Dear Editor,
Blunt chest trauma can cause a number of life-threatening cardio-vascular complications, such as myocardial infarction, myocardial rupture, cardiac contusion [1], conduction disorders or arrhythmias [2]. An occasional yet life-threatening complication is the dissection of the coronary arteries. In such cases myocardial infarction is caused by mechanical damage to the coronary artery wall, which may lead to its dissection and/or clotting in its lumen [3].
A 24-year-old patient was admitted to the emergency department to treat the injuries sustained as a result of a traffic accident. The victim was the driver of a passenger car that collided with an excavator at high speed. On admission, the patient was conscious, sleepy, with respiratory insufficiency (Table 1). Intubation and mechanical ventilation were necessary. The trauma examination revealed numerous abrasions to the scalp, chest and abdomen, as well as contused wounds to both lower legs. Computed tomography (CT) polytrauma scanning was performed and demonstrated cerebral oedema, bilateral rib fractures and pulmonary contusion. During the diagnostic procedures, the heart rate significantly accelerated (157 min-1). An ECG was performed, and the concentration of myocardial necrosis markers was determined showing:
TABLE 1
Patient condition at Emergency Department
hsTnI (high-sensitivity troponin I) 2.444 ng mL–1,
CK-MB mass (creatinine-kinase MB mass) 7.2 ng mL–1.
The ECG visualised the ST segment elevation in the II, III, aVF leads and ST segment depression in the I, aVL and V2–V5 leads. Therefore, an emergency cardiological consultation was requested. According to the cardiologist, the most likely cause of the condition observed was myocardial contusion; there were no indications for invasive diagnostic procedures. One hour and 20 minutes after admission to the emergency department, the patient developed a sudden cardiac arrest due to ventricular fibrillation. Cardiopulmonary resuscitation was undertaken and after 10 minutes spontaneous, insufficient circulation was restored, which required a 0.1 μg kg-1 min-1 infusion of norepinephrine, later increased to 0.2 μg kg-1 min-1. It was decided to transfer the patient to the intensive care unit (ICU) for further treatment.
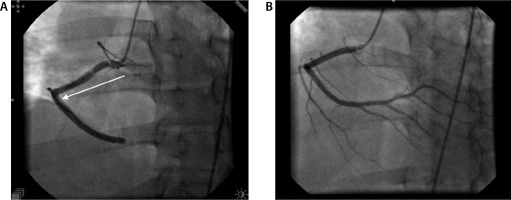
The patient was admitted to the ICU in an extremely severe general condition. His circulatory and respiratory functions remained impaired; therefore, he required further mechanical ventilation and the infusion of pressor amines. Due to a 20-fold increase in TnI, the patient was reconsulted by the cardiologist. The ECG performed disclosed numerous abnormalities: sinus tachycardia 116 min-1, ST segment elevation, pathological Q waves in the III and aVF leads, and tall R waves in the V1–V2 leads. The echocardiogram demonstrated hypokinesis of the right ventricular inferior wall and the free wall as well as widening of the right ventricle. Based on the findings of the examinations performed, inferior wall and right ventricular myocardial infarction was diagnosed. Coronary angiography was emergently performed, which revealed the dissection of the right coronary artery (RCA). RCA angioplasty with stent implantation were undertaken (Figure 1). Over the following days, the general condition of the patient gradually stabilized. The follow-up echocardiographs showed a gradual improvement in the myocardial systolic function. On post-admission day 4, an angio-CT was performed due to a decrease in saturation to 90% and significantly deteriorated gas exchange; the embolic material was visualised in both branches of the pulmonary artery. Anticoagulant therapy was initiated, which led to thrombus resolution. Once verbal contact with the patient was regained, on day 7, extubation and passive oxygen therapy were decided. The patient`s condition significantly improved; on hospitalisation day 13, once fully verbally and logically responsive (GCS 15 points) and with efficient circulatory and respiratory functions, he was transferred to the department of cardiology. On day 26, the patient was discharged home; rehabilitation and cardiological follow-ups after six and twelve months were recommended.
FIGURE 1
Image recorded during percutaneous coronary intervention. A) A catheter and right coronary artery dissection (an arrow). B) The same vessel after angioplasty and stenting
Six months after the incident, the patient in a good general condition presented to the department of cardio-logy for a follow-up coronary angiogra-phy, which demonstrated suboptimal stent implantation. RCA balloon angioplasty was decided. The procedure was uneventful and led to good outcomes. During the treatment, TnI (hsTnI prior to angioplasty: 50.156 ng mL-1, hsTnI after angioplasty: 49.163 ng mL-1) were determined. The follow-up after one year was correct, no alarming changes were found (hsTnI: 0.0055 ng mL-1). The patient consented for publishing his case details.
Coronary artery dissection is a rare yet life-threatening complication of blunt chest trauma. Traffic accidents (63.6%) are the most common causes of blunt chest injuries; 69% of them are car accidents [4]. In addition to traffic accidents, the injuries in question may occur during sports [4, 5] and due to impacts [5]. The most likely mechanism of coronary artery trauma involves sudden mediastinal overloads leading to high shear forces acting on the vascular wall, severe compression on the heart between the sternum and the spine, and a sudden increase in aortic pressure caused by rapid compression of the abdomen and lower extremity vessels [6]. Noteworthy, the incidence of injuries to the left coronary artery (76%) is much higher, as compared to those to the right coronary artery (12%) and the circumflex branch (6%) [7]. The cause of this distribution and location of injuries has not been fully elucidated. The anatomical conditions and the position of the heart in the mediastinum have been implicated. For the same reasons, the right coronary artery is much more likely to be dissected at its initial segment originating from the aortic bulb [7]. It is worth highlighting that the formation of such injuries is more common in the atherosclerosis-affected arteries, even in diseases whose stages are clinically occult [5].
The typical symptoms of injuries resulting from coronary artery dissection are increased concentrations of myocardial necrosis markers, heart failure and abnormal ECG readings indicative of ischaemia in the vascular area affected by artery dissection [6–8]. These symptoms may be accompanied by arrhythmias associated with heart contusion, e.g. sinus tachycardia [1].
In blunt chest injuries, which are very characteristic of collisions involving motor vehicles, the physician should always take into account the possibility of injuries to the thoracic organs. In the case of cardiac disorders, once pericardial tamponade, pleural haematoma, and pneumothorax have been excluded, possible dissection of one of the coronary arteries should be considered, especially when the features of myocardial ischaemia are found on ECG. In patients in good general conditions, electrocardiogram- gated computed tomography may be considered to locate likely abnormalities in the coronary vessels. Some authors have suggested that even when the conventional CT polytrauma protocol is followed, coronary vessel dissection can be visualised. The easiest way to show such injuries is to perform a CT examination in a patient with bradycardia, when the artifacts associated with cardiac action are minimal [6]. When coronary artery dissection is diagnosed, an emergent intervention should be considered. The time between sustaining the injury and the implementation of the therapeutic method determines the prognosis and the extent of further complications [9]. Dissection of the coronary artery, which may initially manifest as arrhythmias [1], is usually not the first diagnosis to be considered in a polytraumatic patient. Nevertheless, special vigilance should be exercised when diagnosing arrhythmias in trauma victims, which should be effectively differentiated them from other cardiac complications associated with blunt chest injuries.




