Hemiarthroplasty is a surgical procedure during which one half of the hip joint is replaced with a prosthesis, leaving the other half intact. Spinal anaesthesia is a common anaesthetic technique for that procedure. Unfortunately it can cause rapid haemodynamic alterations detrimental to the geria-tric patients.
Sympathetic blockade in spinal anaesthesia causes a fall in systemic vascular resistance and central venous pressure with resultant hypotension. Severe hypotension may be harmful in the elderly population due to limited physiological reserve and increased incidence of systemic illnesses [1]. Hypotension is proportional to height of spinal anaesthesia block [2]. Higher block produces extensive sympathetic blockade with a subsequent fall in systemic vascular resistance.
Unilateral spinal anaesthesia is a mode of subarachnoid blockade which produces a predominant motor and sensory block on one side. It was first described by Tanasichuk et al. [2] in 1961. Unilateral block restricts the extent of sympathetic blockade, and hence shows minimal haemodynamic changes as compared to bilateral block [2]. It can produce adequate anaesthesia with minimal cardiovascular instability.
Previous studies in young patients comparing unilateral and bilateral spinal anaesthesia showed a lesser degree of hypotension with unilateral block [3, 4]. Tekye et al. [4] observed delayed onset of spinal anaesthesia in patients receiving unilateral block. Bacak et al. [5] and Fanelli et al. [6] observed prolonged motor blockade in the operated limb in patients receiving unilateral spinal anaesthesia.
There is a paucity of comparative studies evaluating the effects of unilateral versus bilateral spinal anaesthesia in the elderly population. Therefore, the aim of this study was to compare the effects of unilateral and bilateral spinal anaesthesia in geriatric patients undergoing hemiarthroplasty in terms of suitability of the block and the degree of haemodynamic stability.
METHODS
After obtaining Institutional Ethics Committee approval and written informed consent from each patient, this prospective, parallel group, randomized, controlled study was conducted in the Orthopaedics Operating Room of Calcutta National Medical College. Patients aged 60–85 years, of either sex, ASA physical status I and II, undergoing hemiarthroplasty under spinal anaesthesia were included in this study. Patients with contraindications to spinal anaesthesia, allergy to bupivacaine or fentanyl, body mass index over 30 kg m-2, height less than 150 cm, ASA physical status III or more were excluded from the study. Patients who were unable to be placed in a lateral decubitus position and patients receiving antihypertensive or vasodilator agents were also excluded from the study.
Using a computer-generated random number list patients were randomly allocated to two groups, group U and group B. Patients in group U received unilateral spinal anaesthesia, whereas those in group B received bilateral spinal anaesthesia.
All patients received Ringer’s lactate infusion 10 mL kg-1 before performance of subarachnoid blockade. Baseline heart rate (HR), systolic blood pressure (SBP), diastolic blood pressure (DBP), mean arterial pressure (MAP) and oxygen saturation (SpO2) were recorded. Patients were placed in a lateral decubitus position keeping the operated side dependent. Dural puncture was performed using a 25-gauge Quincke needle at L3–L4 or L4–L5 interspace under strict aseptic conditions. Correct needle placement was identified by free flow of cerebrospinal fluid. The bevelled end of the needle was pointed towards the operated side. 0.5% hyperbaric bupivacaine (Rupivac Heavy, Rusan Pharma Ltd, India) 7.5 mg (1.5 mL) and fentanyl (Fenstud, Rusan Pharma Ltd, India) 25 µg (0.5 mL) were injected intrathecally over 30 seconds. In group U, the lateral decubitus position was maintained for 15 minutes and then the patient was turned to the supine position. In group B, the patient was placed in a supine position immediately after the intrathecal injection. The operating table was maintained in a neutral position in both the groups.
HR, SBP, DBP, MAP and SpO2 were recorded at 3-minute interval for the first 15 minutes and then at 5-minute interval until the end of the surgery. If blood pressure decreased by more than 25% of the baseline value, the patient was considered to have developed hypotension and was managed with mephentermine 3 mg intravenously (i.v.). Bradycardia, defined as heart rate less than 50 min-1, was treated with iv atropine 0.6 mg i.v. The Visual Analogue Scale (VAS) score was recorded immediately after intrathecal drug administration and then at 15-minute intervals intraoperatively.
Motor blockade was assessed with the Bromage score as used in a previous study (1 – free movement of legs and feet, 2 – just able to flex knee with free movement of the foot, 3 – unable to flex knee, but with free movement of the foot, 4 – unable to move leg or foot) [4]. The height of sensory block was evaluated by the pin prick method using a 20-G hypodermic needle. The test was performed every 3 minutes for the first 15 minutes. The forehead was used as the baseline point for normal sensation.
At the end of surgery, the patient was shifted to the post-anaesthesia recovery room. HR, SBP, DBP, MAP, SpO2, Bromage score, height of sensory block and VAS were recorded at 30-minute intervals until the full recovery of the motor block. Any untoward side effect was also noted.
A difference in the MAP between the two groups following intrathecal drug administration was considered as the primary outcome variable. The secondary outcome variables included differences in HR, SBP, DBP, Bromage score and height of sensory block between the two groups.
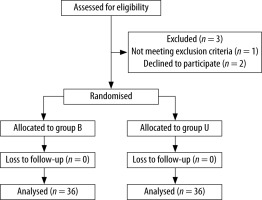
Sample size calculation: It was estimated that 36 patients per group (n = 36) were required to detect a 10 mm Hg difference in MAP between groups with a power of 80% and 5% probability of type 1 error. The calculation assumes a within-group standard deviation of 15 mm Hg. So, the total number of patients required was 72.
Statistical analyses
The statistical software IBM SPSS version 20.0 was used for the statistical analyses. Continuous variables were presented as mean ±SD. Categorical data were presented as number (%). Data distribution was first evaluated using the Kolmogorov-Smirnov test. Categorical variables were compared using Pearson’s χ2 test/Fisher’s exact test as appropriate. Parametric data were compared using unpaired Student’s t test. The Mann-Whitney U test was used for comparison of nonparametric data. A P value of < 0.05 was considered statistically significant.
RESULTS
In total 75 patients were screened for eligibility. Three patients were excluded; 1 of them did not meet the inclusion criteria and 2 patients refused to participate in the study. Finally 72 patients were randomly allocated to the study groups (Figure 1).
The two groups were comparable in terms of demographic profile, operated side, site of intrathecal drug administration and the duration of surgery (Table 1). There was no significant difference in baseline heart rate, SBP, DBP and MAP between the two groups.
TABLE 1
Comparison of demographic profile, operated side, site of intrathecal drug administration and duration of surgery
The SBP, DBP and MAP were significantly lower in group B compared to group U (P < 0.05) at 3, 6, 9, 12, 15, 30, 45, 60 minutes intraoperatively (Table 2).Table 3 shows that the mephentermine requirement was significantly higher (P < 0.001) in group B compared to group U.
TABLE 2
Comparison of intraoperative mean arterial pressure between groups
TABLE 3
Comparison of mephentermine requirement between groups
| Parameter | Group B | Group U | P value |
|---|---|---|---|
| Mephentermine required (yes : no), n | 36 : 0 | 22 : 14 | < 0.001 |
| Amount of mephentermine used in mg | 16.25 ±4.44 | 8.45 ±4.40 | < 0.001 |
There was no statistically significant difference in HR between the two groups both intraoperatively and postoperatively (P > 0.05). Two groups were comparable in terms of postoperative SBP. In comparison to group U, DBP and MAP were significantly lower (P < 0.05) in group B at 0, 30 and 60 minutes postoperatively (Table 4).
TABLE 4
Comparison of post-operative mean arterial pressure between groups
Immediately after intrathecal drug administration, Bromage score on the operated side was 4.00 ±0.00 in group B vs. 3.97 ±0.17 in group U, P = 0.317. Three minutes after intrathecal drug administration, all patients in both the groups attained a Bromage score of 4 on the operated side (4.00 ±0.00 in group B vs. 4.00 ±0.00 in group U, P = 1.000). Therefore, there was no statistically significant difference in the Bromage score on the operated side between the two groups intraoperatively.
However, on the non-operated side, the Bromage score was significantly higher in group B compared to group U. Immediately after intrathecal drug administration, the Bromage score was 4.00 ±0.00 in group B vs. 3.69 ±0.47 in group U, P < 0.001. At 3, 6, 9, 12 and 15 minutes following intrathecal drug administration, the Bromage score was 4.00 ±0.00 in group B vs. 3.75 ±0.44 in group U, P = 0.001.
In the postoperative period, Table 5 shows that the Bromage score on the operated side was significantly higher in group U at 30, 60, 90 and 120 minutes. Conversely, the Bromage score on the non-operated side was significantly higher in group B compared to group U.
TABLE 5
Comparison of postoperative Bromage score between groups
Table 6 shows that, 15 minutes following intrathecal drug administration, both the groups attained comparable sensory block height on the operated side. Conversely, the sensory block height was significantly higher in group B compared to group U on the non-operated side (P = 0.001).
TABLE 6
Sensory block height 15 minutes following intrathecal drug administration
On the operated side, there was no significant difference in the number of patients reaching the T10 sensory block height between the two groups (34 patients in group B vs. 36 patients in group U, P > 0.05). However, on the non-operated side, significantly fewer patients reached the T10 sensory block height in group U compared to group B (34 patients in group B vs. 14 patients in group U, P < 0.001). There was no significant difference in the intraoperative and postoperative VAS score between the two groups (P > 0.05). There was no adverse outcome in either group.
DISCUSSION
Age-related physiological changes play an important role in the clinical features of the subarachnoid blockade in geriatric patients. Following spinal anaesthesia, the block height is usually 3–4 segments higher in elderly patients compared to that in young adults [7]. Decreased cerebrospinal fluid (CSF) volume, nervous system degeneration and anatomic changes in the thoracic and lumbar spine are the main contributing factors [1, 8]. Old age and high sensory block height are two important factors for development of post-spinal hypotension in geriatric patients [9]. The incidence of hypotension following subarachnoid blockade in this population is about 25–69% [9].
It has been found that when a lower dose (5–8 mg) of local anaesthetic is used, placing the patient in the lateral decubitus position for 10–15 minutes can establish successful unilateral spinal anaesthesia. The drug can migrate towards the opposite side with the use of a higher dose of local anaesthetic even if the patient is placed in a lateral position for 30 minutes [4]. Therefore, in this study, 7.5 mg hyperbaric bupivacaine was used and the patients were placed in a lateral decubitus position for 15 minutes.
A slower injection rate generates a laminar flow which reduces the mixing of local anaesthetic agent with the CSF and thereby facilitates unilateral distribution of spinal blockade [10]. The success rate of unilateral blockade is higher when intrathecal injection is performed keeping the patient in a lateral decubitus position compared to the sitting position [11]. Therefore, with the patient placed in a lateral decubitus position, the anaesthetic was injected slowly.
The patients receiving unilateral spinal anaesthesia developed less hypotension both intraoperatively and postoperatively. Similar results were found in previous studies [3, 4, 6, 10]. Esmaoglu et al. [12] observed that no patient from the unilateral group developed hypotension. By limiting the sympathetic blockade to one side and sparing the contralateral sympathetic chain, unilateral spinal anaesthesia limits the marked fall in blood pressure. The factor which contributes to that is the distance between the left and right nerve roots in the lumbar and thoracic regions. The distance between the nerve roots is about 10–15 cm, which facilitates unilateral blockade [13].
Mephentermine requirement was also significantly higher in patients receiving bilateral spinal anaesthesia. Previous studies also obtained similar results [6, 14]. The requirement of a higher dose of vasopressors in patients with bilateral spinal anaesthesia is attributed to a higher degree of sympathetic blockade, which results in more profound hypotension.
There was no significant difference in the Bromage score measured intraoperatively on the operated side. A previous study conducted by Tekye et al. [4] found that the onset of motor block was faster in the bilateral group compared to the unilateral group. It may be explained by the use of a higher dose of bupivacaine (12.5 mg) in their study. The Bromage score on the operated side was significantly higher in group U compared to group B at 30, 60, 90 and 120 minutes postoperatively. Similar results were also obtained in previous studies [5, 6].
We also observed that the Bromage score on the non-operated side was significantly higher in group B compared to group U intraoperatively as well as postoperatively (Table 5). In group B, bilateral distribution of the drug produces blockade of nerve roots bilaterally and provides motor block of both operated and non-operated limbs.
On the operated side, there was no significant difference in the sensory block height between the groups. However, on the non-operated side, the sensory block height and the number of patients reaching T10 sensory block were significantly higher in group B compared to group U. A higher level of sensory block on the operated side is desirable for effective analgesia. However, a higher level of sensory block on the non-operated side does not provide any added advantage in the perioperative period. Moreover, the blockade of sympathetic outflow tracts occurs due to cephalic spread of the local anaesthetic and the resultant cardiovascular effects are proportional to the height of the block. Thus, in group B, the incidence of hypotension was higher due to higher sensory blockade on the non-operated side.
Therefore, unilateral spinal anaesthesia provided good operating conditions with adequate motor and sensory block on the operated side. It also led to avoidance of unnecessary blockade of the non-operated limb. At the same time, it produced less hypotension by sparing the contralateral sympathetic supply.
The limitations of this study include the lack of blinding and non-availability of various invasive and non-invasive methods of haemodynamic monitoring.
In future, similar studies can be conducted on different age groups of patients, undergoing different surgical procedures, using different drug doses and different adjuvants.