Introduction
Hymenoptera (which includes bees, wasps, bumblebees, and hornets) stings are common in adults and children. In the general population, 56.6–94.5% of people report at least one sting in their lives [1]. Reactions of different severity may occur as a result of Hymenoptera stings. The most common are uncomplicated local reactions, typical of people who are not allergic to insect venom. In Hymenoptera venom allergy (HVA) large local reactions occur most often, with a frequency estimated at 2.4% up to 26.4% [2] of the general population. The prevalence of systemic allergic reactions after Hymenoptera stings ranges from 0.3% up to 7.5% in adults and up to 0.3% in children [3]. In Europe, HVA is the most common cause of severe allergic reactions in adults (48.2%) and the second cause of anaphylaxis in children (20.2%) [4]. The proper treatment, which should provide very high protection from future life-threating systemic reactions in patients with HVA, depends on the correct diagnosis and qualification for venom immunotherapy (VIT).
In the entomological picture Hymenoptera species differ between each other as to the leading characteristics as follows: a bee (Apis mellifera) – a brown insect with a moderate number of hairs on the trunk and abdomen; a wasp (Vespula spp.) – a bee-sized, yellow-black insect with few hairs on the body and without hairs on the abdomen; a bumblebee (Bombus) – larger and more hairy than a bee, with numerous yellow, white or red stripes; a hornet (Vespa) – twice the size of a wasp, with a slightly darker, reddish head and trunk. These are the most popular in the middle part of Europe. The other entomological genus – Polistes spp. are relevant due to allergic reactions in the Mediterranean region, but they have still weak representation in in middle-northern part of Europe [5].
Beside the classification of the type of reaction and confirmation of an IgE-mediated pathogenesis, the identification of the offending insect is one of the key points to make the right diagnosis [6, 7]. Information on the appearance and behaviour of the insect, retraction of the sting, natural death of the offending insect after the sting, presence of hives or nests in the nearby area, when available, should be documented from each subject, because these data are helpful to guide the diagnosis, and in future management including the selection of VIT [7]. In the follow-up it should be also the key point for the patient’s education on how to avoid subsequent stings.
The identification of the stinging insect may prove difficult for the patient and his/her family, as well as for the physician, including the allergy specialist, for several reasons. The stinging insect may be overlooked due to its small size and fast movements. Moreover, as the Hymenoptera insects are similar to each other, knowledge of the Hymenoptera physical features and its behaviours is crucial for the identification. In order to adequately address the needs for education in the correct identification of stinging insects, it is necessary to determine the scale of educational deficits in this area. To the best of our knowledge, there are no studies on both children and their parents’ ability to identify stinging insects.
Aim
The primary objective of this case-control study was to assess the accuracy of identifying insects by children with Hymenoptera venom allergy and their parents as compared with children without such an allergy and their parents. The secondary objective was to indicate variables affecting the accuracy of the identification.
Material and methods
The questionnaire-based study was performed in a tertiary paediatric medical centre – the Children’s University Hospital in Krakow. All the patients with HVA and their parents were recruited from the Department of Pediatrics, Pulmonology, Allergology and Dermatology. The subjects without HVA and their parents (some of them stung by insects in the past), to serve as control groups, were randomly selected from the patients and their caregivers who were present in the above medical units for medical reasons other than HVA.
The analysed group consisted of 102 children with confirmed HVA (according to current EAACI guidelines on allergen immunotherapy [8]) with their 102 parents and 98 children without HVA accompanied by their 98 parents.
A 7-item questionnaire survey, addressed separately to the child and his/her caregiver, consisted of 2 parts. The first part was dedicated to demographic data and the personal history of stings of the child and the accompanying parent, respectively. The second part consisted of 5 single-choice sub-questions referring to the recognition of insects presented in photos without captions. Demographics included age, sex, place of residence, current level of education in reference to children and the highest level of education obtained by parents. The sting history contained the questions addressed to the number of insect stings in the past, the kind of culprit insects (bee, wasp, hornet, bumblebee, or an unidentified insect) and the approximate dates of such stings for a child and for his/her caregiver, respectively.
The images were colour pictures depicting the following, typical for the region, four different representatives of Hymenoptera order insects for identification: a bee, a wasp, a hornet, a bumblebee, and additionally, as a confounder, one representative of Diptera order – hoverflies, which resembles Hymenoptera, but their stings are harmless to humans. The image of each insect was shown as 2 pictures (top and side view) (see the Supplementary file). Questions referring to the pictures were scored as 1 point for the correct identification and 0 points for an incorrect identification, for a total possible score of 5. Each child and his/her parent responded to the questions separately. It took about 10 min to complete the questionnaire.
The study was approved by the Jagiellonian University Ethics Committee (dated 26 Jan 2017/No.122.6120.14.2017). The study was performed in accordance with the ethical standards as laid down in the 1975 Declaration of Helsinki, as revised in 2000. Because the research involved human participants, written informed consent was obtained before enrolment from the legal guardians (parents) of all participants. The data that support the findings of this study are available from the corresponding author upon reasonable request.
The Jagiellonian University Medical College supported the study through a subsidy for maintaining research potential. This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Statistical analysis
Distribution of qualitative variables was presented using frequencies and percentages, whereas for quantitative variables, means and SDs for normally distributed ones and medians and quartiles otherwise were used. χ2 test was used to examine the relationship between two qualitative variables. If at least 20% of cells in the analyzed table had expected frequencies lower than 5 the exact Fisher test for 2x2 tables and Fisher-Freeman-Halton test otherwise were used. Difference in mean age between studied groups was tested using Student’s t-test for independent samples. The difference in distribution of other quantitative variables between 2 groups was analysed using the Mann-Whitney test; when the size of the analysed subsample was lower than 30, the exact version of the test was used. Effects with p < 0.05 were treated as statistically significant. IBM SPSS Statistics 25 for Windows software was used.
Results
There was no difference in the mean age of children between Hymenoptera venom allergic group and controls (10.3 ±3.7 vs. 11.1 ±3.3 years; p > 0.05). Parents of children with HVA were younger than parents from the control dyads (38.9 ±7.1 vs. 41.5 ±8.3 years; p = 0.016). In both groups, most of children were males, and most of parents were females. The majority of participating children in both groups lived in the village. Most of children attended primary school. Most parents of children with HVA had obtained primary or secondary education, contrary to parents from the non-HVA group (Table 1).
Table 1
Demographics of the study groups
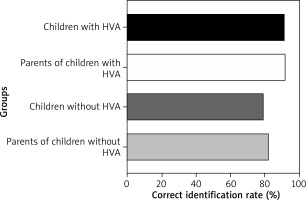
The differences between groups in the percentage of correct insect identification were statistically significant (p < 0.001) (Figure 1). The percentage of persons correctly identifying all kinds of insects was the highest in the group of parents of children with HVA (92.5%) and their children (91.2%). The lowest rate of participants who identified insects correctly was found in the group of children without HVA (78.8%) and their parents (82.4%).
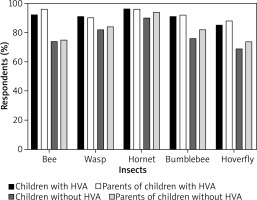
The differences between insects in the percentage of their correct identification by all study participants were also statistically significant (p < 0.001). The most frequently recognized insect in all groups was the hornet (up to 96.1% in children with HVA), whereas the least identified one was the hoverfly (down to 69.1% in children without HVA). In each group (children with HVA and their parents, children without HVA and their parents), the percentage of participants correctly identifying the insect varied depending on the kind of insect (p = 0.024, p < 0.001, p < 0.001, p = 0.018, respectively) (Figure 2).
Figure 2
Percentage of children with and without HVA and their parents correctly identifying insects based on pictures
The percentage of children stung by a bee, wasp and hornet was higher among the children with HVA than in the respective control group (Table 2). The percentage of parents stung by a bee was higher among parents of the children with HVA than in the respective control group. The children with HVA and their parents were mostly stung by a bee, the median number of stings per person was 3. The wasp was the second insect most often stinging children with HVA and their parents with the median number of stings per person amounting to 1 and 2, respectively. The median time from the last sting by a bee was shorter among children with HVA than in children without HVA. In parents of children without HVA, the time period from the last bee sting to the questionnaire survey was much longer than in parents of children with HVA (Table 2).
Table 2
History of stings in study groups
Children with HVA
Children with HVA, in comparison to children without HVA, were more likely to correctly identify the bee (92.2% vs. 74.5%, p = 0.001), bumblebee (91.2% vs. 76.5%, p = 0.005) and hoverfly (85.1% vs. 69.4%, p = 0.008). The correct identification of the wasp by children with HVA depended on their place of residence and was more common among children living in the village than in the city (95.0% vs. 76.9%, p = 0.018). Among children with HVA who correctly identified the wasp, the time from being stung by this insect to completing the survey was shorter in relation to the group of children with HVA who were unable to correctly identify the wasp (1.3 (Q1–Q3 0.4–2.6) vs. 5.2 (Q1–Q3 2.4–15.6) years, p = 0.03).
The rate of children with HVA who were stung by a bee, wasp and hornet was higher in comparison to the group of children without HVA (Table 2). The children with HVA stung by hornets were older than children who were not stung by this insect (12.4 ±3.9 vs. 10.0 ±3.5, p = 0.028). Children living in the countryside, regardless of their HVA status, were more often stung by a bee or a hornet than children living in the city (68.4% vs. 32.8%, p < 0.001 and 9.8% vs. 1.5%, p = 0.038, respectively).
Children without HVA
The correct identification of a bee and a bumblebee by children without HVA depended on their place of residence and was more common among children living in the city in comparison to children living in the countryside (86.7% vs. 64.2%, p = 0.011, and 88.9% vs. 66.0%, p = 0.008, respectively).
Most children without HVA who were attending junior high school (70.0%) were stung by a bee. Minority of children without HVA attending primary (29.6%) or high school (42.9%) were stung by this insect. Children without HVA stung by a bee or a wasp were older than children who were not stung by this insect (12.3 ±3.0 vs. 10.5 ±3.2 years, p = 0.005 and 12.3 ±2.9 vs. 10.4 ±3.3 years, p = 0.005, respectively).
Parents of children with HVA and parents of children without HVA
The parents of children with HVA, as compared to the parents of children without HVA, were more likely to correctly identify the bee (96.1% vs. 75.5%, p < 0.001), bumblebee (92% vs. 83.7%, p = 0.048) and hoverfly (88% vs. 74.5%, p = 0.015) (Figure 2). Only in the group of parents of children without HVA the correct identification of the bee, wasp and bumblebee depended on the parents’ level of education and was more common among parents educated at the high school level than parents who completed only the primary and junior high school (58.1% vs. 41.9%, p = 0.035, 57.8% vs. 42.2%, p = 0.007, 56.8% vs. 43.2%, p = 0.04, respectively).
The parents of children with HVA were more likely to be stung by a bee than the parents of children without HVA (78.4% vs. 58.2%, p = 0.002). Among the parents of children without HVA, those stung by a bee or by an unidentified insect were older than those who were not stung by these insects (43.2 ±8.0 vs. 39.2 ±8.2 years, p = 0.018, and 44.2 ±8.6 vs. 40.4 ±8.0 years, p = 0.040, respectively).
Discussion
The problem of Hymenoptera venom allergy is clinically important regardless of the patient’s age. According to the Centers for Disease Control and Prevention Wide-Ranging Online Data for Epidemiologic Research database of the US, documenting all animal-related fatalities between 2008 and 2015, deaths attributable to Hymenoptera (hornets, wasps, and bees) account for 29.7% of the overall animal-related fatalities and have been steady over the last 20 years [9]. The data from the online Network of Severe Allergic Reactions (NORA) suggest that insect venom is an important trigger of anaphylaxis both in children and adults (20.2% and 48.2%, respectively) [4]. Preponderance of stinging insects depends on the geographic region [10]. In Europe, 70.6% of anaphylactic reactions are caused by stings of wasps followed by those of bees (23.4%) and of hornets (4.1%) [4]. In the analysed populations, the children with HVA and their parents were mainly stung by bees. It is due to the fact that many patients were bee-keepers’ family members.
As the diagnosis of HVA negatively affects the quality of life [11–13], it probably makes patients more alert and pay more attention to flying insects. May be to the diagnostic process, HVA groups are better at recognizing the stinging insects. Moreover, the unpleasant experience associated with an allergic reaction to insect venom and the individual’s need to avoid another future reaction contribute to better identification of insects. This may explain a higher rate of correct insect identification among children with HVA and their parents than in the control groups. The identification abilities in a group of children with HVA did not differ significantly in comparison to the group of their parents. Children without HVA were less likely to correctly recognize stinging insects compared to their parents. Unlike in an earlier study [14], adults without HVA most often correctly recognized hornets, then wasps and bumblebees, followed by bees and hoverflies.
Identification of the culprit insect may be difficult, because insects may sting without being seen, they are relatively small, and share similar features with other members in the order, complicating identification of the perpetrator in many instances. Hymenoptera identification is difficult even for allergy-trained experts [15]. We have put among Hymenoptera species an example of Diptera (hoverfly, Syrphidae) as a confounder which resembles the bee or wasp (though it does not belong to Hymenoptera) in order to better assess the participants’ ability to recognize the insects in question.
The correct identification of a given insect may depend on the time since the last sting. However, this rule was not confirmed in reference to the majority of insects analysed in the study, but only in reference to wasps.
Interestingly, the relationship between the level of education and insect recognition skill was observed only in the group of parents of children without HVA referring to the bee, wasp and bumblebee identification. An older age and higher level of education among children were factors that should potentially improve the correctness rate in insect identification also in this population, but this has not been noted in our study.
According to our data, as well as to these already published, the significant percentage of the patients encounter difficulties in the correct identification of the insect that has stung them and caused the allergic reaction [14, 15], hence there is a need for an appropriate education. Most individuals have little or no formal education in insect identification [15]. As it is suggested in clinical practice, detailed colour photographs may be the best educational tool when educating individuals on salient characteristics of stinging insects and how to avoid them [15]. Compilation of a picture-based educational insect guidebook is simple and can be a useful resource for educating patients on stinging insect features and avoidance strategies, but these materials may not be helpful as a tool when considering testing to identify stinging insect hypersensitivity [15]. In the diagnostic approach an allergist should assess the patient by taking a clinical history, with the emphasis on the severity of symptoms, and by performing venom testing. Because the possibility of making a mistake in subjective data is high, objective medical records together with allergy tests must be performed to confirm the allergy. In some of the cases further diagnostic tests (component-resolved diagnostics, basophil activation test) are needed to correctly identify the allergy-relevant insect.
Allergen immunotherapy is instituted in these/individuals with insect sting reaction exceeding skin symptoms and confirmed IgE-mediated venom allergy [7]. Insect identification should be a part of both the diagnostic and educational process. The correct identification of the allergy-relevant insect is helpful for testing and accurate therapy of venom-allergic patients [6].
This study has some limitations to be considered. The first limitation concerns the time since being stung. The longer the time, the more probable an erroneous identification of the insect. It should be noted, however, that in the sample studied the time period between the last stinging event and taking the history from the subjects was longer for the children without HVA than from those with HVA. Another limitation is that picture representation of insects displayed colours slightly different than in reality. Despite this, the results of the previous study suggest that for identification purposes individuals are more likely to be successful using detailed photographs rather than actual dried insects [15].
Conclusions
Most of people experienced stings by Hymenoptera insects. Even despite potentially life-threatening allergic reactions, some children with HVA and their parents are not able to identify stinging insects correctly. The ability to identify stinging insects depends on the burden of HVA diagnosis, the distinguishing features of the insect (e.g. size), place of residence, the time that has passed since the sting, and the level of institutionalized education received. These skills, combined with knowledge of the habits and behaviours of individual insect types, can help prevent stinging, subsequently leading to HVA, and should be an integral part of diagnostic and educational process.