Purpose
Following radical prostatectomy (RP), approximately one-third of patients present with a local recurrence (LR) within ten years [1]. Positive surgical margins and extra-prostatic tumor extension are risk-factors for LR. In such patients, adjuvant external beam radiation treatment (EBRT) improves biochemical progression-free survival (bPFS) [2-4]. However, more recent data suggest that adjuvant and early salvage irradiation have similar outcomes [5-8]. The optimal radiation dose for such patients has not been optimally defined, but 66 Gy dose is considered adequate, with higher doses possibly required for macroscopic disease [1]. Significant late genitourinary toxicities are frequent after adjuvant or salvage EBRT. However, rates of genitourinary toxicities are lower with salvage irradiation in comparison with adjuvant irradiation [5, 7].
There are very few reports in the literature on the use of interventional radiotherapy (IRT) with interstitial high-dose-rate (HDR) brachytherapy in salvage irradiation for LR after RP without distant metastases. In majority of patients, this method was used as a boost combined with EBRT, except for one recent study [9-12]. On the contrary, salvage low-dose-rate (LDR) seeds were mostly used without EBRT [13-18]. Following RP and EBRT as adjuvant or salvage treatment, it is challenging to choose a further local treatment. Most patients would be offered hormonal treatment (HT) on palliative basis [1, 19]. Few small studies included patients who were treated with LDR brachytherapy seeds after EBRT [13, 17, 18]. These studies reported modest control rates and remarkably, there were no additional toxicities after using LDR brachytherapy seeds. In most recent study by Le Roy that included five patients, there were no late grade 2 or more toxicities observed [18]. Data on salvage stereotactic radiotherapy (SBRT) with ultra-hypofractionation to the prostate bed recurrence after previous EBRT remains limited despite recent availability of mostly retrospective reports [20]. The rates of late ≥ grade 2 genitourinary toxicities ranged between 11.1-26.3% [21-23]. The reported biochemical recurrence-free survival rates at 1-year and 2-year were 79% and 56%, respectively [22].
Cryoablation and high-intensity focused ultrasound (HIFU) have been proposed as salvage treatment options after primary irradiation with modest results [24-26]. A small report investigated the role of salvage HIFU for biopsy-confirmed LR after RP in 4 patients, of whom 3 received EBRT. There were no treatment-related complications [27].
HDR-IRT is a highly conformal technique of irradiation that enables a high-dose escalation with extreme hypofractionation. The sharp dose gradient ensures sparing of organs at risk (OARs). Therefore, HDR-IRT is considered a suitable salvage option for radiation recurrent prostate cancer [28-30].
The present study reported on the technical feasibility, safety, and efficacy of HDR-IRT as a salvage local treatment after RP and subsequent EBRT.
Material and methods
Patients
All medical records of prostate cancer patients who were treated with salvage HDR-IRT from January 2010 to December 2020 were reviewed. Only patients with a history of prostatectomy and EBRT were included. All patients were evaluated through physical examination, magnetic resonance imaging (MRI) of the pelvis, and either an isotopic bone scan plus contrast-enhanced chest pelviabdominal computed tomography (CT, in 7 patients), or positron emission tomography/CT scan using choline (in 4 patients) or later prostate-specific membrane antigen (PSMA, in 3 patients). LR was histologically confirmed through a trans-rectal ultrasound (TRUS)-guided biopsy. Treatment decision for each patient was discussed by a multidisciplinary tumor board.
Before HDR-IRT, a compatibility check was performed. Contraindications included international prostate symptom score of more than 12, maximum urinary flow rate (Qmax) below 10 ml/s, pubic arch interference, infiltration of the rectum and/ or the bladder, and non-ability to sustain lithotomy position or anesthesia.
Interventional radiotherapy (brachytherapy)
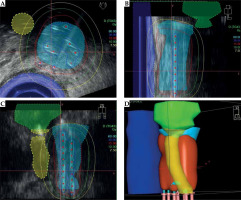
Under general anesthesia, the patient was placed in a lithotomy position. A Foley catheter was introduced and filled with aerated gel. The needles were inserted under TRUS guidance through a perineal template. A TRUS image-series with 1 mm slice thickness was captured and transferred to treatment planning system (Oncentra, Elekta-Brachytherapy, The Netherlands). Clinical target volume (CTV) and OARs, including rectum, bladder, and urethra were delineated. CTV comprised tumor volume as recognized on TRUS images with a safety margin (range, 2-5 mm), excluding OARs. Each patient received 30 Gy in two fractions of HDR-IRT, separated by 2 weeks. Figure 1 shows an example of 3D dose distribution.
Follow-up
Follow-up visits were scheduled every 3 months for 3 years, and then every 6 months. Biochemical failure (bF) following HDR-IRT was defined as a rise of 2 ng/ml or more above prostate specific antigen (PSA) nadir. In case of bF, further imaging studies (pelvic MRI/PET-CT scan) were performed to assess the cause of bF. Treatment-related toxicities were graded according to common terminology criteria for adverse events version 5.0.
Statistical analysis
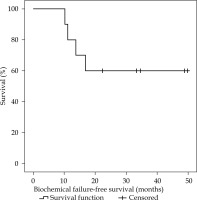
Results were reported as absolute value, median with range, or as mean with standard deviation. The duration of biochemical failure-free survival (bFFS) after HDR-IRT was measured from the date of biopsy-confirmed recurrence after EBRT until bF. Probability estimates of bFFS were calculated using Kaplan-Meier analysis. Statistical analyses were performed with SPSS version 20. (IBM Corp., USA).
Results
Patient and tumor characteristics
Ten patients received two fractions of 15 Gy as a salvage treatment for a local prostate cancer relapse after RP and subsequent EBRT. Table 1 summarizes initial patient and disease characteristics. All patients received EBRT as an adjuvant treatment (6/10), or as a salvage treatment for LR (4/10). The median interval between EBRT and HDR-IRT was 42 months (range, 15-117 months). The median age at HDR-IRT was 63 years (range, 59-74 years), and the median PSA value was 2.5 ng/ml (range, 0.4-2.7 ng/ml). The location of LR was perianastomotic in four patients, left seminal vesicle bed in four patients, and right seminal vesicle bed in two patients. Gleason score was upgraded in 2 patients. At the time of HDR-IRT, four patients were undergoing androgen deprivation therapy with luteinizing hormone-releasing hormone (LHRH) agonist.
Table 1
Patient and disease characteristics
HDR-IRT treatment characteristics
The mean volume of CTV was 21.2 cc (±7.9), the median number of needles was 8 (range, 7-12 needles), and the mean CTV D90 was 93.7% (±2.4%). The complete dosimetry parameters of HDR-IRT are summarized in Table 2.
Table 2
Dosimetry parameters of HDR-IRT
Treatment outcome and related toxicities
The median follow-up time was 34 months (range, 10-68 months). The PSA nadir value following HDR-IRT was reached within six months, with a median value of 0.2 ng/ml (range, 0.04-1.2 ng/ml). Following HDR-IRT, bF was encountered in four patients, in whom 3 patients showed a further progression of the local relapse and 1 patient experienced distant metastases. The mean time to PSA increase in these 4 patients was 13 months.
The median bFFS for all patients was not reached. One-year bFFS, 3-year bFFS, 4-year bFFS were 80%, 60%, and 60%, respectively (Figure 2). Two patients died from consequences of metastatic disease; the mean time of death was 66.4 months.
The recorded treatment-related acute toxicities were exclusively grade 1-2. Six patients had acute genitourinary toxicity, and two patients acute gastrointestinal toxicity. Late genitourinary toxicities ≥ grade 2 were documented in four patients, of whom two patients had grade 2 toxicity and two patients had grade 3 toxicity (non-infective cystitis). Two patients had late ≥ grade 2 gastrointestinal toxicities.
Discussion
The use of salvage HDR-IRT following RP and subsequent EBRT is a potentially curative option for patients with a gross LR without distant metastases. In different international treatment recommendations, this sub-group of patients usually receives HT with a non-curative intent [1,19]. Although after adjuvant or salvage EBRT, up to 28% of the patients would suffer from late genitourinary adverse events of grade 2 or more [7], and many patients would still pass the compatibility check before HDR-IRT. The high rates of late genitourinary toxicities following EBRT are probably due to the inclusion of the bladder-neck and the vesico-urethral anastomosis in treatment volumes.
Despite the strong evidence for the use of salvage EBRT in patients with bF after RP, most studies did not differentiate microscopic from macroscopic relapses [1, 19]. Patients treated with salvage radiation for biochemically recurrent prostate cancer after prostatectomy did not benefit from dose-intensified stereotactic radiation treatment (70 Gy) vs. standard 64 Gy in conventional fractionation [31]. However, in a sub-set of patients with macroscopic recurrence, dose escalation might be needed. Probably, patients with macroscopic recurrence would benefit from an approach combining both EBRT and HDR-IRT. As the dose of EBRT could be reduced, focal dose escalation to LR with HDR-IRT sparing the rest of the prostate bed could maximize disease control, and therefore, better treatment-related toxicities can be anticipated.
In the literature, only three reports investigated the use of this approach as a salvage treatment for a macroscopic LR after RP were published (Table 3). In the three reports, HDR-IRT was applied for dose escalation following a relatively moderate EBRT dose [9-11]. One recent study used HDR-IRT as a salvage treatment for macroscopic local recurrence after RP and EBRT [12] (Table 3).
Table 3
Published literature investigating the use of high-dose-rate interventional radiotherapy for the treatment of local relapse after radical prostatectomy
| Author(s), year [Ref.] | n | EBRT (Gy) (n) | HDR-IRT (Gy) (n) | Previous EBRT (Gy) (n) | Median follow-up in months (range) |
|---|---|---|---|---|---|
| Niehoff et al., 2005 [10] | 35 | 30 (21/35) 40 (14/35) | 2 × 15 (21/35) 2 × 15 (14/35) | None None | 27 (5-70) |
| Strom et al., 2014 [11] | 6 | 50.4 (4/6) 45 (1/6) None (1/6) | 2 × 9.5 (4/6) 2 × 9.5 (4/6) 4 × 9.5 (1/6) | None None 70 (1/6) | 9 (3-40) |
| Buchser et al., 2016 [9] | 13 | 37.5 (11/13) | 1 × 15 (11/13) 2 × 12 (2/13) | None 66 (2/13) | 7 (4-15) |
| Aghili et al., 2022 [12] | 15 | None (15/15) | 4 × 9 | 70 (median; range, 60-70) | 48 (12-132) |
| Our series | 10 | None (10/10) | 2 × 15 | 64 (median; range, 50-66) | 34 (10-68) |
The largest series by Niehoff et al. included 35 patients who received two fractions of 15 Gy HDR-IRT. These patients were divided into two groups according to the dose of EBRT: 30 Gy in 21 patients and 40 Gy in 14 patients. The mean time to PSA increase was 16 months and 10 months, respectively, without statistical significance. PSA progression-free survival was also similar between the two groups. No patient experienced grade 3 or 4 treatment-related toxicities [10].
Strom et al. published results of 6 patients treated with intensity-modulated radiation therapy to 45-50.4 Gy, followed by two fractions of 9.5 Gy HDR-IRT. At 9 months median follow-up, all patients showed undetectable PSA levels, with no severe treatment-related toxicities reported [11].
Buchser et al. analyzed treatment results of 13 patients. Eleven patients had a single session of HDR-IRT (15 Gy), followed by hypofractionated EBRT (37.5 Gy in 15 fractions). In two patients who had previous adjuvant EBRT, HDR-IRT was applied alone (2 × 12 Gy). After a median follow-up of 7 months, all patients showed an appropriate biochemical response, with no late grade 3 or 4 treatment-related toxicities observed [9].
In a recent study, the safety and efficacy of HDR-IRT for prostate bed recurrence after RP and subsequent EBRT were investigated [12]. Aghili et al. analyzed retrospectively 15 patients who underwent retropubic RP and received 70 Gy EBRT median dose, with 5 years median interval between HDR-IRT and EBRT. The patients were treated with 36 Gy in four fractions over two insertions, with 1 weak interval. At 48 months median follow-up, 13 patients were controlled locally and had no evidence of PSA increase. Three cases had grade 2 genitourinary toxicities after HDR-IRT during the first 6 months. Two patients had grade 3 genitourinary toxicities (urinary incontinency), and no gastrointestinal toxicities were reported [12].
Our patients as well as the patients reported by Aghili et al. differ from the patients analyzed in the preceding series, since they previously received a complete course of EBRT as adjuvant or salvage treatment after RP. This could explain the reported grade 3 genitourinary toxicities in in the current study as well as in the study by Aghili et al. Additionally, both the studies had considerably long follow-up periods (34 and 48 months) when compared with the preceding studies, in which the follow-up duration ranged between 7 and 27 months [9-12].
All patients in the current study showed a proper biochemical response; the median PSA value dropped from 2.5 ng/ml to 0.2 ng/ml within six months after HDR-IRT. Four patients showed biochemical failure with a mean time to PSA increase of 13 months. These results are comparable to that of Niehoff et al. study [10]. Aghili et al. reported biochemical failure in 2 of 15 patients at 22 and 26 months of salvage HDR-IRT, respectively [12]. Nevertheless, PSA increase may be due to a nodal or distant failure, and might not always reflect the status of local control.
Since all included patients had a prostatectomy, adopting a proper definition of bF was problematic. The definition of bF following prostatectomy was not approved by the interdisciplinary tumor board because the patients had a macroscopic recurrence treated with radiation treatment. Therefore, the committee’s decision was to apply the definition of bF following curative radiation due to the presence of gross prostatic tissues.
In the current study, three patients suffered from a progression of the LR volume combined with an increased PSA level without evidence of other regional or distant metastases. These patients were treated systemically with hormonal treatment. No further local treatment was offered, since the patients have received a previous EBRT with a median dose of 66 Gy and additional HDR-IRT dose of 30 Gy (EQD2 > 100 Gy), and further radiation treatment with LDR brachytherapy seeds or SBRT would have been highly challenging due to the high potential risk of radiation-induced complications.
Moreover, offering a further local treatment option for such patients may also provide an opportunity to omit or delay HT. Systemic complications of HT can negatively impact quality of life (QoL), including sexual problems, fatigue, psychological morbidity, adverse metabolic sequelae, and increased cardiovascular and bone fracture risk [32]. However, after curative brachytherapy for early-stage disease, there was no difference in cancer-specific QoL scores at five years of follow-up compared with pre-treatment scores [33].
In the era of individualized cancer treatment, patients with an isolated macroscopic LR should be identified from all patients having bF without distant metastases following RP. Such patients may benefit from further dose escalation, possibly through HDR-IRT. The recent advances in multiparametric MRI (mpMRI) and PSMA PET-CT/MRI scan could play a crucial role in identifying the isolated prostate bed recurrence after RP [34, 35]. Although mpMRI has a highly detailed anatomical analysis of the prostate bed, it has a lower sensitivity in detecting prostate bed recurrences at PSA levels < 0.5 ng/ml [36]. The sensitivity of mpMRI can be improved by an endorectal coil [37]. In a recent large meta-analysis of nearly 5,000 patients, the overall estimate of the positivity of PSMA PET-CT in the prostate bed was only about 28% [34]. The detection of LR using PSMA PET-CT is highly affected by its proximity to the urinary bladder [34, 35, 38]. Adding the benefits of both techniques in the form of PSMA PET-MRI with a specific mpMRI protocol for the prostatic bed, has doubled the rate of detected prostate bed recurrences compared with the standard PSMA PET-CT [38].
Despite the limitations of the current study, including small number of patients and retrospective analyses, HDR-IRT could offer an opportunity for a salvage local treatment with potentially curable intent in patients with an isolated macroscopic LR, following RP and subsequent EBRT. Further clinical studies are encouraged to investigate the role of HDR-IRT in the management of LR after RP.