Patients with critical neurological conditions must be transported to a trauma centre that can provide specialised care [1]. In Lithuania, the largest centre is the Neurosurgery Clinic of the University of Health Sciences Hospital in Kaunas. According to the order of the Minister of Health of Lithuania, urgent patients can be transported to this centre from 4 different regions, which make up 13 diffe-rent hospitals in Lithuania [2]. It means that approximately 1.1 million people make up the range from which neurocritical patients could be transferred to the Hospital of Lithuanian University of Health Sciences Kaunas clinics. This amount of people makes up 38.6% of the total Lithuanian population [3]. The quality of care and treatment provided during transportation is of paramount importance and is related to the outcome of critically ill patients [4]. Studies have shown that patients undergoing transfer with specialised transport are associated with a lower 24-hour mortality rate [5].
The high-quality cooperation between the staff of the referring and receiving institutions ensures that a proper assessment and stabilisation are planned before the transfer and that the initial treatment is maintained throughout the whole transportation time to a specialised centre [6]. To make the transfer of critical patients from one hospital to another as safe as possible, the guidelines for the safe transportation of critical neurological patients were updated in 2019. These guidelines pay equal attention to the assessment of patients’ vital signs as well as their neurological status. The following must be monitored during the transport: patient consciousness according to the Glasgow Coma Scale (GCS), pupil size and response to light, standard electrocardiogram (ECG), systolic arterial blood pressure (sABP), oxygen saturation (SpO2), and diuresis and end-tidal carbon dioxide (ETCO2) if a patient is intubated or being ventilated [7]. All information about the patient must be recorded on a special transport sheet, which is handed over to the specialist care staff at the trauma centre after the patient has been transported [8]. Although these guidelines for the safe transport of patients with critical neurological conditions were published in 1996 and upgraded 2 times after that (2006 and 2019), their practical application in Lithuania remains questionable.
In our study, we aimed to assess the quality of interhospital transportation of neurocritical patients in the largest neurosurgical cluster in Lithuania and identify possible outcome prediction variables.
METHODS
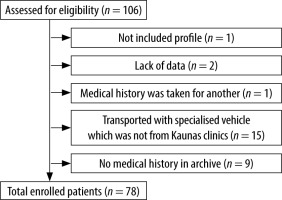
A retrospective cohort study was conducted. After approval of the local Ethics Committee (2022-06-20, BEC-MF-491), we analysed the data from 106 neurocritical patients who were transported to the Hospital of Lithuanian University of Health Sciences Kaunas Clinics Neurosurgery Clinic in 2018. We decided to evaluate the year 2018 to obtain results that were not influenced by the COVID-19 pandemic. The inclusion criteria were the following: neurocritical patients who were transported by a specialised ambulance to the Hospital of Lithuanian University of Health Sciences Kaunas Clinics Neurosurgery unit, and those who were 18 years old and above. The data were collected from the hospital’s electronic medical history system. All inpatients consented to the use of data related to their disease for scientific purposes.
Patients’ outcomes were described as negative or positive. Negative outcomes were considered as death, persistent vegetative state, or severe disability. Positive outcomes were moderate or low disability or full recovery. Normal distribution dates were expressed as mean (standard deviation). The normality of variables was assessed with the Kolmogorov-Smirnov test. Non-normal distribution data were expressed as median (min, max). For non-parametric data, the Mann-Whitney U test was performed for comparison between groups. Qualitative data are provided as numbers and percentages. The statistical analysis was performed using IBM Statistical Package for the Social Sciences (SPSS) statistical software (version 27, Chicago, IL., USA). P-value less than 0.05 was considered significant.
RESULTS
Seventy-eight patients were enrolled in the study (Figure 1). Out of all 78 transported patients, 41 (52.6%) were diagnosed with a traumatic brain injury, 14 (7.9%) – intracerebral haemorrhage (ICH), 7 (9%) – subarachnoid haemorrhage, 2 (2.6%) – ischae-mic brain stroke, and other diseases – 14 (17.9%). Patient demographics and transferring data are shown in Table 1.
TABLE 1
Patient age and departure from the initial hospital time indicators
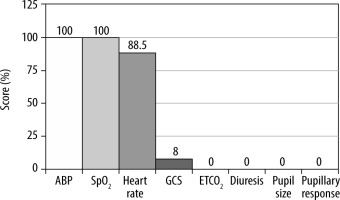
According to the Guidelines from the Association of Anaesthetists and the Neuro Anaesthesia and Critical Care Society, during the transfer it is important to monitor and document the following aspects: Glasgow Coma Scale, pupil size and response to light, standard ECG, arterial blood pressure, SpO2, and diuresis and ETCO2 if a patient is intubated or being ventilated. Unfortunately, in 21.8% of all transported neurocritical patients’ cases, the transport sheet was not completed at all. After analysing the filling protocols of 61 patients during transportation to the Hospital of Lithuanian University of Health Sciences Kaunas Clinics Neurosurgery unit, it was found that although diuresis and ETCO2 were not monitored in any patient, the vital parameters were monitored better than the neurological status of the patients. Consciousness was assessed by GCS in only 8% of patients. Pupil size and reaction to light were not assessed in any patient (Figure 2).
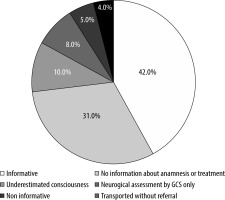
During the study, the quality of referrals to the Kaunas Clinics Neurosurgery unit was evaluated. It was found that less than half (42%) were informative and suitable for sending the patient to another hospital. It means that all necessary information was collected about anamnesis of the disease and life, objective condition (full neurological examination, hemodynamic and other parameters), applied treatment, and stabilisation of the condition before transportation. Another 58% of referrals had deficiencies (Figure 3).
All information about the initial condition of the patient, stabilisation, and applied treatment methods are important and affect the outcomes of the patients. In our study, we found that the first sABP measured at Neuro-ICU is associated with patient outcomes. Significantly higher sABP values (P = 0.041) were recorded in the group of patients with negative outcomes (death, continued need for care) (Table 2).
TABLE 2
Comparison of first systolic arterial blood pressure measurement in Neuro- ICU and patients’ outcomes
| Variable index | Positive outcome (n = 25) | Negative outcome (n = 53) | P-value* |
|---|---|---|---|
| sABP (mmHg) Median (min-max) | 133 (82–197) | 155 (42–205) | 0.041 |
We also analysed the outcomes of all transferred neurocritical patients depending on their diagnosis. Of all subjects (78), 32.1% recovered and 67.9% had negative outcomes. In each disease group, it is observed that most patients did not recover. The worst outcome can be seen in patients with ICH, only 14% of whom have recovered (Table 3).
TABLE 3
Outcomes of transported neurocritical patients
| Outcome | ICH | Traumatic brain injury | SAH | Ischaemic stroke | Other diseases | All together |
|---|---|---|---|---|---|---|
| Positive | 2 (14%) | 16 (39%) | 0 (0.0%) | 1 (50%) | 6 (43%) | 25 (32.1%) |
| Negative | 12 (86%) | 25 (61%) | 7 (100%) | 1 (50%) | 8 (57%) | 53 (67.9%) |
Moreover, we analysed the outcomes of neurocritical patients who were hospitalised directly in the Neuro-ICU. Of all patients (704), 44% had positive outcomes while 56% had negative outcomes. The worst outcome can be seen in patients with ICH, 83% of whom had negative outcomes. Patients who had other neurological diseases were seen to have the best outcomes (93%, Table 4).
Discussion
In our study, we found that patients who had significant hypertension episodes after transport had worse outcomes compared to those who did not. According to the AHA/ASA (American Heart Association/American Stroke Association) guidelines, in patients with ICH, the target sABP is 140 mmHg. This guideline proves to be helpful because higher sABP is mostly associated with a higher probability of haematoma growth, while lowering sABP to < 120 mmHg shows a greater risk of remote cerebral ischaemic lesions and acute neurologic deterioration [9]. Moreover, aggressive hypotension is associated with cerebral hypoperfusion and contributes to secondary brain damage. Lavrentios B et al. found that hypotension increases 30-day mortality, especially if it lasts > 60 min [10]. Conversely, a retrospective study has shown that higher blood pressure creates a greater risk of mortality if hypertension is the only ICH aetio-logical factor [11]. In contrast to these studies, Shi et al. [12] conducted a meta-analysis that demonstrated the lack of curative qualities of intensive blood pressure lowering in ICH patients with high blood pressure. The only beneficial outcome is attenuation of haematoma growth (≤ 62 years old) when the ICH volume is less than 15 mL and intensive blood pressure management is undertaken in less than 6 hours. Zafar et al. [13] found that in neurocritical trauma patients the mortality rate can be 21% when the sABP is 120 mmHg, 9% when it ranged between 120 and 140 mmHg, and 19% when the sABP was 140 mmHg. Thus, the initial sABP treatment is significant for better patient outcomes and should be administered promptly.
We did not find any statistically significant results when considering specific neurocritical conditions and their outcomes. We think this is due to the small sample of patients in the individual groups. Although we did not find a statistically significant difference between the subgroups, our analysed data showed that non-specialised hospitals need more experience in the initial treatment and stabilisation of neurocritical patients. To achieve better results in the future, the focus should be on communication between the transferring and accepting hospitals and consultations with professionals who work in specialised centres.
The transferal of neurocritical patients is as significant as the initial and specialised care. Our study shows that negative outcomes were most likely to occur if patients had a significant variation of sABP (comparing the sABP median min – max values: 42–205 mmHg in the negative outcomes group vs. 82–197 mmHg in the positive outcomes group). As mentioned before, neither hypotension nor hypertension is advantageous for neurocritical patients.
Hypotension can result in ischaemia due to hypo-perfusion, while hypertension can lead to larger haematomas and higher mortality rates. Jeon et al. [14] showed that high sABP variation is associated with haematoma growth and poor 3-month outcome in patients with supratentorial non-lobar ICH. These results suggest that sABP must be monitored continuously, and any higher or lower ranges in sABP must be treated immediately.
During the transportation of neurocritical patients, it is essential to ensure a constant sABP measurement. Although in our study all 100% of transportation protocols had sABP measured, it is believed that the monitoring is not frequent enough or sABP changes are not being treated. Poor results could be reached due to infrequent monitoring, so it would be useful to monitor sABP more often to notice changes as soon as possible and to correct them immediately. For better outcomes, the transportation of neurocritical ill patients must be re-evaluated. Today, the largest pre-hospital clinical stroke trial “INTERACT4” is being conducted in China to find the best stroke treatment strategy in the ambulance setting [15].
More studies regarding the transportation of neurocritical patients have not been accomplished yet, so there is a lack of practical advice and recommendations on what should be improved to achieve better results.
During our research, we found that in 2018, 67.9% of transported neurocritical patients had poor outcomes. By contrast, 56% of patients who were admitted directly had negative outcomes. Furthermore, most of the groups had better results. All SAH patients who were transferred with a specialised vehicle had negative outcomes, while 46% of directly admitted patients had positive results. This contrast could have been influenced by improper stabilisation of critical conditions or poor transportation to a specialised centre. After a thorough analysis of our research, we can suggest some changes to improve patient outcomes. First, the quality of referrals must be refined to document the condition of neurocritical patients precisely and to give appropriate information to colleagues. Secondly, the transportation itself must be improved, it is important to fill in the transport protocol as well as continuously monitor patients’ vital signs not excluding neurological parameters (GCS, pupil size, and response to light), diuresis, and ETCO2. Additionally, any significant changes in a patient’s status during the transferal must be treated immediately; therefore, a specialised team is required. Lastly, the accepting hospital can contribute to its success by putting out a team of professionals who can give lectures. Communication should be the focus to achieve greater results in patient care.
Starting our study, we opted to enrol all consecutive neurocritical patients in our department. Twenty-eight patients were excluded from the data analysis. The reasons for exclusion were lack of medical histories (10), after transportation it was seen that the patient’s underlying disease was not neurocritical (1), patients were transported with another hospital’s vehicle, so we did not have the opportunity to analyse the transportation sheets (15), and a lack of data of the start and end times of transportation (2). We felt that these patients were not eligible for the final analysis.
Despite all the aspects that our study lacked, our research has some value in understanding the faults and strengths of our transportation practice. On a global scale, there are some other studies with a similar aim, mainly focusing on communication between staff and perfecting checklists before the transfer. Some studies have shown that after implementing a checklist, during the period of ICU transfer, checklists were used in more than 85% of patients; therefore, the average length of hospitalisation decreased. A checklist was associated with improved safety perceptions and reduced patient transfer times. Also, after the failure mode and effect analysis intervention, interdisciplinary communication, and patient safety improved significantly [16, 17].
This was the first study of this nature in Lithuania and the only one to highlight the scarcity of proper documentation. Thus, to have a better practical value, a larger study should be conducted in the future.
CONCLUSIONS
In our retrospective cohort study in Lithuania, we found that the guidelines for the safe transfer of neurocritical patients should be improved. The weakest links in patients’ transferrals were found to be the monitoring of vital signs and neurological parameters during the transfer as well as the quality of referrals to a specialised hospital. Of all subjects, only 32.1% recovered and 67.9% had negative outcomes. This shows that for better outcomes, the transportation of neurocritical ill patients must be re-evaluated.