Introduction
Superficial dermatophytoses are common fungal infections all over the world [1, 2]. Alarming data from India suggest that there is a dramatic increase in the prevalence of dermatophyte infections over the last 5 to 6 years. This may be considered as an epidemic or even hyperendemic situation [3]. Many patients treat themselves or undergo treatment by general practitioners or charlatans with dubious qualifications, usually with topical steroid combination preparations widely available without medical prescription [4]. This has a strong influence on the clinical manifestation of dermatophytoses in India, resulting in so-called steroid modified tinea or tinea incognita and widespread disease involving different anatomical regions which is often chronic and recalcitrant [5].
The data on the well-being of patients suffering from dermatophytoses are very limited in the literature.
Aim
The aim of this study was to assess the quality of life (QoL) in Indian patients with dermatophytosis seeking medical treatment and advice from dermatologists.
Material and methods
One hundred consecutive patients with dermatophytosis from two centres in India (Vadodara and Mumbai) were invited to participate in the study. Seventy-six of them agreed to be involved (76% response rate). Among them, 38 were females and 38 were male subjects. The age of patients ranged from 16 to 74 years, mean 32.2 ±14.4 years. The mean duration of the disease was assessed as 6.3 ±18.0 months (range: 0.1–144 months). Superficial dermatophytosis was diagnosed based on the typical clinical manifestation and the clinical suspicion was confirmed with a direct microscopic mycological examination (10% KOH). The study was approved by the local Ethical Committee.
The assessment of QoL impairment was performed based on the Dermatology Life Quality Index (DLQI) [6]. DLQI is widely used a dermatology-specific QoL questionnaire which comprises 10 questions relating to symptoms, feelings, daily activities, leisure, work, school, personal relationships and treatment. The total score ranges from 0 to 30 points; the higher the score, the lower the QoL. The cut-off points for DLQI have been proposed as follows: an index of 0–1 point indicates no effect at all on the patient’s life; 2–5 points a small effect; 6–10 points a moderate effect; 11–20 points a very large effect; and 21–30 points an extremely large effect [7]. Moreover, patients were asked to assess the presence and intensity of itch during the last 3 days using Numeral Rating Scale (NRS) [8].
Statistical analysis
Statistical analyses were performed using Statistica 12 software (StatSoft, Tulsa, USA). All data were assessed for parametric or nonparametric distribution. Pearson’s χ2 test was applied to sets of categorical data. Differences between groups were determined using the Mann-Whitney U-test as analyzed variables were of abnormal distribution. Correlations were determined by Spearman correlation analysis. The resulting p-values were considered nominally significant at p < 0.05 level.
Results
Among 76 patients with superficial dermatophytoses, the majority of them – 40 (52.6%) subjects – suffered from a combination of tinea corporis and tinea cruris, 16 (21.0%) from tinea cruris alone, 10 (13.2%) from tinea corporis alone. Five (6.6%) subjects were diagnosed with a combination of tinea corporis, tinea cruris and tinea faciei, 4 (5.3%) with tinea corporis and tinea faciei simultaneously, whereas 1 (1.3%) patient presented concurrent lesions of tinea cruris and tinea faciei (Table 1).
Table 1
Types of dermatophytoses and the quality of life according to the Dermatology Life Quality Index (DLQI)
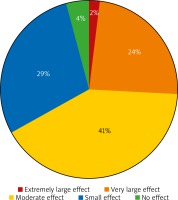
The mean DLQI score for the whole group of dermatophytosis patients was 8.2 ±5.1 points, indicating a moderate influence of patients’ QoL. A very large and extremely large effect was reported by 20 (26.3%) patients, moderate by 31 (40.8%), small by 22 (29%) subjects, while only in 3 (3.9%) patients the QoL was not influenced (Figure 1). Females were more heavily affected than males (9.3 ±5.2 and 7.1 ±4.7 points, respectively) (p = 0.038). Patients with a combination of tinea corporis, tinea cruris and tinea faciei demonstrated the lowest QoL (11.0 ±4.5 points), followed by those with tinea corporis and tinea cruris (9.0 ±5.4 points), tinea corporis (7.8 ±5.7 points) and tinea cruris (6.7 ±3.8 points) (Table 1).
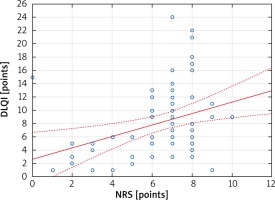
Figure 1
The impact of the superficial dermatophytosis on the sufferers’ quality of life as expressed by the Global Question indexing
Moreover, a significant correlation between the impairment of QoL and the intensity of itch (mean NRS score: 6.8 ±1.8 points) (r = 0.37; p < 0.002) was documented (Figure 2). Additionally, there was a clear trend (p = 0.11) towards lower QoL in patients who have been previously treated with topical agents containing corticosteroids (n = 32; 9.5 ±5.9 points vs. n = 44; 6.7 ±4.2 points). No relationships between the QoL impairment and patients’ age, socioeconomic status, profession as well as duration of dermatophyte infection were found (data not shown).
Discussion
Dermatophyte infections are common skin diseases worldwide, affecting skin as well as its appendages, such as hairs and nails. In general, instituting an appropriate antifungal therapy leads to a successful treatment outcome. However, certain clinical types of dermatophyte infections (e.g. onychomycosis) frequently constitute a long-lasting clinical problem [9, 10]. Additionally, steroid modified tinea can cause diagnostic difficulties and may lead to chronicity and recalcitrance [1, 3]. The psychosocial burden of dermatophyte infections has been reported very rarely up till now. The literature data are scant and the available studies mainly concentrated on the influence of onychomycosis on patients’ well-being, presumably by its chronicity [9, 10]. The review of DLQI usage during the first 10 years of its availability showed that the instrument was used in one study involving only 10 patients with tinea [11]. The authors demonstrated that the mean DLQI value in those subjects was 5.5 points, which can be considered as a small effect on patients’ life. The next review of the DLQI usage published in 2008 did not disclose any new findings in this area [12]. However, a recently published study by Patro et al. [13] assessed the DLQI scores among 294 patients with superficial dermatophyte infections. The overall effect on the QoL was moderate among males, subjects with shorter duration of lesions (no more than 6 months), patients with less extensive disease (less than 10% of the Body Surface Area involved) and patients of low to medium socio-economic status. In contrast, a very large effect on the DLQI concerned females, patients with longer duration of lesions, more extensive area of skin involvement, high socio-economic status and those with medium to high education. Moreover, the disability domain of the 5D-pruritus scale was correlated with the DLQI disability score (r = 0.8, p < 0.0001).
The current epidemic situation in India has led our group to conduct the clinical study on the superficial dermatophytoses and the QoL. To the best of our knowledge, this is the second largest series of patients with tineas in which QoL has been assessed. We have clearly documented that superficial dermatophytoses may be responsible for moderately decreased QoL. The difference between our results and the initial study might be due to the limited number of patients with lower disease severity included by Jobanputra and Bachmann [14] and possibly due to the fact that during the recent decades there has been a shift in the aetiology of dermatophytoses (from the predominant Trichophyton rubrum to Trichophyton mentagrophytes – a species that can lead to more inflammatory and widespread lesions) [15]. Moreover, similarly to the recent Indian study [13], we have documented that the QoL impairment may be related to the number of skin areas involved and also the intensity of itch. Patients suffering from coexistence of tinea corporis, tinea cruris and tinea faciei reported a very large impact of the skin condition on their life. This is in concordance with other studies on different dermatoses as well, in which correlations between impaired QoL and disease severity, and additionally the intensity of itch, were reported [16–18]. Interestingly, our results indicate that previous treatment of dermatophytosis with topical agents containing corticosteroids may be associated with a trend towards lower QoL. This could be due to the fact that topical corticosteroid therapy may contribute to the prolonged course of the disease and more widespread infection [1, 3, 15].
There are several limitations of our study. Firstly, there was a relatively small number of the participants. Secondly, the findings in this cohort may not necessarily reflect the situation in the general population. Lastly, the confirmation of the diagnosis of dermatophytoses was based upon the clinical picture and direct KOH examination, whereas neither fungal culture nor polymerase chain reaction were performed in our patients. The lack of fungal culture made the definite identification of certain species of fungi impossible. Additionally, as different kinds of dermatophytes are associated with more or less marked inflammatory cutaneous lesions, we speculate that this issue may possibly influence the quality of life to a different extent. As a result, the impact of different species of dermatophytes on the quality of life remains to be explored in the future. However, fungal culture does not always yield positive results, especially if there is a difficulty in maintaining the wash-out period between the last application of topical medications and the procedure of obtaining the specimen. Currently, the diagnosis of dermatophytoses in India still relies mainly on the clinical picture and direct KOH examination. Unfortunately, due to economic issues, performing culture and subsequently identifying the causative organisms is problematic in most situations. This issue may be obviously regarded as a problem not only in India, but possibly in several other countries in which healthcare is underfinanced. Despite the value of fungal culture as the gold standard in the diagnosis of dermatophytosis, the Expert Consensus on The Management of Dermatophytosis in India (ECTODERM India) does not recommend its routine use in clinical practice [19]. This method should be considered in cases which are recalcitrant or involving multiple areas.
Conclusions
Our study emphasizes the influence of superficial dermatophytoses on the QoL. The alarming increase in the incidence of tinea in India, majorly due to the unsupervised usage of combination creams containing corticosteroids, leads to altered clinical manifestations, widespread disease and prolonged duration of superficial dermatophytoses. As a result, the well-being of the affected subjects is impaired. The responsible authorities should take these facts seriously into consideration in order to develop strategies to combat this problem.