Introduction
Stress is an integral part of life of every human being. It affects us almost every day, and in different life situations. Although from the point of view of evolution, stress as a reaction to danger is undoubtedly an adaptive benefit, yet assessing it from a different perspective, stress is associated with numerous diseases, involving first of all reduced immunity. For this reason the World Health Organization defines stress as the disease of the century.
In the context of physiology, stress may be defined as a state of general body mobilisation in the face of strong physical or mental stimulus, whose prolonged interference with the homoeostasis may lead to impairment of numerous physiological processes. In the context of psychology, stress is seen as a special relation between a person and the environment, where the person perceives the situation as weakening their resources and posing a threat to their welfare, and where the situation is considered stress-inducing by the person involved, not by objective factors [1]. Therefore, psychological stress is in a sense a challenge testing individual possibilities and adaptation abilities of the organism.
According to the author of the stress theory, Hans Selye, stress may be both constructive and destructive. This means that not every type of stress is harmful toperson. In certain situations, it may show positive effects in the form of mobilisation to more effective performance. Positive stress is called eustress, and negative, harmful stress is called distress. Selye was the first scientist to notice that patients with different diseases reported similar complaints. He also first came up with the hypothesis that the underlying cause of numerous somatic diseases is the inability of the organism to cope with stress. He defined this phenomenon as insufficiency, a so-called general adaptation syndrome (GAS) [2]. Currently it is assumed that stress means organic, metabolic, physiological and neuropsychological disorders caused by stress-inducing factors - stressors [3], and that a reaction to these factors - a stress reaction - is a psychophysiological reaction [4]. Stressors endanger the stability of the body internal environment (homoeostasis), and a physiological response to the activity of these factors is adaptive in nature and is directed either to maintenance or to restoration of the homoeostasis impaired by the stressor activity [5].
Stress factors and mechanisms of the stress reaction
Stress factors have a complex nature. In the simplest terms, they are physical or psychological (psycho-emotional) signals. Recognition of the ascending information, which acts as a stressor, depends not only of its objective importance, but also on the assessment made by the organism itself. In the case of physical stressors, the objective assessment does not much vary from the subjective one. This is different in the case of psychological stressors, where their diagnosis and qualification highly depends on previous experiences, cognitive schemes or emotional attitude [6]. Adaptation to stress-inducing conditions is a dynamic process, coordinated by structures of the nervous system [7], and the organism’s response to stress induces neuroimmunohormonal changes.
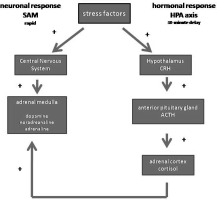
All stressors, both physical and psychological ones, activate the hypothalamic-pituitary-adrenal (HPA) axis, leading to a pronounced increase in the adrenocortical hormones in the peripheral blood. HPA, also called a stress axis, is activated with about a 30-minute delay, but its effects are long-lasting. Its role is related to control the course of the entire stress reaction and to determine the moment when it should end (Fig.1). The adrenocortical hormones, known as glucocorticoids, are steroid molecules produced and released by the arenal cortex. Cortisol, the major glucocorticoid in humans, is secreted at an approximately 10% lower rate in women as compared to man. The activity of the HPA axis components is closely related to the body’s stress response and is an integral part of the physiological mechanism of a stress reaction. A part of this reaction is also adrenocorticotropic hormone (ACTH) secretion from the anterior pituitary gland, stimulated by activation of perikaryons in the hypothalamic paraventricular nucleus (PVN). In the PVN, two hormones are secreted: corticotropin-releasing hormone (CRH) and arginine vasopressin (AVP), which control secretion of ACTH. ACTH, released to the bloodstream, stimulates the adrenocortical cells to release glucocorticoids, which by means of the negative feedback action inhibit the release of ACTH and CRH [8] via interactions with receptors located in the hippocampus, hypothalamus and pituitary gland. Synergistic action of AVP and CRH in the regulation of the HPA axis activity confirm once more the AVP involvement in the regulation of mood and anxiety behaviour [9].
The other important hormonal system involved in a stress reaction is the sympathetic-adrenal medullary (SAM) axis, identified with “fight or flight reaction”. SAM is activated already in the first minute of the stress reaction (Fig.1). It aims at rapid body response leading to solution of the stress situation [10]. Activation of this axis by stimulating the locus coeruleus in the brainstem and centres of the sympathetic nervous system, leads to an increased secretion of biogenic amines, such as adrenaline and noradrenaline, by adrenal medullary cells. Noradrenaline is also released by postganglionic sympathetic neurons. The activity of catecholamines is manifested e.g. by increased heart rate and respiratory rate, dilation of vascular walls of skeletal muscles, constriction of skin and gastrointestinal vessels, which leads to a better blood supply to the brain and muscles. An increase in the blood glucose level preceded by potentiation of the glycogenolysis process in the liver enables use of this sugar as a source of energy in defence mechanisms in situations of danger caused by a stressor [11].
Neurohormonal factors involved in the stress reaction also include systems of neurotransmitters such as dopamine, a member of the catecholamines, and serotonin. Dopamine, especially the mesocortical dopaminergic pathway, plays an important role in the processes related to emotion, selection of information and learning, on which counteracting stress is much dependent [12]. Serotonin (mainly serotoninergic system of the raphe nuclei of brain stem) participates in the mechanism of inducing anticipatory anxiety [13]. The role of this neurotransmitter is also associated with the occurrence of phobia and general anxiety disorders [14], and excessive stimulation of the serotonergic system may result in depression [15].
In addition to the above-mentioned factors, endogenous opioid peptides (EOP) are also involved in the response to stress. EOP (endorphins, enkephalins and dynorphins) influence the activity of immune cells [16]. The immune cells, in turn, may secrete endorphins at the site of anti-inflammatory process, which eliminates the state of pain stimulation invoked by the activity of proinflammatory factors [17].
Furthermore, CRH neurons located outside the hypothalamus (e.g. in the frontal cortex, central nucleus of the amygdalae, nucleus accumbens, grey matter, locus coeruleus, raphe nuclei, and cingulate cortex) participates in the activation of processes related to anxiety behaviour [3]. How strong body mobilisation is caused by stress is shown by the fact that in the course of the stress reaction there occurs release of somatotropin, prolactin, vasopressin and hormones of thyroid axis.
Psychoneuroimmunoendocrinology of stress
The HPA axis and the activation of the sympathetic nervous system are responsible for the relationship between stressful events and human immunity. The existence of mutual correlations between the CNS and immune system was first proven in early animal experiments, which showed that immunosuppression may be induced by classic conditioning [18]. The adaptive response to physical and psychological stressors includes modulation of not only two, but three regulatory systems, i.e. nervous, hormonal and immune system (Fig. 2). Normal communication between these systems is necessary to maintain homoeostasis and to guarantee human health and survival. The functional connection between nervous system, and endocrine and immune systems are currently obvious and relatively well-documented [19,20].
The mutual communication between these systems is the objective of research in the field of psychoneuroimmunoendocrinology. It is based on the ability of immune cells to detect and react to non-cognitive stimuli (antigens) and to inform the neuroendocrine system of such events. On the other hand, the neuroendocrine system identifies cognitive stimuli (e.g. stress, light, sound), reacts to them and transmits the information to the immune cells [21]. The cooperation of these three regulatory systems is possible because each of them includes receptors for specific mediators of other systems (neurotransmitters, hormones and cytokines) and because of the co-existence of particular system mediators in the nervous tissue, endocrine system and lymphoid organs. This communication ensures maintenance of homoeostasis, and, as a result, of physical and mental health [22,23]. Considering a complex nature of the neuroimmune-endocrine communication, any stimuli affecting the nervous and hormonal systems have also an effect on the immune system, and vice versa. Thereby, negative stimuli, such as emotional stress, anxiety or depression, impair immune functions by interfering with mutual interactions in the neuroimmune-endocrine network, leading to physiological disorders.
Literature data provide evidence that immune cells express receptors not only for cytokines, but also for neurotransmitters. The presence of sympathetic nerve endings: cholinergic, noradrenergic and peptidergic, which, by releasing neurotransmitters (e.g. catecholamines, opioid peptides), participate in the regulation of immune functions, since the immune cells contain receptors specific thereto. Endorphins, for example, stimulate production of immune cells in the bone marrow, and their maturation in the thymus gland. In addition, it has been proven that leukocytes express receptors for some hormones and neuropeptides. A classic example of correlations between these systems is the stimulation of ACTH secretion, which, in turn, increases secretion of glucocorticoids -factors responsible for immunosuppressing, inhibiting multiplication of leukocytes and synthesis of cytokines or mediators of the inflammatory process (Fig. 3).
Furthermore, the immune organs: thymus gland, bone marrow, spleen and lymph nodes are innervated, which enables them to receive signals from the nervous system [24]. The nervous system is under a constant influence of cytokines, e.g. interferon alpha (IFN-alfa) (Fig. 3). It has been demonstrated that high doses of this antiviral and anticancer protein cause negative side effects -concentration disorders, reduced physical activity, reduced sense of pain or even mental disorders [25]. It is also known that people with anxiety disorders are characterised by reduced performance of the immune system. A relationship between the nervous and immune systems may also be indicated by the fact that damage to the hypothalamus results in the significant changes in the cell-mediated immunity. The way of functioning of the immune system may undoubtedly undergo changes as a result of stress and emotional tensions. Hans Selye already noticed that experimental induction of stress conditions causes thymus involution and reduction in the number of immune cells. Many years latter it was documented that susceptibility to viral diseases is modulated by the type of stressful stimulus. It was also proven the influence of experienced emotions on the development of infectious diseases [26].
The response to stress may differ significantly depending on the age, sex, physiological condition, type of stressor, its intensity and duration. One of the most important factor is time of exposure to stressors. Therefore, the established taxonomy classifies stressors with regard to its duration [27]. This classification involves five categories of stressors: 1) acute time-limited stressors, which refers to the challenge punctuality, e.g. public speaking, such as scientific reports or lectures; 2) brief naturalistic stressors, including stress experienced by a person confronting a short-term challenge, such as an academic examination; 3) stressful event sequences, which refer to focal events resulting from a series of related challenges (e.g. a major natural disaster); 4) chronic stressors, which force a person to restructure his or her identity or social roles and are also characterised by certain stability and also uncertainty – whether the challenge will ever end (e.g. a person providing care for a relative with dementia); 5) distant stressors, including stress-inducing situations that occurred in the past, but yet affecting the person (e.g. traumatic experiences from childhood, such as sexual assault).
Neuroimmunoendocrinological studies provide evidence that mental and physical stressors may have a two-sided impact on the organism, i.e. from one point of view they mobilise the body to action by enabling long-term effort; on the other hand, this increased effort may be the cause of so-called “adaptation diseases”. From this perspective, health decline may be treated as the result of depletion of immune resources used in the process of long-term handling of stress. The conclusion is clear - while stressful events contribute to the development of diseases, the diseases and its consequences are a source of psychological stress.
Psychological stress may be defined as an environmental threat which does not necessarily induce a physical response in the form of “fight or flight”, but triggers a typical psychological reaction and physiological modifications instead. Regardless of the nature of reaction to stress (active or passive), the ability to respond to stress events and adapt to stress-inducing conditions is highly important in the context of health, including fertility. However, although reaction to stress is essential for life, failure to cope with stress may result in psychological and physiological responses which, although possibly adaptive, are insufficient or inadequate [19]. In this context, a complex intercommunication between the three regulatory systems is impaired, and the resulting loss of homoeostasis may cause unfavourable health effects.
From a physiological perspective, chronic stress involves the following: an increase in blood pressure leading to hypertension, a drastic decline in the calcium and magnesium levels, cardiac arrhythmias caused by long-term secretion of noradrenaline and adrenaline, fluctuations of the blood sugar level, excessive insulin secretion leading to cellular insulin resistance, constantly increasing blood level of free fatty acids leading to acidification, erosions and mucosal ulcerations, appetite dysregulation - compulsive eating or lack of appetite, premature ageing of skin and internal organs [28,29]. The list of diseases caused by stress is long, and a growing number of scientific evidence shows that the majority of so-called civilisation diseases is likely to be rooted in stress. Cardiac and cardiovascular diseases are the largest group (Fig. 4). The results of some studies indicate that people affected by stress are more predisposed to certain neoplasms. Moreover, stress often triggers or aggravates symptoms of autoimmune diseases, e.g. Hashimoto’s disease, rheumatoid arthritis (RA), diabetes mellitus type 1, and also ulcerative colitis. From a psychological perspective, chronic stress may cause: anxiety reactions, depression conditions, neuroses and affective diseases, aggressive behaviour, flight reactions [28]. A prolonged stress may induce exhaustion of the body and its immune and hormonal reserves, thus suppressing the neurotransmitters activity. Due to glandular fatigue, further secretion of cortisol becomes impossible, so there are insufficient amounts of fuel for the cells [30]. Discussing negative health impacts of stress, one must also mention the chronic fatigue syndrome (CFS). While the disease aetiology is not yet fully understood, its clinical symptoms (excessive fatigue, sleep disorders, sore throat, headache, joint and muscle pain, enlarged lymph nodes, circadian rhythm disorders, cognitive impairment and co-existing depression) are increased under stress conditions [31].
Stress also affects fertility, and mental balance is very important for the normal function of the reproductive system. Stress and fatigue may underlie the various sexual disorders. For example, stress hormones (CRH, cortisol) cause a reduction in the biosynthesis of a luteinising hormone (LH) and testosterone. Changes in the concentration of these hormones lead to spermatogenesis disorders, and, in turn, to a reduction in the sperm quantity and quality [4,32]. Intense negative emotions also affect a female reproductive system [33]. Early studies documented that girls living in chronic stress reached sexual maturation much later, and then they revealed irregular ovulation cycles. As mothers, they delivered weaker babies with significantly higher mortality rate [34]. Additionally, stress experienced in the course of pregnancy has a negative effect on foetal development and future cognitive abilities of the child. Chronic stress in pregnant women may result in a low birth weight of the new-born and in a number of disorders related to abnormal development of the nervous system [35,36].
The way stress affects immunity is known to be a complex process which largely depends on the duration of the stressful stimulus. It is assumed that short exposure to stress stimulates the immune response, while prolonged exposure inhibits the response [37]. For example, brief naturalistic stressors, such as exams, show a tendency to suppress cell-mediated immunity, at the same time maintaining full physiological status of humoral immunity. The activity of chronic stressors is related to the reduction of both types of immunity: cell-mediated and humoral [38]. In this context, the correlation between the brief stress and stimulation of the immune function may be seen as an adaptive feature. On the other hand, however, chronic exposure to stress seems to have a harmful effect on immunity, due to constant activation of the same mechanisms [39]. The explanation of these regulatory processes differing in response to stress may be related to different, glucocorticoid-dependent, mechanisms of cell signalling induced by these hormones under the conditions of short-term and prolonged stress [37]. It must be emphasised that glucocorticoids are neither the only ones nor basic factors inducing changes in the immune system during chronic stress [40]. For example, in animals, suppression of lymphocyte response to mitogen depends only on the β-endorphin level, and does not involve corticosterone activity [41]. Similarly, lymphocyte apoptosis during stress is induced by opioids [42]. On the other hand, the adrenergic receptor (β2-AR), after binding catecholamines, triggers DNA damage via two different signalling pathways [43]. Simplifying, acute stressors strengthen the internal ability of the immune system to act quickly [44], usually excluding the function of natural killer (NK) cells [45] and production of neutrophil peroxide [46]. The effect of chronic stressors, however, is related to global immunosuppression, and such effect of their activity is related to the mechanisms of both innate and acquired immunity [47,48].
Results of numerous studies have documented that chronic stress is accompanied by behavioural changes, including alcohol consumption [49], smoking tobacco products [50], bad eating habits [51], or sleep disorders [39]. All these situations may result in serious health consequences. Similarly, a change in the social role and social support related to stress also has a negative effect on the health and quality of life [52]. Reports on AIDS very well fit in this notion, highly emphasising the effect of psychological factors on the development of this disease. Rapid progress of AIDS is primarily related to accumulation of difficult events underling with stress. The negative experiences may cause dysregulation of the immune system and, in consequence, multiplication of HIV which was latent up to that point [53].
Other studies, exploring correlations between psychological stress and immune system, analysed the effect of highly stressful events, e.g. mourning after sudden death of a loved one, depression and significant life losses with regard to their impact on the immune response. For example, mourning impairs the neutrophil function and causes reduction in the lymphocyte production [54]. Solitude is associated with a reduced activity of NK cells. The same applies to the depression and anxiety, which also involve an increase in the lymphocyte level [55]. The following also have important consequences for somatic health: professional burnout, loss of job or staying in an unfavourable social environment [26]. The same refers to people for whom their illness is an obstacle in the implementation of an important plan or professional activity [55]. The specific reactions of the immune system to positive events were also demonstrated; social support causes an increase in the lymphocyte count and in the activity of NK cells; laughter generates more active lymphocytes; relaxation activates T lymphocytes and NK cells and reduces the level of cortisol and herpes virus in the blood; aerobics increases the level of white blood cells, NK cells, and activates opioid receptors by an increase in endorphins [55].
It is generally accepted that taking care of a chronically ill person exerts a strong influence on the mental well-being and physical health of the carer [56]. For example, parents of small children suffering from cancer showed a reduced sensitivity to the anti-inflammatory effect of glucocorticoids, which may potentially contribute to development of asthma, autoimmune diseases and cardiovascular diseases, and lead to dysregulation of the immune system and serious infections [57].
It is known that vaccination generates immune memory directed against specific pathogens, and prepares the body for a response to real infection. The measurement of post-vaccination protection is the titre of specific antibodies. Elderly and lonely persons, and persons whose marriage quality was poor revealed lower post-vaccination immunity against flu than people living in happy relationships [47]. Stressful life events or situations perceived as stress, were associated with a lower level of antibodies produced in response to vaccination against flu and meningitis in students [58,59], while higher social support increased the titre of antibodies to some vaccine strains [59]. Parents taking care of children with developmental disability showed a much lower titre of antibodies against pneumococci, as compared to control group. Similarly, parents taking care of ill children did not reach equally high post-vaccination immunity against flu as the parents from the control group [60].
Stress also affects significantly the processes of DNA repair. Studies indicating existence of correlations between stress and DNA repair processes [61] suggest at the same time a complex relationship between stress and defence mechanisms of the body. In young and healthy students of medicine exposed to UV radiation, stress related to the exam period caused an increase in the range of DNA repair [62]. This phenomenon was also confirmed in other study who revealed an increased rate of DNA repair in students during the exam period, as compared to the holiday period [63].
From homeostatic perspective, another important mechanism is the programmed cell death, i.e. apoptosis. Apoptosis is a physiological processes that is necessary for the normal functioning of the immune system, since it guarantees maintaining homoeostasis under conditions involving activity of various physiological and pathological stimulus [64]. Therefore, it is not surprising that unfavourable conditions of the external and internal environment impair the balance of apoptotic processes.
Another observation confirming the negative effect of stress and emotion on the immune system is the fact that in the event of an epidemic, people in a good mood and mental state less frequently fall down with illness and suffer less from it. This fact becomes especially important in the face of coronavirus pandemic, which affects not only physical health of humans, but also their mental sphere. Many people experience stress, anxiety, and even depression. The SARS-COV-2 pandemic, despite almost three-year history, still raises many doubts and questions, but most of all -what immunity the infection gives, and how long it is maintained? It is known, however, that patients suffering from COVID-19 reveal striking immune dysregulation leading to higher morbidity and mortality. For example, subjects suffering from coronavirus revealed a reduced number of T, B, and NK cells and an increased level of proinflammatory cytokines. They had an increased level of white blood cells and neutrophil count. Moreover, the number of T lymphocytes, NK cells and B lymphocytes was lower in patients with severe course of the disease [65], as compared to a mild course. Patients with a long course of COVID-19 had highly activated mechanisms of innate immunity, and showed an increased expression of IFN type I (IFN-β) and type III (IFN-λ1), which was maintained at a high level even 8 months after infection [66]. It was also found that subjects with an immune system dysfunction were more susceptible to breakthrough infection, regardless of the vaccination status, as well as to serious consequences of COVID-19 [67]. There are more and more serious concerns regarding negative effects of the infection on the human reproductive function [68– 70]. However, the ultimate effect of the coronavirus infection on female and male fertility requires long-term observation.
In the times when stress is omnipresent and constitutes a serious social problem, it is highly needed that negative effects of stress be counteracted, and effective methods of coping with negative emotions be developed for the purpose of improvement in the quality of life. That is why one should have healthy sleep, good relations with others, and should find time for such activities that would ensure physical activity and relaxation. A very interesting and effective, non-invasive method used in the treatment of various diseases is biofeedback. Biofeedback is an innovative therapeutic method which has an effect on many various complaints. It is based on the assumption that man may consciously affect the state of one’s body and its physiological processes. Biofeedback is a method using the latest discoveries in the field of medicine and computer science. The biofeedback training may enable the patient to learn to control some, normally involuntary, processes, which in turn enables them to fight symptoms of certain diseases.It may also promote improvement in concentration, and achieving higher performance at work and study with a reduced energy output. The therapy also results in a reduced level of stress and anxiety, improved social relations, and higher self-assessment. It also enables the patient to modify certain behaviours, teaches control over reactions and emotions, which in turn translates into a better control of body and mind. Biofeedback is a fully recognised method, confirmed with scientific studies, which in many people gives better results than pharmacotherapy.
Studies conducted over many years, exploring relationships and cooperation of the nervous, hormonal and immune systems, gave basis to concomitant consideration of two health dimensions - mental and somatic. A close connection of the nervous system with the endocrine system and immune system causes that long-term mental tensions induce neuroendocrine changes that in turn affect immunity. It must be emphasised, however, that in this network of mutual correlations of the nervous/hormonal/immune systems during stress, the interaction is multidirectional, but a full explanation of mechanism that control them remains in the sphere of scientific speculations and requires further studies exploring this complex relationships. Therefore, in the times when stress is omnipresent and constitutes a serious social problem, it is highly needed that negative effects of stress be counteracted, and effective methods of coping with negative emotions be developed for the purpose of improvement in the quality of life.

 POLSKI
POLSKI