Introduction
The vascular anatomy of the colon is quite complicated, and, in particular, splenic flexure is considered as one of the most variable areas by vascularisation. When large mesenteric vessels are surgically ligated, the mesenteric circulation has a rich collateral network to maintain adequate perfusion in the colon [1–3]. These collaterals between the superior mesenteric artery (SMA) and inferior mesenteric artery (IMA) play an important role in colonic surgery; the most well-known are the Drummond marginal artery and Riolan’s arch [4–7].
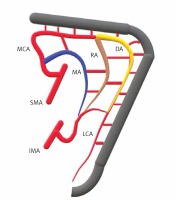
The meandering mesenteric artery, also known as the Moskowitz artery, is a lesser-known collateral pathway and represents another link between the SMA and IMA (Figure 1). The Moskowitz artery (MA) runs along the colonic mesentery floor and represents the link between the proximal segment of the middle colic artery and the ascending branch of the left colic artery. The Moskowitz artery runs through the base of the mesocolon, above the ventral edge of the pancreas [8, 9].
Figure 1
Upper image represents the collateral structures at the splenic flexure level; the yellow marked structure at the lateral side is the Drummond marginal artery (DA), the brown marked structure in the middle is Riolan’s arch (RA), and the blue marked structure at the medial side is the Moskowitz artery (MA)
MCA – middle colic artery, RA – Riolan’s arch, DA – Drummond artery, MA – Moskowitz artery, SMA – superior mesenteric artery, IMA – inferior mesenteric artery, LCA – left colic artery.
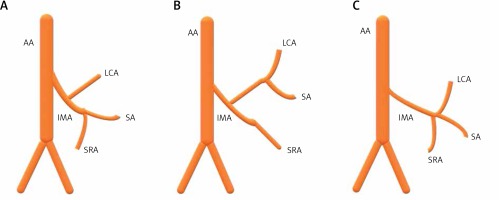
Arterial blood supply of the left colon occurs through the left colic artery and sigmoid artery branches originating from the IMA. There are three main types of branching of the left colic artery from the IMA (Figure 2). In type 1, the left colic artery originates from the IMA as a single branch. In type 2, the left colic artery (LCA) and sigmoid artery arise as a common branch. In type 3, the left colic artery, sigmoid artery, and superior rectal artery branch simultaneously from the IMA [10–12].
Figure 2
Three main types branching of the left colic artery from IMA are observed: A – the left colic artery originates from IMA as an independent single branch (type 1), B – left colic artery and sigmoid artery emerge as a common branch (type 2), C – left colic artery, sigmoid artery (SA) and superior rectal artery (SRA) simultaneously originate from the IMA
AA – abdominal aorta, LCA – left colic artery, IMA – inferior mesenteric artery, SA – sigmoid artery, SRA – superior rectal artery.
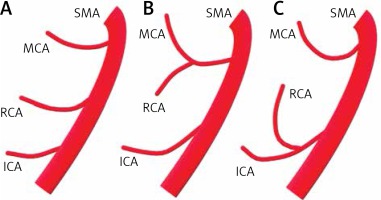
The middle colic artery (MCA) plays a critical role in the blood supply of splenic flexure and originates from the superior mesenteric artery. The middle colic artery originates mainly from the SMA in two different ways [13–16]. It usually originates from the superior mesenteric artery as a single branch and less often arises as a combination branch with the right colic artery (Figure 3).
Figure 3
The image depicts the origin of the middle colic artery (MCA) from the superior mesenteric artery in three main ways. It is noteworthy that the MCA takes origin as a single branch in (A) and (C) and as a combined branch in (B)
SMA – superior mesenteric artery, MCA – middle colic artery, RCA – right coronary artery, ICA – inferior colic artery.
Aim
In this study, we aimed to comprehend the presence and importance of the Moskowitz artery (meandering mesenteric artery) in preoperative patients. In multislice computed tomography studies, we tried to define the collateral vascular circulation and surgical importance of the splenic flexure vascularisation at this level by highlighting the Moskowitz artery. Also, we tried to evaluate the relationship between the left colic artery ascending branch diameter, branching types of the left colic artery from the IMA, variant types of emerging from the middle colic artery, and the presence and diameter of Riolan’s arch and the Moskowitz artery.
Material and methods
The permission and methods used for this study were approved by the local ethics committee of Yeditepe University Faculty of Medicine. Between April 2015 and September 2018, all abdominal computed tomography (CT) images performed using intravenous contrast for any reason at the Radiology Department of Yeditepe University Hospital were scanned retrospectively. Patients older than 18 years with intravenous contrast (arterial and venous phases with a cross-section thickness of 0.625 mm), who underwent abdominal CT scan, and patients without any abdominal surgery were included in the study. Surgical history of the gastrointestinal tract, tumour in the right, middle, or left colon, cirrhosis and portal hypertension, abdominal aorta and iliac artery occlusion or stenosis, diabetes mellitus, body mass index (BMI) ≥ 35 kg/m2, or age younger than 18 years were excluded from the study. As a result of the screening, 109 CT scans with eligibility criteria were included in the study. In the CT examination of each case included, measurements and comments were made by a radiologist experienced in abdominal radiology.
CT images of the cases were obtained by using a multislice CT with 64 detectors (Revolution HD/GSI, GE Healthcare, Chalfont St Giles, UK). CT parameters of the abdominal angiography scan included the following: 0.625 mm section thickness, 120 kVp, 200 mA, 0.4 s of a gantry rotation time, and 512 × 512 matrix size. All patients were received intravenously through an 18-gauge angiographic catheter placed in the forearm vein using a mechanical injector at a flow rate of 3 ml/s. Arterial phase images were obtained after a 20-second scan delay from IV contrast agent injection and portal venous phase images after a 70-second scan delay.
Multislice CT images were transferred to a customised workstation program for GE Volume Viewer v13.0 ( GE Healthcare, LLC, Waukesha, WI), and vascular structures were evaluated. Analysis and measurements were performed on axial, coronal, oblique, and sagittal format images for all cases. Additional data were obtained for each case by additionally providing three-dimensional post-processing such as multi-plane image reformatting (MPR) and maximum density projections (MIP).
In the CT images, for each case, the following were evaluated: the presence and diameter of the Moskowitz artery, the diameter of the Drummond marginal artery, the presence of Riolan’s arch and the first diameter at the level of origin, the first emerging diameter of the middle colic artery, the LCA ascending branch diameter, the MCA origin types, and their relationship with the Moskowitz artery, respectively.
Statistical analysis
Statistical analyses were done using SPSS software (IBM SPSS v22.0, IBM, Armonk, NY, USA). Descriptive statistical methods (median, frequency, percent, minimum, and maximum) were used to express the central tendency. The normality of quantitative data distribution was evaluated by the Kolmogorov-Smirnov test. Pearson’s correlation analysis was used to evaluate the relationship between the parameters. Logistic regression analyses were applied for univariate and multivariate analyses. Student’s t-test test was applied to evaluate differences in continuous variable and categorical variables, respectively. P-value < 0.05 was considered statistically significant.
Results
There were 109 cases in this study; 50 (45.9%) of them were male and 59 (54.1%) were female. The youngest case was 18 years old, the oldest case was 92 years old, and the median age was 55 years. The Moskowitz artery was found in 18 (16.5%) cases; 8 were males and 10 were females (Photo 1). Riolan’s arch was present in 30 cases, of whom 15 were male and 15 were female. Drummond marginal artery was present in all participants (100%). MCA and LCA ascending branches were presented in all cases; mean diameters of the vascular structures and demographic data are summarised in Table I.
Photo 1
In abdominal CT examination obtained in arterial phase the Moskowitz artery is indicated by yellow arrows in coronal (A) and axial (B) images
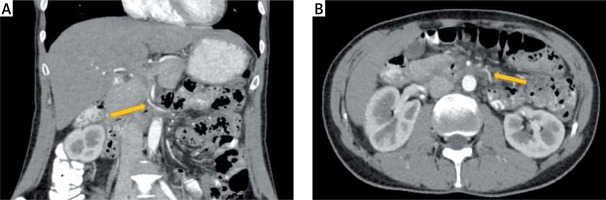
Table I
Demographics and measurement of vascular diameters
The youngest case in males was 18 years old and the oldest case was 92 years old, the average age was 55.66; while the youngest case in females was 26 years old and the oldest case was 84 years old, and the average age was 54.06 (Table II).
Table II
Distribution of demographics and vascular diameters by gender
When MCA types were evaluated, 75 cases had a single branch and 34 cases had combined branch type. Regarding LCA types, there was an independent branch in 58 cases, common branch in 22 cases, and simultaneous branching type in 29 cases. There was no statistically significant difference between gender and MCA and LCA types (p > 0.05) (Table III).
Table III
MCA and LCA types
| Type | N | Percent | |
|---|---|---|---|
| MCA: | Single branch | 75 | 68.8 |
| Combined branch | 34 | 31.2 | |
| Total | 109 | 100.0 | |
| LCA: | Type 1 | 58 | 53.2 |
| Type 2 | 22 | 20.2 | |
| Type 3 | 29 | 26.6 | |
| Total | 109 | 100.0 | |
There was no statistically significant difference between age, gender, and presence of MA. There was a statistically significant difference (p < 0.05) between the combined MCA emerging type and the presence of MA, and 12 cases with a combined branch and 6 cases with single branch had Moskowitz artery.
There was a statistically significant difference (p < 0.05) between LCA types and the presence of MA, and the Moskowitz artery was most commonly present in cases with type 1 LCA. The same number of MAs was in type 2 and type 3 LCA (Table IV).
Table IV
Presence of MA and its relationship with LCA types
| Variable | LCA types | Total | ||||
|---|---|---|---|---|---|---|
| Type 1 | Type 2 | Type 3 | ||||
| MA | (–) | N | 46 | 19 | 26 | 91 |
| % | 50.5 | 20.9 | 28.6 | 100.0 | ||
| (+) | N | 12 | 3 | 3 | 18 | |
| % | 66.7 | 16.7 | 16.7 | 100.0 | ||
| Total | N | 58 | 22 | 29 | 109 | |
| % | 53.2 | 20.2 | 26.6 | 100.0 | ||
According to Pearson’s correlation, there was a very strong (+) correlation between the RA diameter and the MA diameter (r = 0.894, p < 0.05). When evaluated respectively, there was a (+) medium correlation between MCA diameter, LCA ascending branch diameter, and RA diameter (r = 0.384–0.397, p < 0.05). A medium (+) correlation was found between DA diameter and MCA diameter (r = 0.331, p < 0.05). There was also a strong (+) correlation between MCA diameter and MA diameter (r = 0.646, p < 0.05). Finally, there was a strong (+) correlation between MCA diameter and LCA ascending branch diameter (r = 0.504, p < 0.05).
Discussion
The clinical significance of left colon and splenic flexure vascularisation has been evaluated in multiple studies, and collateral pathways have been identified. The most well-known among these is the Drummond marginal artery and Riolan’s arch [4–6, 17, 18]. Another little-known collateral pathway is the Moskowitz artery [7–9]. However, there are also some different views on the identification and naming of the Moskowitz artery. For example, some argue that this artery is an expanding part of Riolan’s arch, while another view is that it is a separate anastomotic structure [5–9]. In our study, we observed the Moskowitz artery as a separate anastomotic structure, similar to the second opinion.
The main approach during the mesocolic excision of tumours located around the splenic flexure with the medial laparoscopic method is the opening sac to the ventral edge of the pancreas. This step is important for obtaining non-tensioned colorectal anastomosis, splenic flexure mobilisation, and mesocolic excision of the tumour [19, 20]. However, when the presence of the Moskowitz artery is overlooked in some cases in this region, a risk of bleeding may be encountered during surgical dissection [21, 22].
On the medial approach, during mobilisation of the laparoscopic splenic flexure, in the presence of the Drummond artery, the avascular region is considered as a large and safe area. In the presence of the Moskowitz artery and Riolan’s arch, there will be collateral pathways in this region because of the risk of iatrogenic bleeding, and hence controlled laparoscopic dissection is required. The presence of this artery becomes important due to ischaemic, anastomosis safety or pathological conditions that provide alternative blood flow to hypoperfusion sites after surgical ligation during abdominal surgery [23–26].
The presence of the Moskowitz artery is important mainly in left colon surgery and low anterior resection, and it may cause difficulties in mobilization of the splenic flexure during surgery [27–29]. The Moscowitz artery must be cut to fully mobilise the splenic flexure and achieve a low tension-free anastomosis in the pelvis [19, 20]. This can create extensive proximal ischaemia and a greater need for mobilisation. Especially in the need for more splenic flexure mobilisation, undesirable consequences such as splenic injury may be encountered [23, 24]. Conversely, in cases where the Moskowitz artery is not cut, it may cause tension in the anastomosis [21]. Therefore, preoperative radiologic evaluation of the presence of the Moskowitz artery during left colon surgery during splenic flexure mobilisation and prevention of anastomotic complications is important.
Dilatation of the Moskowitz artery may develop as a result of chronic obstruction of SMA and IMA. A similar situation can be seen during distal abdominal aorta occlusion and chronic obstruction that may develop in the iliac arteries [23–27]. In order to maintain vascularisation in the colorectal anastomosis, it is very important not to damage the MA intraoperatively, and tissue ischaemia in this area is considered a risk factor for anastomotic leakage [28].
Garcia-Granero et al. reported in a cadaver study of splenic flexure mobilisation that Drummond marginal artery was observed in all cases. Also, Riolan’s arch was found in 18% of cases and Moskowitz’s artery in 11%. However, the relatively low number of patients and the lack of vessel diameters are noteworthy [9]. In addition, the need for a radiological preoperative study is mentioned in this field for correct and safe surgery. Most of the studies on splenic flexure vascularisation in the literature have focused on the terms “Riolan’s arch” and “meandering mesenteric artery”, but the existence and definition of the Moskowitz artery have been relatively insufficient [4–7, 18–20].
Our study has one of the largest case numbers in the literature to determine the presence of the Moskowitz artery. Also, as a result of evaluating the relationship between the Moskowitz artery and Riolan’s arch, Drummond marginal artery, MCA, and LCA types, very valuable data were obtained (Tables II–IV). In our study, the Moskowitz artery and Riolan’s arch were monitored as separate vascular structures, and in all cases with the Moskowitz artery, Riolan’s arch was also present. Limitations of our study include the evaluation of cases by a single radiologist and the small number of studies in the literature about the Moskowitz artery.
Conclusions
Knowledge about the relationship between Riolan’s arch and the Moskowitz artery is valuable, and preoperative evaluation of this artery may be beneficial in the presence of Riolan’s arch. Also, preoperative radiological evaluation and its importance are prominent in minimising intraoperative bleeding during splenic flexure mobilisation with a medial laparoscopic approach and reducing the risk of colorectal anastomosis leakage in the postoperative period.








