Pityriasis rubra pilaris (PRP) is an uncommon clinically heterogeneous keratinization skin disorder. PRP occurs equally in men and women and has a bimodal age distribution with typical onset during the first and fifth decades [1]. Due to the significant clinical diversity, PRP is classified into six subgroups according to age of onset, distribution, morphologic features, clinical course and human immunodeficiency virus (HIV) infection [1, 2]. The aetiology of the disease remains unknown but several studies have reported its occurrence in the setting of viral infection, trauma, stress, associated autoimmune diseases, malignancies and drugs [3].
We present the case of a 7-year-old patient with type III PRP in which emotional stress appeared to be the most probable triggering factor.
A 7-year-old girl was referred to our institution for a diagnostic evaluation of skin lesions with a 3-month history. The skin lesions clinically appeared as generalised erythroderma. Locally, physical examination revealed diffuse pityriasiform scale of the scalp, confluent areas of erythema on the trunk (Figure 1 C) and follicular hyperkeratotic papules within erythematosquamous plaques with an orange hue distributed on the legs. Patches of normal skin were evident within those sheets of erythema (Figure 1 A). Waxy palmoplantar keratoderma with fissures was observed (Figure 1 B). Skin burning sensation and itching accompanied skin lesions. The patient’s past medical history was notable only for mild xerosis cutis. A review of systems was non-contributory. Family history of psoriasis and atopic diseases was negative. There were no similar previous episodes or recent exposure to drugs or infections. Four months before hospitalisation the patient began primary school. Her mother noted that in that time the patient developed anxiety, aggressiveness and social isolation due to rejection by friends in her class. She tended to refrain from social activities in the presence of peers. The first skin lesions in the form of scaly erythematous patches developed initially over the elbows and knees 4 weeks after the First Day of Class. Despite initial therapy with hydroxyzine and emollients prescribed by her primary care physician, the plaques spread throughout the patient’s face, scalp, torso and limbs. Her hands and feet developed an orange-red appearance with desquamation. She was referred to the Paediatric Dermatology Department where she was clinically diagnosed with generalised pustular psoriasis. Topical treatment with anthralin cream resulted in rapid deterioration of skin findings. At admission basic laboratory and microbiological examinations were performed. Laboratory investigations revealed mild eosinophilia (1000/μl) and a high serum immunoglobulin E level (1100 IU/ml). Lesional punch biopsy of affected skin documented alternating orthokeratosis and parakeratosis, an absence of Munro microabscesses, a low-grade superficial perivascular infiltration of lymphocytes and plugging of follicular infundibula by cornified cells (Figure 2). The image corresponded to the clinical diagnosis of classic juvenile type III PRP. The patient was treated with oral acitretin 10 mg daily (approximately 0.3 mg/kg), moisturizing creams, topical 10% urea ointment (hands and feet) and topical 5% salicylic acid ointment (scalp). The duration of acitretin therapy was 3 months. Within 2 months, the patient improved remarkably. The papules and plaques resolved completely with residual postinflammatory hyperpigmentation (Figure 3). The patient did not suffer from any adverse reactions to acitretin other than xerosis cutis.
Figure 1
A, B – Hyperkeratotic papules, patches of normal skin and erythematosquamous plaques with an orange hue distributed on the legs. C – Waxy palmoplantar keratoderma with fissures. D – Confluent areas of erythema covered with diffuse pityriasiform scale on the trunk

Figure 2
The biopsy shows alternating orthokeratosis and parakeratosis in a checkerboard pattern and plugging of follicular infundibula by cornified cells (H + E, magnification 100×)
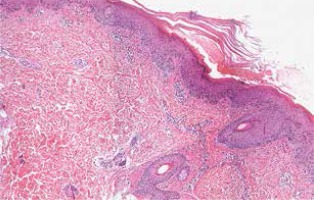
Figure 3
After 2 months the papules and plaques resolved completely with residual postinflammatory hyperpigmentation and xerosis cutis

The incidence of PRP in children is not precisely known, though in one study the disease has been estimated to be present in approximately 1/500 patients hospitalized in the Paediatric Unit with a skin disorder [4]. Type III (classical juvenile) represents approximately 10% of PRP with a median age of onset of 5–10 years [3]. Erythroderma can be one of the most remarkable clinical findings. In one retrospective series, 24% of children presenting type III PRP had erythroderma [5]. Other clinical features consist of hyperkeratotic follicular papules and plaques that coalesce with islands of sparing and orange-hued palmoplantar keratoderma. Maximum spread is typically within 3 months. Mucosal involvement is uncommon [6]. It is considered to be prognostically favourable with a spontaneous clearance within 1–2 years [3]. The recurrence rate is about 17% [5]. PRP is diagnosed clinically with skin biopsy findings being supportive but not pathognomic. Characteristic histological features consist of psoriasiform hyperplasia, alternating orthokeratosis and parakeratosis (checkerboard pattern), follicular plugging and scanty superficial perivascular infiltrate within the dermis. Unlike psoriasis, in PRP neutrophils are not present in the epidermis or stratum corneum [7, 8]. A detailed family and personal history should be obtained to help rule out common differential diagnosis such as psoriasis, atypical keratosis pilaris, phrynoderma, atopic dermatitis, ichthyoses, seborrheic dermatitis and palmoplantar keratoderma. There are no standard recommended treatment algorithms for PRP in paediatric patients. Based on few long-term studies on the treatment and prognosis, systemic retinoids are considered the first-line therapy [9, 10]. Treatment with acitretin at 0.3 mg/kg was highly effective in our patient. Within the last decade, several case reports have noted efficacy of biologic therapies initially approved to treat plaque psoriasis such as TNF inhibition [11, 12].
In conclusion, we herein present an unusual case report showing that in paediatric population emotional stress can be the isolated trigger for the occurrence of PRP. Further investigations are needed to identify the pathomechanism of antecedent psychological stress and onset of PRP.








