Dear Editor,
Anaesthesia for emergency life-saving surgery can pose challenges such as limited time for evaluation and preparation of the patient, haemodynamic instability, and fluid/electrolyte imbalance, and it is associated with high morbidity and mortality [1]. Usually, these patients are at high risk of aspiration due to inadequate fasting intervals. Despite adequate precautions, aspiration cannot be prevented in some cases. Aspiration is the inhalation of either oropharyngeal or gastric contents into the larynx and lungs [2]. The consequences are determined by the quantity and nature of the material aspirated, as well as the host’s response. The 3 syndromes associated with aspiration are chemical pneumonitis, bacterial pneumonia, and airway obstruction. The patient may have one or more of these, depending on the type of aspirate [2]. Aspiration of gastric acidic content can lead to chemical pneumonitis (Mendelson syndrome), while aspiration of bacteria from oral and pharyngeal areas can add to infection, and macro aspiration of gastric contents can lead to airway obstruction [3]. Aspiration pneumonia is associated with higher mortality than other forms of community-acquired pneumonias (29.4% vs. 11.6%) [4]. Bronchoalveolar lavage (BAL) is a minimally invasive procedure that involves instillation of sterile normal saline into a subsegment of the lung, followed by suction and collection of the instil-lation for analysis. In the context of aspiration, BAL has been described as a diagnostic technique with elevated a-amylase concentrations in BAL fluid as a marker of aspiration [5–7]. The role of therapeutic BAL is well known for pulmonary alveolar proteinosis [8]. We report the use of therapeutic BAL in mitigating the effects of aspiration in a patient undergoing emergency re-exploration for intra-abdominal bleeding.
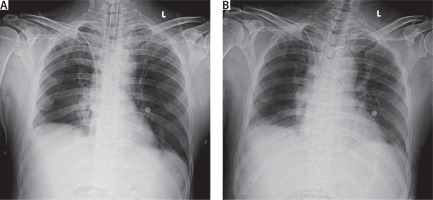
A 48-year-old man underwent laparoscopy-assisted distal radical gastrectomy with D2 lymphadenectomy and Roux-en-Y retro-colic gastro-jejunostomy for carcinoma of the stomach following 3 cycles of neoadjuvant therapy. Early post-operative course was uneventful, and he was allowed oral liquids from day 2. On postope-rative day 5, he had intra-abdominal bleeding following drain removal. Due to profuse bleeding from the drain site, within minutes he became haemodynamically unstable, and emergency re-exploration surgery was planned. Because he had eaten a meal an hour ago, anaesthesia was induced in the Trendelenburg position and intubated with a rapid sequence protocol. Despite the precautions taken, he regurgitated and aspirated the gastric contents. After a quick intratracheal and oral suction, the patient was handed over for surgery, considering the need for emergent intra-abdominal haemostasis. The cause of bleeding was identified as splenic artery secondary to focal pancreatitis, and ligation of the splenic artery with splenectomy was done. The surgery lasted for 90 minutes. Once the bleeding was controlled, a therapeutic BAL through an endotracheal tube was performed to remove the aspirated gastric contents from the principal bronchi and their accessible subsegments. The entire process took one hour, and about 3 L of normal saline at 37°C was instilled in 50-mL aliquots, and close to 2.6 L of instilled volume was suctioned out with the gastric contents. Figure 1 demonstrates the food particles including rice grain particles that were removed during therapeutic BAL. Patient was intermittently ventilated during the procedure with low tidal volume to avoid distal migration of the aspirated material. The patient was given meropenem 2 g along with metronidazole 500 mg intravenously 3 times a day for 5 days empirically as prophylaxis for pulmonary infection. After BAL, the patient was electively ventilated in the intensive care unit to assess the lung injury and maintain positive end-expiratory pressure. On arrival, the patient’s body temperature was 36.1°C, and he was actively warmed to normothermia. He maintained near normal oxygen saturations and airway pressures, and his trachea was extubated on postoperative day 2. Inotropes were weaned off over 2 days. Clinico-radiological evaluation revealed well expanded lungs on day 3 (Figure 2). He was discharged home on postoperative day 6 in a stable condition.
This case illustrates how therapeutic bronchoalveolar lavage can effectively mitigate the consequences of aspiration like chemical pneumonitis and bacterial pneumonia. Therapeutic BAL performed in alveolar proteinosis helps clear the alveoli of the proteinaceous material. The lite-rature mentions variable amounts of fluid used for therapeutic BAL, i.e. 5–40 L until the returning fluid is clear [9]. We found 3 L to be adequate. Ideally, therapeutic BAL should start as early as possible to be effective. Although intuitively one may believe that earlier is better, the time gap between aspiration and BAL which can still protect the lung of the adverse effects of aspiration is unknown. In this case we started therapeutic BAL as soon the rectus sheath closure was started, because haemostasis for intra-abdominal bleeding was the priority. Recent literature suggests an increasing incidence of multidrug resistant pathogens in sick hospitalized patients with aspiration pneumonia. Empiric antibiotics including carbapenems may be started based on the associated risk factors [10].
We report successful prevention of aspiration syndrome with therapeutic BAL and recommend it for macro-aspiration of gastric contents. More studies are required to establish its utility and ideal timing.