that a formal reference should be sent to a senior anaesthesiologist to examine the patient and document labour analgesia, delivery, and anaesthesia plan, if required. The ideal option for labour analgesia for an obese parturient is via neuraxial technique [29], which includes an epidural catheter (EC), combined spinal-epidural (CSE), dural puncture epidural (DPE), and intrathecal catheters (ITCs).
Pre-anaesthesia check-up
A pre-anaesthetic check-up is an opportunity for the clinician to inform and educate about labour epidural analgesia, anticipate, inform, and discuss any complication that may arise, and be well prepared for it in advance. It also provides time for the parturient to present her queries, which should be addressed by the anaesthesiologist so that an informed decision about labour epidural analgesia can be made.
The anaesthesiologist should undertake a routine history focusing on screening for potential comorbidities linked to obesity, like obstructive sleep apnoea (OSA), cardio-vascular illnesses, diabetes, and the risk of aspiration due to gastroesophageal reflux [28]. A thorough examination of the airway, cardiovascular, and respiratory systems, and spine should also be undertaken. Pedal oedema and dyspnea on exertion are usual features of pregnancy that are difficult to distinguish from an underlying cardiovascular illness, so it is advised that the anaesthesiologist should keep a low threshold to order an electrocardiogram and/or echocardiography when the patient is obese. Examining the spine can point towards the difficult placement of labour epidural catheter and neuraxial anaesthesia because palpation of inter-vertebral spaces is difficult in these patients due to increased sub-cutaneous tissue. Findings should be documented, and preparation should be made accordingly because the patient may require the assistance of ultrasound for the same.
Preparation
It is advocated that anaesthesiologists should ensure the availability of adequate equipment and adequately trained staff to manage an obese parturient in the labour unit. We recommend checking for transfer equipment like air mattresses and patient lifts, difficult airway carts, ultrasound machines, long spinal and epidural needles, appropriately sized cuffs for non-invasive blood pressure (NIBP) measurement, appropriately sized gowns and pneumatic compression devices, and invasive arterial monitoring, in cases with cardiac disorders. The weight-bearing capacity of operation theatre tables and wheelchairs should be appropriate. At the same time clear communication should be maintained with the obstetric team. Prior interaction with an anaesthesiologist will help to assure the parturient that all measures to ensure the safety of the mother and her baby are in place.
Placement of epidural catheter
Placing an epidural catheter in obese patients can be challenging. We recommend that the epidural catheter be placed as early in labour as possible as the patient will be calm and cooperative, which helps in her positioning, palpation of landmarks, and placement of the catheter. The preferred position in most studies was sitting, with the spine flexed, allowing better palpation. Multiple attempts may be required, and there are high chances of failure of epidural; therefore, the patient should be well informed about it. If ultrasound assistance is needed, it can be arranged in time.
In 2021, a retrospective study by González- Tascón et al. [11] analysed data of 3653 obese parturients and studied the variables related to the difficulty and complications of epidural catheter placement, and they observed that complications like multiple attempts and incidents of caesa-rean delivery are more common in obese patients as compared to non-obese parturients. However, they found no difference in incidences of haematic punctures and accidental dural punctures. Thus, the authors strongly recommended that epidural catheters be sited early in these patients.
Equipment
In parturients with extreme obesity, a longer needle may be required and should be available. Since most anaesthesiologists are used to the standard- length needle, handling a longer one may prove challenging. Counselling and communicating with the patient while placing the catheter makes her less anxious and helps in proper positioning. If the patient is sitting with her spine flexed, ask her to sit upright before fixing the catheter because it could be drawn inwards due to the increased subcutaneous tissue. There is no definitive evidence on whether a high BMI is protective against post-dural puncture headache, as supported by a retrospective study by Song et al. [20] in which records of 17,749 obese parturients were reviewed, out of which 164 had an accidental dural puncture.
Ultrasound assistance
Many studies have been done in which a determination of anatomical landmarks and depth of epidural space was performed with the help of ultra-sound. Hoang et al. [17] provided educational modules to 18 anaesthesia providers on the use of ultra-sound for epidural needle placement in obese parturients, and 100% of subjects found it helpful to be inculcated in the best-practice recommendation. Vernon et al. [9] used it for landmark identification and needle insertion, but the procedure time was increased. On the other hand, Rote et al. [18] concluded that ultrasound use decreased the overall procedure time. Accuro ultrasound (Rivana medical, Charlottesville, VA, United States), a device used by Ni et al. [21], when used by experienced anaesthesio-logists, can enhance the safety and efficacy of epidural needle placement. Additionally, a prospective study by Capogna et al. [15] in 2018 validated CompuFlo as a tool to identify epidural spaces in complex obstetric cases.
On the other hand, Arnolds et al. [13, 22] observed high chances of inadvertent high epidural catheter placement in obese patients, which could not be prevented by ultrasound. This disparity in results is thought to be mainly because of differences in operator expertise, and though ultrasound is mostly found to be useful, it is not considered necessary in every case, despite the parturient size, as seen in a survey conducted by Loebig et al. [19] in 2020. Never-theless, we believe that anaesthesiologists should be trained in using ultrasound for labour epidural catheter placement.
Comparing techniques of epidural analgesia
A recent study by Tan et al. [10] compared the dural puncture epidural (DPE) technique with standard epidural catheter placement in 132 parturients but could not find any significant difference between the 2 techniques. However, in a retrospective study by Arnolds et al. [13], the failure rate of the neuraxial catheter was studied in 233 super-obese parturients, and it was concluded that epidural catheters placed via CSE or DPE were more reliable than the ones placed without dural puncture in obese parturients. A major source of failure was the migration of the catheter.
Continuous epidural infusion, patient-controlled epidural analgesia, and programmed intermittent epidural bolus are widely used modes of delivering local anaesthetic via the epidural catheter. However, none of these maintenance techniques have been compared in obese pregnant women.
Post-procedure care and precautions
Routine assessment should be done to ensure the proper functioning of epidural catheters, and timely remedial and rescue measures should be taken if it is not working properly or if the patient is not satisfied with it. An otherwise healthy obese parturient can be managed in the labour room itself, and the epidural catheter can be used to provide analgesia. Prophylaxis against venous thromboembolism should be initiated.
CONCLUSIONS
Through this review, we recommend setting up a well-documented institutional protocol for obese parturients presenting in labour, which considers all the latest global advancements but also incorporates indigenous measures and locally procured pieces of equipment to set up a fully functioning, safe obstetric unit. Future research can be undertaken in the field of labour epidural analgesia in obese parturients concerning the available safety equipment, training of personnel, mode of delivery of local anaesthetic, and simulation models of obese parturients on which difficult neuraxial catheter placement can be practiced and troubleshooting can be done.