Introduction
The primary role of the eyelid is to protect and moisturise the eye. Any sort of neoplasm affecting the eyelid may cause its malposition and in consequence be vision-threatening for the patient.
Anatomically, the eyelid has four layers: skin with thin subcutaneous tissue, striated muscle (orbicularis oculi), tarsal plate and conjunctiva. The skin covering the eyelids is thin, unlike in other regions of the body, and does not contain a layer of subcutaneous fat. It has, however, typical histologic composition of the normal skin: keratinised epithelium, melanocytes, blood and lymphatic vessels, nerve fibres and several types of glands: sweat glands, apocrine glands (glands of Moll) and sebaceous glands (glands of Zeiss). A second layer of the eyelid contains the orbicularis muscle (‘purse’ muscle) that covers the whole entrance to the orbit and is responsible for closing the eyelids and for the lacrimal pump. A third layer is a tarsus or tarsal plate composed of thick connective tissue. The tarsi give the eyelid its shape and firmness. What is more, they contain a number of sebaceous glands called the Meibomian glands that are responsible for the stability of the tear film on the surface of the eye. The fourth layer of the eyelid is the palpebral conjunctiva that contains typical conjunctival epithelium and stroma, numerous glands including goblet cells that secrete mucus, which is another ingredient of the tear film [1].
Despite the relatively small surface area comparing to the skin in other regions, approximately 5–10% of all skin cancers originate from the eyelids, primarily [2] because of their exposure to sunlight and environmental factors.
Aim
The aim of this study was to assess the prevalence of different types of benign and malignant skin lesions in the area of eyelids basing on the tertiary centre experience.
Material and methods
Data of patients treated at the Department of Ophthalmology, Poznan University of Medical Sciences between January 2013 and January 2017 were retrospectively reviewed. Patients were included in the study if they underwent the surgical treatment for the eyelid lesions with a histopathological report. They were excluded if the patient underwent previous surgery for palpebral mass or if the lesion penetrated into the orbit or affected the bones.
The histopathology techniques included standard H + E sections and when needed immunohistochemical studies, too. Collected data included age, gender, location and the type of the tumour.
Results
Five hundred, fourty-four patients were identified, 201 men and 343 women in the mean age of 60.5 years (range: 18–92). All the lesions were surgically removed with standard reconstruction techniques. There was a slight predominance in the affected side, with majority of the lesions (57%) located in the left eyelids.
Among all 544 eyelid lesions included in the study, 429 (79%) tumours were benign and 115 (21%) – malignant. In the benign group, the most common finding was chalazion (49.2%) followed by squamous papilloma (22.8%), seborrheic keratitis (10%), epidermal cyst (8.2%), and intradermal nevus (5.1%). The detailed diagnoses of benign lesions are listed in Table 1, and some typical examples shown on Figures 1–3.
Table 1
Prevalence of benign lesions in the studied group
| Lesion | N | % |
|---|---|---|
| Chalazion | 211 | 49.2 |
| Squamous papilloma | 98 | 22.8 |
| Seborrheic keratitis | 43 | 10.0 |
| Epidermal cyst | 35 | 8.2 |
| Intradermal nevus | 22 | 5.1 |
| Pyogenic granuloma | 8 | 1.9 |
| Hidrocystoma | 7 | 1.6 |
| Molluscum contagiosum | 5 | 1.2 |
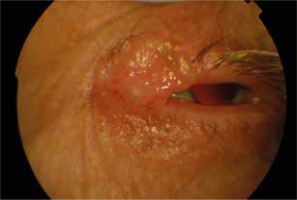
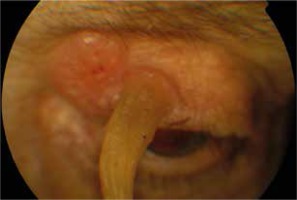
Out of all malignant lesions, the most common diagnosis was basal cell carcinoma (BCC) in 110 (95.5%) patients. Squamous cell carcinoma (SCC) was diagnosed in 3 (2.6%) patients and sebaceous gland carcinoma (SGC) in 2 (1.7%). Table 2 contains the detailed diagnoses of malignant lesions. Figures 4 and 5 show basal cell carcinoma and Figure 6 shows a squamous cell carcinoma with a cutaneous horn.
Table 2
Prevalence of malignant lesions in the studied group
| Lesion | N | % |
|---|---|---|
| Basal cell carcinoma | 110 | 95.7 |
| Squamous cell carcinoma | 3 | 2.6 |
| Sebaceous gland carcinoma | 2 | 1.7 |
In the BCC group, the most frequent location of the tumour was the lower eyelid – in 78%. The upper eyelid was affected in 15% and the medial canthal area in 8%. According to histopathology, 46 BCC lesions (41.8%) were nodular, 12 (10.9%) were ulcerative and 10 (9.1%) superficial. In 42 cases (38.2%), the histopathology report did not include the type of BCC. All histopathology diagnoses are listed in Table 3.
Discussion
This is a study reporting the incidence of various eyelid skin lesions basing on the single-centre experience. The majority of analysed lesions were benign (79%).
Deprez et al. [3] in their extensive study, described the prevalence of 5504 eyelid tumours. The authors reported that benign tumours represented 84% of all eyelid lesions, which is consistent with our findings in the present study. The most common lesions were squamous cell papilloma (26%), seborrheic keratosis (21%), nevus (20%), hidrocystoma (8%), and xanthoma/xanthelasma (6%). The difference in this study is that we included chalazia in the study group and it was the most common benign finding. Huang et al. [4] reported that the most frequent benign subtypes were intradermal nevus (57.8%) followed by seborrheic keratosis (12.6%), xanthelasma (11.2%) and epidermal cyst (8.2%). Gundogan et al. [5] analysed 1502 cases of eyelid lesions, of which 87.2% were benign. Among those, the most prevalent were squamous papillomas (37.0%), followed by seborrheic keratoses (29.3%) and epidermal cysts (12.2%). The similarities and differences in the incidence rates of benign tumours can be perhaps attributed to racial and regional distribution factors. Absence of xanthelasma findings in this study is caused by the fact that the diagnosis is made mostly by clinical observation, while this study relied on histopathology results only.
In all previously cited studies, basal cell carcinoma accounted for the most commonly seen malignant eyelid tumour. Deprez et al. [3] reported its incidence in 86%, Gundogan et al. [5] in 95.5% of malignant eyelid lesions. This high incidence of BCC is also confirmed by other authors [6, 7] as well as by our study. There are some reports showing that the prevalence of BCC increases over time [8]. The treatment of choice, especially in the high-risk area of the eyelid is surgical removal using the Moh’s technique or a large margin of 2–4 mm [9, 10]. Other treatment modalities include radiotherapy or immunotherapy [9].
Squamous cell carcinoma is the second most common malignancy of the eyelid accounting for 5–10% of all malignant eyelid lesions [3, 11, 12]. Even though SCC is not as common as BCC, it could be much more invasive for the patient as it may metastasise to lymph nodes as well as to the central nervous system due to the perineural invasion [13]. Because of that, the treatment of choice is surgical resection with a more significant margin (4–6 mm) [14].
Other authors suggest that sebaceous gland carcinoma is the second most common eyelid malignancy [15, 16] with 34–38% of prevalence rates. It is unclear why this study showed a much lower incidence rate of 1.7%. Of note, factors such as geographical and racial variations as well as a smaller study group have to be taken into consideration. Sebaceous gland carcinoma may arise from sebaceous glands of the eyelid such as Meibomian glands of the tarsus or Zeiss glands of the hair follicle of the eyelash. It is a particularly dangerous eyelid tumour because it may masquerade as an inflammatory condition and its high metastasis rates reaching up to 41% [17].
We did not observe in our analysed group cutaneous malignant melanoma arising from the eyelid. However, its occurrence in other studies is also small, accounting for 0.5–3% of all eyelid tumours [15, 18]. Most eyelid melanomas are likely to evolve from lentigo maligna precursor lesion that progresses to lentigo maligna melanoma or from a dysplastic nevus. A cutaneous malignant melanoma may invade the lid margin and conjunctiva, in which cases it may be impossible to differentiate if the melanoma originates from the conjunctiva or the skin. Such cases have worse prognosis [19].