Introduction
Vitiligo is an acquired chronic depigmenting disorder of the skin, predominantly asymptomatic, characterized by amelanotic macules and patches that affects 0.5% to 2% of the world’s population [1]. Its prevalence is not related to age or ethnicity, more than half of cases occur before the age of 20 years and 95% of all cases are under the age of 40 [2–5]. The cause of the disease is uncertain but seems to be dependent on the interaction of genetic, immunological and neurogenic factors [6, 7]. Although vitiligo does not cause direct physical impairment, it is commonly believed that it can produce a significant psychosocial burden [8]. Numerous studies have demonstrated a varying form of stigmatization, defined as a process in which skin appearance is negatively judged and persons who are affected experience absence of acceptance because of their visible symptoms. Patients experience distress and anxiety, are often glared at or even avoided in fear of infection or disgust. Patients have various degrees of emotional disturbances, including low mood, loss of pleasure, poor body image, poor self-care, low self-esteem, and high stress [9, 10]. Other authors show that many vitiligo patients feel distressed and stigmatized by their condition, especially in relation to social activities [11]. It is also believed that exposing the body causes anxiety and embarrassment, which in more intimate encounters may have a negative effect on sexual relationships [12]. In other words, there appears to be an impact of vitiligo on the overall patient quality of life (QoL) [13]. Nevertheless, vitiligo is often regarded as a cosmetic issue, and impairment of QoL tends to be underestimated [14].
A disease-specific questionnaire for vitiligo has been developed and validated in the English language: the vitiligo-specific quality of life instrument (VitiQoL) [5]. The VitiQoL is a questionnaire of 15 items, with item scores from 0 (never) to 6 (all the time). It yields a total score from 0 to 90. Question 16 of the VitiQoL questionnaire is a self-reported severity scale ranging from 0 (no skin involvement) to 6 (most severe case). The questionnaire proved to be a promising clinical and epidemiological study instrument, and a powerful marker of the treatment outcome. An exploratory factor analysis with oblique rotation yielded 3 factors: participation limitation, stigma, and behaviour. The instrument was translated, culturally adapted and validated into Brazilian Portuguese (VitiQoL-PB) [15] and Iranian [16].
Aim
The aim of this study was to perform the translation, cross-cultural adaptation and validation of the VitiQoL into Polish (VitiQoL-PL). What is more, we are the first to use it through an online survey.
Material and methods
Two bilingual physicians translated the English version of the VitiQoL questionnaire to Polish, then the Polish version was translated to English by other two bilingual dermatologists who had not read the original questionnaire (back to back translation). Afterwards, the final version was compared with the original English version. The authors of the VitiQoL questionnaire authorized its translation and cross-cultural adaptation.
The study was conducted online on 97 patients with vitiligo from our private outpatient departments in Gdynia and Gdansk, Poland from May 2018 to December 2019. Based on the original study and the WHO recommendations for the development of quality of life questionnaires, a specific questionnaire on demographic data, the VitiQoL questionnaire (Table 1) and a generic instrument for dermatological diseases, the DLQI (Dermatology Life Quality Index) (Table 2), were administered to 97 subjects. The VitiQoL questionnaire consisted of 15 questions with a seven-point Likert scale (0–6). The final scores could range from 0 to 90, in which patients with higher scores showed poorer quality of life.
Table 1
VitiQoL questionnaire
Table 2
DLQI questionnaire
In addition, subjects made a personal assessment of their severity of vitiligo, using a scale ranging from 0 (no skin involvement) to 6 (most severe cases), which corresponded to question 16 of the VitiQoL questionnaire.
Patients were enrolled based on their consent and data were analyzed with respect to their confidentiality.
Statistical analysis
The qualitative features were analyzed using the χ2 test using the Pearson method. Independent quantitative variables meeting the assumptions for parametric tests were analyzed using the Student’s test. Quantitative variables that did not meet the assumptions of parametric tests were analyzed using non-parametric tests: the Mann-Whitney U test or the Kruskal-Wallis test. Spearman’s correlation coefficient was used to describe the correlation strength of two features (VitiQoL-PB and DLQI). In all tests, p < 0.05 was considered to be a significant level of statistical significance. Statistical calculations were made using Statistica, version 12.0. (StatSoft, Inc. 2015). Additionally, the Cronbach’s α coefficient was used to check the reliability of the VitiQoL-PB questionnaire.
Results
The questionnaire was completed by 97 patients. Their demographic and clinical characteristics are described in Table 3. The average VitiQoL-PL score was 39.65 ±23.34; while the median DLQI was 4.0 (interquartile range P25 = 2 and P75 = 10). Overall, women had poorer QoL (higher VitiQoL scores) than men, 49.79 ±21.50 and 27.45 ±19.45, respectively. The educational level had no impact on the VitiQoL result (p = 0.43). In our group, Singles scored: 55.07 ±21.93, folloved by Divorced/Separated: at 47.66 ±21.66, and Widowed: at 27.00 ±19.67. In our study, the impact of previous/ongoing therapy was significant (p = 0.008). Patients that were previously treated for vitiligo got VitiQoL medium scores at 46.32 ±19.15 and a group without any treatment prior to current scored 34.98 ±24.99. The patients that were treated with phototherapy scored higher at 48.44 ±18.64 than the group of patients that never had such a treatment at 37.65 ±23.93. The single item that most contributed to the VitiQoL-PL score was related to feeling bothered by the appearance of the skin (question 1). Other items that significantly contributed to the final score were: feeling frustration about the skin condition (question 2), embarrassment or inhibition because of the skin (question 7) and social or leisure activities (question 9).
Table 3
Demographic and clinical characteristic of our patients
We have also found a strong correlation between gender and QoL in the DLQI results: women showed higher results: 8.15 ±5.32 compared to 3.79 ±4.03 in men. DLQI scores in certain martial status groups looked similar to VitiQoL, with Singles reaching 10.28 ±5.83, Divorced/ Separated at 7.16 ±4.76 and Married with the lowest result at 3.54 ±3.10. The impact of previous/ongoing therapy on VitiQoL was statistically significant (p = 0.015). Previously treated patients got higher scores (7.17±4.81 to 5.47±5.44) but this time treatment method had no impact on the final score.
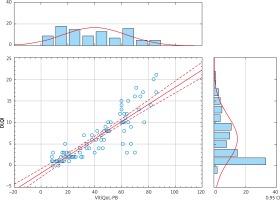
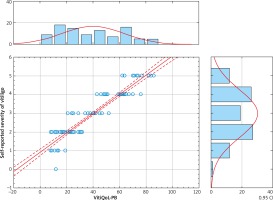
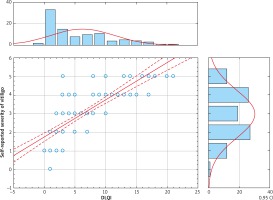
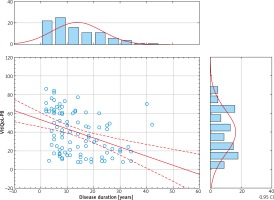
There was a significant correlation between VitiQoL and DLQI (r = 0.90, p < 0.001) (Figure 1) and also between VitiQoL-PL and subjects’ assessment of the severity of their disease (r = 0.94, p < 0.001) (Figure 2). We also found a good correlation between the total DLQI and subjects’ assessment of the severity of their disease (r = 0.87, p < 0.001) (Figure 3).
Discussion
There are many disease-specific instruments for the evaluation of severity or QoL of a certain dermatosis, such as atopic dermatitis, acne and melasma. Until 2012 and the development of VitiQoL there were none specific to vitiligo. In Poland, physicians treating this disease still do not have a specific instrument for assessing patients QoL, and have to administer other non-vitiligo specific questionnaires to do so. In this study, the Polish version of a specific index for estimating quality of life of patients with vitiligo was developed (Table 4).
Table 4
Polish version of VitiQoL questionnaire
Previously, the instrument was translated, culturally adapted and validated only into Brazilian Portuguese (VitiQoL-PB) [15] and Iranian [16]. In our study, VitiQoL total score was lower than in Portugal – 39.65±23.34, in comparison to 40.04+27.32 but higher than in Iran – 30.5±14.5. Similar to the Persian study, education had no impact on QoL which is a little unexpected, because patients with a university education should be more aware of the nature of the problem and less worried about any potential consequences, and hence have better quality of life. This may be a result of gaining knowledge about the disease from other media like the internet which are becoming more impactful when it comes to patients self-studying. Female patients reported poorer QoL in all 4 studies, which was logically predictable, since all over the world, aesthetic issues are more considerable in women. This demonstrates a strong relationship between gender and QoL and more attention should be paid to this group. Patients that were previously cured had higher VitiQoL-PL scores. Phototherapy treatment was statistically significant and the results showed that patients subjected to this kind of treatment had lower QoL. In contrast to the Iranian study, there was no association between VASI of exposed areas and quality of life. This was an unexpected discovery because we anticipated that patients with high VASI scores that are mainly cured with phototherapy would have higher VitiQoL scores and thus lower QoL.
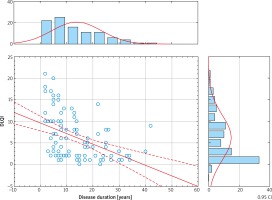
Regarding life quality and duration of the disease, the Persian group found that patients who had disease duration of 5 years or less and patients with 15–20 years of disease duration had better quality of life, although it was not statistically significant. In our study, there is a statistically significant negative correlation between DLQI, VitiQoL and disease duration. As the vitiligo continues, the DLQI and VitiQoL values decrease (Figures 4, 5).
The VitiQoL-PL Cronbach’s α coefficient was similar to the coefficient of the original questionnaire and two other validations (our VitiQoL Cronbach’s α = 0.98, original = 0.935, Brazilian = 0.944, Persian = 0.956), which demonstrates the reliability of the instrument. Additionally, it showed a strong correlation with both the subjects’ assessment of disease severity and the DLQI. In the original VitiQoL, one of the limitations highlighted by the authors was the fact that the instrument should be validated and then used through the digital route of administration. We successfully managed to do so and have administered the questionnaire via an online survey. We hope that from now on the impact of vitiligo on the quality of life in Poland can be assessed using a disease-specific questionnaire, which will contribute to a more complete and reliable evaluation of these patients. Because of our work, physicians in Poland can now compare results of their studies of vitiligo and we all can correlate our work with international data.