Femoral neck fractures are one of the most common orthopaedic injuries, especially in old age [1]. Hip fractures are life-threatening events with a high risk of morbidity and mortality, so appropriate treatment of such conditions is lifesaving, and surgical replacement whether total or hemi-arthroplasty is the cornerstone of treatment [2]. Recent studies have shown that the one-year mortality rate after a surgically corrected hip fracture is about 21% compared to a 70% one-year mortality for untreated cases [3]. Pain is one of the most burdensome postoperative symptoms and is experienced by all patients undergoing hip arthroplasty. Proper control allows rapid recovery, decreases sympathetic stimulation thereby decreasing the incidence of cardiac and pulmonary complications [4], decreases the incidence of developing chronic pain syndromes, and facilitates rapid discharge from the hospital [5].
Recent guidelines favour the use of multi-modal analgesia for adequate pain control with a preference for site-specific regional techniques over continuous neuraxial techniques to facilitate Early Recovery After Surgery (ERAS) protocols [6]. Patients with femoral neck fractures are also at high risk for venous thromboembolism (VTE) and are usually prescribed high doses of anticoagulants perioperatively, a factor that should be considered before using continuous neuraxial techniques [6].
The hip joint capsule is innervated anteriorly by the femoral nerve and obturator nerve. It is poste-riorly innervated by the nerve to the quadratus femoris muscle and occasionally by the superior gluteal and sciatic nerves [7].
Many regional nerve blocks are used in hip arthroplasties including fascia iliaca block, femoral nerve block, pericapsular nerve group block (PENG), and quadratus lumborum block; the block of choice is still a matter of debate [8].
Fascia iliaca block affects the femoral nerve, obturator nerve, and lateral femoral cutaneous nerve. It can be used for the management of hip fractures in emergency rooms and hip arthroplasties [9].
Quadratus lumborum block (QLB) is a relatively new regional technique with a vague mechanism of action used mainly for upper and lower abdominal procedures. Recently many clinical trials have examined its benefits in hip surgery [9].
Anterior QLB reduces the length of hospital stay and opioid use; it provides early and rapid pain relief and allows early ambulation. However, some branches responsible for innervations of the hip joint are not affected by QLB, which should be taken into consideration [10].
There are 3 different types of QLB: the lateral, posterior, and anterior approaches. Different approaches have different mechanisms of action. The lateral block spreads to the transversus abdo-minis plane, the posterior block is associated with spread to the thoracolumbar fascia, and the anterior block seems to spread to the lumbar spinal nerves and the thoracic paravertebral space [11].
Various studies have demonstrated the positive effects of fascia iliaca block (FIB) in reducing pain resulting from hip fractures and reducing total opioid consumption [12]. There are 2 main approaches for the FIB: the supra-inguinal approach and the infra-inguinal approach. Although the infra-inguinal approach is easier and safer compared to the supra-inguinal approach, various studies have shown that its sensory block was inferior to the supra-inguinal approach [13].
In the era of fast-track protocols for total joint arthroplasties, there seems to be no ideal regimen for post-operative pain management.
In this study, we aimed to examine the effect of supra-inguinal FIB compared to anterior QLB in the management of perioperative pain in patients undergoing hip arthroplasties.
METHODS
Ethical approval and trial registration
Ethical approval for this study (FMASU R 118/2021) was provided by the Research Ethics Committee of the Faculty of Medicine, Ain Shams University, Abbasia, Cairo, Egypt (Chairperson Prof F. Tash) on 27/5/2021.
The study was prospectively registered at Clinical Trial Registry Clinical Trials.gov Identifier: NCT05504525.
Patients recruitment
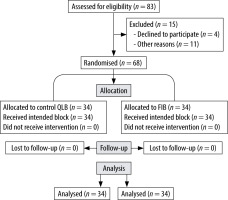
After obtaining written informed consent from all subjects, patients were recruited to this study by our anaesthesia residents from our clinic. Sixty-eight patients were enrolled in this study, which took place at Ain Shams University Hospitals between May and December 2022.
We enrolled adult male and female patients, scheduled for hip operations due to femoral neck fractures aged between 40-60 years with ASA status I-III. Patients who refused to participate or had a history of local anaesthetic allergy, local infection at the injection site, or usage of anticoagulant therapy were excluded.
Study design
This was a randomised prospective study and patients were divided into 2 parallel study groups:
Group (F): Patients who received ultrasound- guided supra-inguinal fascia iliaca block S-FIB.
Group (Q): Patients who received ultrasound-guided anterior QLB.
All patients were clinically examined, routine preoperative investigations were done, and they were informed about the visual analogue scale (VAS) and the numerical rating scale (NRS), and how to use them, by the investigator.
Anaesthesia and surgical procedure
On arrival at the operating room, monitors were applied to the patients. A peripheral cannula was inserted. Every patient received 0.05 mg kg–1 mida-zolam as preoperative sedation, then the anaesthe-tic block was done.
Group (F): Patients received ultrasound-guided supra-inguinal fascia iliaca block under a complete aseptic technique using ultrasound with a 10–15 MHz linear transducer (SonoSite M-Turbo C). The patient was positioned supine with the hip extended, the anterior superior iliac spine ASIS was palpated, and the ultrasound probe was placed inferomedially. The iliacus muscle with the fascia iliaca superficial to it was recognized as superficial to the ilium. Superficial to the fascia iliaca, the deep circumflex iliac artery was identified between the internal oblique and fascia iliaca to avoid it while introducing the needle [13].
An echogenic B-bevel 22 G needle (Stimpulex® D, B.Braun) was inserted in-plane from the inferior aspect of the probe. After piercing the fascia iliaca, the needle was slightly withdrawn to the superficial border of the iliacus. Then, 1–2 mL of local anaesthe-tic was injected to confirm the separation between the hyperechoic fascia iliaca and the iliacus muscle beneath it. The needle was advanced cephalad into the pocket of local anaesthetic, and 40 mL of bupivacaine 0.25% was injected with frequent aspiration to avoid any inadvertent vascular injection [14].
Group (Q): Patients received ultrasound guided anterior QLB under a complete aseptic technique, using the same ultrasound in the lateral position. The transducer was placed parasagittal 3–4 cm lateral to the midline over the sacrum to identify the L5 transverse process. The latissimus dorsi aponeurosis (laterally), QL muscle, psoas major muscle, and L5 transverse process (medially) were visualized [15]. An echogenic needle (Stimpulex D®, B.Braun) was introduced in plane laterally, through the latissimus dorsi aponeurosis and QL muscle to position the tip between the QL and psoas major muscle close to the transverse process. Correct needle tip position was confirmed by injecting 2 mL of local anaesthetic. Once the proper position was confirmed, 40 mL of bupivacaine 0.25% was injected anterior to the QL muscle at the level of its attachment to the transverse process of the L4 vertebra [16].
A successful block was ensured by the patient reporting tingling and numbness in the anterior and medial aspects of the thigh. 30 minutes after administration of the block the patient was seated for the administration of spinal anaesthesia and quantitative relief of pain using the VAS was assessed before administration of spinal anaesthesia, which was given via a 25 G spinal needle using 3 mL of hyperbaric bupivacaine 0.5%, and the patient was monitored through the operation for pulse, oxygen saturation, ECG, and MAP.
Measurements and outcomes
VAS during seating the patient when applying the neuraxial block.
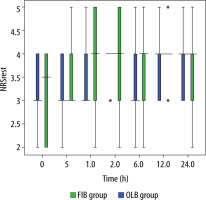
Postoperative pain assessment: Using the NRS score at rest during the immediate postoperative period (0 min), and at 30 min, 1, 2, 6, 12, and 24 hours. The assessment was done by an independent anaesthesiologist who had no role in applying the block or intraoperative management of the patient. All patients received paracetamol 15 mg kg–1 IV (500 mg or 1 gm) at an interval of 6 hours in the postoperative period. However, if the patient had pain in between, he/she was asked to inform the nursing staff who informed the attending anaesthesiologist. If NRS > 4 at any time, then rescue analgesia in the form of morphine 5 mg IV was given if the pain persisted after 30 minutes the patient was given another dose of morphine.
The total dose of morphine required in 24 hours was documented.
Side effects of opioids such as nausea, vomiting, respiratory depression, and itching were noted. Postoperative nausea and vomiting (PONV) were assessed using a 4-point numerical scale (0 = no PONV, 1 = mild nausea, 2 = severe nausea or vomi-ting once, and 3 = vomiting more than once). If the score was 2 or more, then ondansetron 0.1 mg kg–1 IV was given as a rescue antiemetic.
Patient satisfaction was evaluated and recorded 24 hours after surgery on a 7-point Likert scale (1 – extremely dissatisfied, 2 – very dissatisfied, 3 – dissatisfied, 4 – neither satisfied nor dissatisfied, 5 – satisfied, 6 – very satisfied, 7 – extremely satisfied).
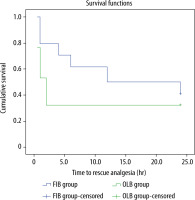
The primary outcome of the study was the duration of postoperative analgesia (i.e. time to first analgesic request from the time of applying the block). The secondary outcome was to measure the VAS while the patient was sitting during application of the neuraxial block, the total morphine requirement in the postoperative period, patient satisfaction in the postoperative period, and the frequency of adverse effects.
Sample size
According to previous studies [17, 18], the sample size was calculated using the G power program. Based on a 50% reduction in the total morphine consumption postoperatively for 24 hours (the primary outcome) with the power at 90%, a error 0.05%, and assuming a large effect size for the difference between the two groups corresponding to a Cohen D coefficient value of 0.8, a sample size of 68 patients was needed (34 patients in each group) and was sufficient to achieve the study objective.
Statistical analysis
Data were collected, coded, tabulated, and then analysed using SPSS Statistics for Windows version 16 (IBM, Armonk, NY, USA). Numerical variables were presented as mean (standard deviation) or median (Q1–Q3) as appropriate and compared using the t-test or Mann-Whitney test respectively. Time to rescue analgesia was analysed using Kaplan-Meier survival analysis and the Breslow (generalized Wilcoxon) test for between-group comparison. Any difference with a P-value < 0.05 was considered statistically significant.
RESULTS
A total of 68 patients were enrolled in the study (Figure 1). Demographic data were similar between groups with 17 males and 17 females participating in the QLB group with a mean age of 53.35 ± 6.03 and 19 males and 15 females participating in the FIB group with a mean age of 55.47 ± 4.50. ASA classification distribution between groups was non-significant as shown in Table 1.
TABLE 1
Demographic data including age, sex, and ASA classification among the 2 groups
| Variable | Group QLB | Group FIB | P-value |
|---|---|---|---|
| Age (years), mean ± SD | 53.35 ± 6.03 | 55.47 ± 4.50 | 0.1060 |
| Sex, M/F, n | 17/17 | 19/15 | 1.00 |
| ASA, I/II/III, n | 5/20/9 | 4/19/11 | 0.84 |
The group receiving supra-inguinal FIB showed a significant increase in the duration of analgesia with a mean duration of 18 (4–24) hours compar- ed to the group receiving anterior QLB, which showed a mean postoperative analgesia duration of 2 (1–24) hours and a P-value of 0.005 (Table 2, Figure 2).
TABLE 2
Time to first rescue analgesic dose, total morphine consumption, and VAS during patient positioning to receive spinal anaesthesia
| Variable | Group QLB | Group FIB | P-value |
|---|---|---|---|
| Time to rescue analgesia (hours) | 2 (1–24) | 18 (4–24) | 0.005 |
| Total morphine consumption (mg) | 6.9 ± 1.87 | 5.3 ± 0.9 | 0.0086 |
| VAS during seating | 5.12 (2.65) | 3.85 (2.55) | 0.0096 |
Although pain scores in the group receiving anterior QLB were higher than in the other group, statistical analysis showed no significant difference (Figure 3).
FIGURE 3
Box and whiskers diagram, showing median, IQR, and total range of NRS at rest in both groups
The total morphine consumption in 24 hours was significantly lower in the group receiving supra-inguinal FIB with a mean consumption of morphine 5.3 ± 0.9 mg compared to 6.9 ± 1.87 mg and a P-value of 0.0086 (Table 2).
The VAS during positioning the patient showed a significant difference between the groups, 3.85 ± 2.55 in the supra-inguinal FIB compared to 5.12 ± 2.65 in the anterior QLB group and a P-value of 0.0096 (Table 2).
Overall patient satisfaction showed no significant difference between groups (Table 3).
TABLE 3
Overall patient satisfaction
| Groups | Total | ||||
|---|---|---|---|---|---|
| FIB group | QLB group | ||||
| Patient satisfaction | 3 | Count | 7 | 7 | 14 |
| % within groups | 20.6 | 21.2 | 20.9 | ||
| 4 | Count | 10 | 17 | 27 | |
| % within groups | 29.4 | 51.5 | 40.3 | ||
| 5 | Count | 17 | 9 | 26 | |
| % within groups | 50.0 | 27.3 | 38.8 | ||
| P-value | 0.207 | ||||
Side effects including respiratory depression and itching were not reported in either group, and PONV scores were not significantly different between groups (Table 4).
DISCUSSION
In this clinical trial, we compared the perioperative analgesia resulting from supra-inguinal FIB and anterior QLB in patients undergoing hip surgery. We found that patients who received supra-inguinal FIB had prolonged analgesia compared to the other group. They were more comfortable during positioning to receive spinal anaesthesia, and they received significantly smaller amounts of opioids in the postoperative period. Although patients receiving FIB had better perioperative analgesia profiles overall, patient satisfaction showed no significant difference between groups.
Our findings were contrary to the findings of Hashmi et al. [8], when they compared the effect of FIB to QLB in elective hip replacement. This difference could be attributed to the different approaches used in the 2 studies. We used the supra-inguinal approach, which is well known for having a superior analgesic effect compared to the infra-inguinal approach [13, 16]. Another factor that could attribute to the difference between the studies is the larger volume that we used to achieve the block; while Hashmi et al. used 20 mL of bupivacaine 0.25%, we used 40 mL, which is well tolerated in patients and does not exceed the toxic dose of 2.5 mg kg–1 of bupivacaine.
Our study contradicts the findings of Blackwell et al., who found that posterior quadratus lumborum was superior to fascia iliaca block in hip arthroscopy, and that difference could derive from many factors. Their study was a retrospective study, which is an inferior level of evidence compared to randomized prospective studies. We found that some patients in the group assigned to the fascia iliaca block received femoral nerve block only, which makes the results questionable. Not all patients received the same form of postoperative opioids, some being converted to morphine equivalents, many patients received local infiltration of LA after the procedure, and the exact form of fascia iliaca block, whether supra- or infra-inguinal, was not mentioned [19].
LIMITATIONS
The major limitation of our study was the lack of blinding, but we tried to avoid any bias by using 2 different pain scales – the VAS and the NRS – and at the end, we measured the overall patient satisfaction from the whole experience. Another limitation was that we did not measure the levels of serum bupivacaine as we used a relatively large dose although pharmacologically safe.