Introduction
Modern societies are facing a dynamic increase in the number of elderly people, which entails numerous health and social consequences. One of the key challenges is the increase of chronic diseases, requiring long-term treatment, systemic care, and comprehensive preventive measures. The multifactorial nature of these conditions, including both biological aspects (e.g., progressive degenerative changes in the circulatory system or the nervous system) and psychosocial aspects (including the need for emotional support and the prevention of social isolation), makes the study of their course and the development of effective methods of care for the elderly on of the most important tasks of contemporary medicine and nursing [1, 2, 3].
According to WHO data from 2019, chronic diseases were the leading cause of death in Poland and the main underlying factor in the loss of Disability-Adjusted Life Years (DALY). This indicator reflects both the number of premature deaths caused by a given disease and the years of life lived with disability, demonstrating the significant impact of chronic diseases on public health. These conditions not only increase mortality but also contribute to long-term limitations in the ability to function independently, often requiring prolonged therapy and rehabilitation [4, 5, 6]. Epidemiological studies indicate that chronic diseases affect a large part of the population, and their prevalence data increases with age. In 2019, around 39% of adult Polish people suffered from at least one chronic condition, meaning that nearly every second adult experienced long-term health problems. This percentage is even higher among older adults- up to 70%. of the population over the age of 65 suffers from one or more chronic diseases. Moreover, studies show that socioeconomic status has a significant impact on the risk of developing chronic diseases. Moreover, studies show that socioeconomic status has a significant impact on the risk of developing chronic diseases. According to a 2021 report by the Organization for Economic Co-operation and Development (OECD), individuals with lower incomes are more likely to suffer from these conditions, which may result from limited access to healthcare, poorer living conditions, and greater exposure to risk factors such as inadequate diet, physical inactivity, and chronic stress [1, 7]. Given the increasing number of people affected by chronic diseases, it is essential to implement effective preventive measures and improve access to healthcare [1, 8].
Aging is associated with numerous changes that can limit the functioning of older adults and reduce their quality of life. While some of these changes are physiological and result from the natural aging process, many are pathological and can lead to development of chronic diseases. Chronic diseases constitute a broad category of conditions, including approximately 150 disease entities. They are characterized by a long-lasting and often progressive course, and their treatment requires a systematic approach.
The most common chronic disease includes cardiovascular diseases (hypertension and heart failure), cerebrovascular diseases (stroke, atherosclerosis), and chronic respiratory diseases (chronic obstructive pulmonary disease (COPD), asthma). The group of chronic diseases also encompasses cancers, diabetes, rheumatoid arthritis, mental disorders, autoimmune diseases, epilepsy, osteoporosis, obesity, multiple sclerosis, and acquired immunodeficiency syndrome (AIDS) [7, 9].
Given the increasing number of people affected by chronic diseases, it is essential to implement effective preventive measures and improve access to healthcare, with particular emphasis on: i) health education- raising awareness about risk factors and methods of preventing chronic diseases, ii) primary prevention- promoting a healthy lifestyle, proper diet, and regular physical activity, iii) early disease detection- increasing the availability of screening and diagnostic tests, iv) improved access to treatment-developing therapeutic and rehabilitation programs, especially for seniors and at-risk populations, v) psychological and social support- providing patients and their families with comprehensive care and assistance in daily functioning.
Effective management of chronic diseases requires an integrated approach, in which physicians, nurses, physiotherapists, and psychologists play a key role. Interdisciplinary collaboration can significantly improve patients’ quality of life and reduce the negative health and social consequences associated with these conditions. Chronic diseases represent a major challenge for contemporary medicine and healthcare systems. Their high prevalence, particularly among older adults, and their impact on patients’ quality of life necessitate comprehensive measures in both treatment and prevention. Reducing the effects of chronic diseases requires not only appropriate medical programs but also extensive educational and social initiatives, which can contribute to improved population health and reduced burden on the healthcare system [10, 11, 12, 13].
The aim of this study was to highlight the important role of nurses in the care of seniors suffering from chronic diseases, in the context of both physiological and pathological age-related changes, as well as the characteristics of the most common conditions. Another key objective was to present issues related to long-term care, rehabilitation, patient education, and emotional and social support, which are essential components of comprehensive therapy. The study also aimed to gain a better understanding of the health needs of older adults and to formulate conclusions that could contribute to the improvement of nursing practice and systemic solutions in long-term care.
Material and methods
The study was conducted at the St. Anna Medical and Service Center in Płock from March 2025 to May 2025, during a period approved by the Bioethics Committee (approval no. KB/PIEL-II28.2025). The study group consisted of 60 elderly individuals- 44 women and 16 men- suffering from various chronic diseases. The largest age groups were 70-79 years (28 participants) and 8-89 years (16 participants). The remaining participants included 10 individuals aged 60-69 and 3 individuals over 90 years old. The inclusion criterion for participation was providing informed consent after being informed about the study’s purpose. Participants were given anonymous questionnaires covering issues related to nursing care and quality of life assessment in the course of chronic diseases.
The following tools were used in the study:
a self-designated questionnaire, including demographic data and questions concerning chronic diseases, patient functioning, and the quality of nursing care,
the ACDS (Adherence in Chronic Diseases Scale), used to assess patients’ adherence to therapeutic recommendations,
The WHOQOL-BREf questionnaire (World Health Organization Quality of Life – BREf), enabling the assessment of patients’ subjective quality of life in four main domains: physical health, psychological well-being, social relationships, and living environment.
The self-designated questionnaire consisted of closed and open-ended questions, divided into sections covering, among others, the type of chronic diseases, their duration, independence in daily functioning, frequency of disease exacerbations, and the subjective assessment of the quality of nursing care (Fig. 1-12).
The ACDS scale was used to determine the degree if patients’ adherence to medical recommendations. The use of this tool was important because effective nursing care in chronic diseases involves not only performing medical tasks but also supporting patients in following therapeutic guidelines. By assessing the level of adherence, it was possible to gain a better understanding of the extent to which patients engage in the treatment process, which directly affects health outcomes and quality of life.
The WHOQOL-BREf questionnaire allowed for the collection of data on patients’ overall quality of life, their physical and psychological well-being, social relationships, and environmental conditions. This provided a comprehensive view of the situation of older adults with chronic diseases.
All of the applied tools were selected to ensure a comprehensive assessment of the health status, adherence to therapeutic recommendations, and quality of life of elderly patients. Using the observation method, which involved systematic monitoring of patients’ functioning in their daily environment, the information obtained from the questionnaire was verified through direct observations of their health status and independence. This allowed for the selection of representative study population. Due to scientific evidence regarding the influence of ambient temperature on physiological processes and, consequently, the course of diseases, the study was conducted during the spring months (March-May). Day length also has significant health implications; during the autumn and winter periods, older adults are considerably less active. Increased infection rates and limited sunlight, which can negatively affect mood, could also disrupt the results of the study [14].
After collecting all completed forms, the data were processed and subjected to statistical analysis in order to interpret the results and formulate conclusions summarizing the findings of the study.
Statistical analysis
All data collected during the study were entered in real time into a specially prepared database in Microsoft Excel, developed for the purposes of this research. IBM SPSS Statistics version 28.0 was used to perform statistical analyses, enabling efficient processing of the collected results and testing of the research hypotheses.
The study was anonymous and voluntary. The collected data were subjected to descriptive, graphical, and statistical analysis to accurately characterize the study group and determine relationships between selected variables.
To assess relationships between qualitative variables, the chi-square (χ2) test of independence was used. The results were analysed at a significance level of 0,05 (p < 0,05). Accepting 5% risk of error allowed to the results to be considered statistically significant when the p-value was less than 0,05.
Obtained values were compared with the critical values in the chi-square table. If the calculated χ2 value exceeded the critical value for a given significance level, the relationship between the studied variables was considered statistically significant.
Results
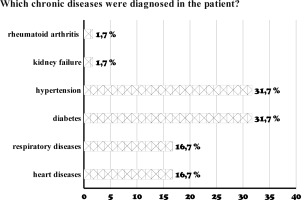
The most common chronic diseases among the studies patients were the hypertension (31,7% of patients) and diabetes (31,7% of patients). Other diagnosed conditions included respiratory diseases (16,7% of patients), heart diseases (16,7% of patients) and kidney failure (1,7% of patients), while rheumatoid arthritis (RA) was present among 1,7% of patients.
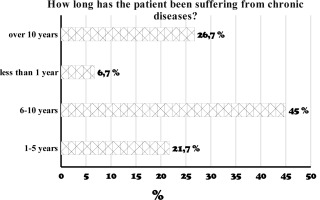
The largest group of patients has been suffering from chronic diseases for 6-10 years (45%), while 26,7% of patients have had their conditions for over 10 years. Between 1 and 5 years, 21,7% of patients have been affected, and the smallest group consists of those who have been ill for last than 1 year (6,7%).
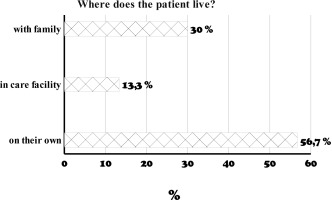
Over a half of the responders live independently (56,7%), 30% live with family and 13,3% reside in care facilities.
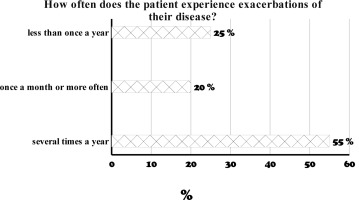
Exacerbations of chronic diseases occur several times a year in more than half of the patients (55%), while less that once a year in 25% of patients. In 20% of patients, exacerbations occur once a month or more frequently.
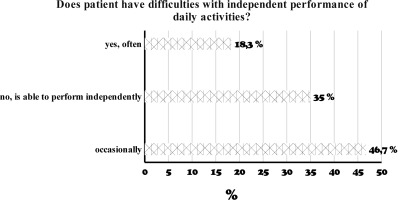
Approximately half of the patients sometimes have difficulty performing daily activities independently (46,7%). 35% of patients are fully independent in daily life, while 18,3% of respondents frequently experience problems with daily self-sufficiency.
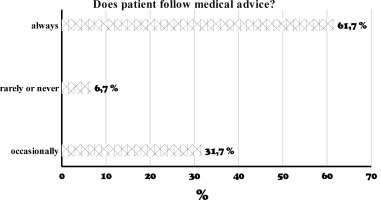
The majority of patients always follow medical recommendations (61,7%), while 31,7% adhere only occasionally. The group of patients who rarely or never follow medical advice constitutes 6,7% of patients.
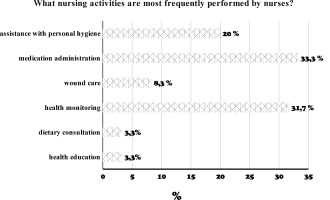
According to the patients, the most frequently performed nursing care activities are: medication administration (33,3%), health monitoring (31,7%), and assistance with personal hygiene (20%). Less frequently, nurses provide wound care (8,3%), dietary consultations (3,3%), or health education (3,3%).
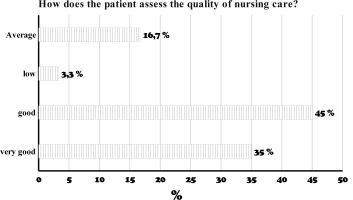
45% of patients assessed nursing care as good, while slightly fewer, 35% assessed it as very good. Nursing activities were assessed as average by 16,7% of patients and as poor as by 3,3% of the study population.
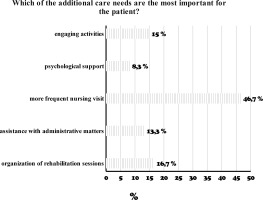
More frequent nursing visits were clearly the most desired by respondents (46.7%). The next most important needs were increased rehabilitation sessions for patients (16.7%) and, similarly, engaging activities (15%). The least reported needs were assistance with administrative matters (13.3%) and psychological support (8.3%).
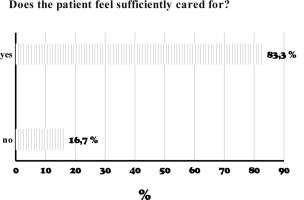
The vast majority of patients feel sufficiently cared for by the nursing staff (83,3%), while 16,7% expressed dissatisfaction with this care.
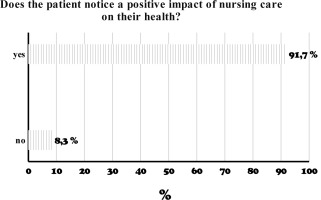
Almost all of the patients (91,7%) reported a positive impact of nursing care on their health, while only 8,3% of patients did not notice such an effect.
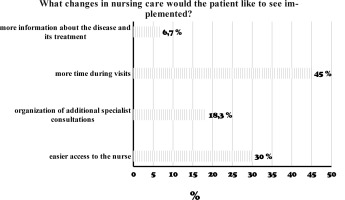
The majority of patients would definitely like nursing staff to spend more time with them during visits (45%) and to have easier access to the staff (30%). According to the patients, organizing additional specialist consultations (18,3%) or providing more information about their disease (6,7%) is less necessary.
Statistical analysis of results
The applied methods of data analysis enabled a reliable elaboration of the study findings (Fig. 1-12) and the assessment of relationships between selected variables. This allowed for drawing accurate conclusions regarding nursing care for elderly patients with chronic diseases.
Tab. 1.
The most frequently performed nursing care activities
The most frequent indicated nursing activity by patient was medication administration- this form of care was mentioned by 33,3% of patients (n=20). Slightly fewer, 31,7% of patients (n=19), pointed to health monitoring, which highlights the importance of medical supervision in the course of chronic disease.
Assistance with personal hygiene was provided according to 20,0% of patients (n=12), while wound care was indicated by 8,3% (n=5).
The least frequently indicated activities were health education and dietary consultation, each reported by 3,3% of patients (n=2). This may suggest that educational and dietary interventions are implemented less often or are less noticeable to patients.
Tab. 2.
Relationship between the duration of chronic diseases and the patient’s difficulties in performing daily activities.
Among patients who have been ill for less than a year, none reported difficulties in daily functioning- 100,0% answered “sometimes”, which may suggest a mild course of the disease or preserved independence at the early stage of treatment.
In the group of patients who have been ill for 1-5 years, the majority reported no difficulties and maintained independence (62,2%), while only 15,4% reported frequent or occasional difficulties.
The situation is different among patients who have been ill for 6-10 years- as many as 63,0% reported occasionally experiencing difficulties with daily activities, and 11,1% reported frequent difficulties. Only 25,9% considered themselves fully independent.
The most problems were observed among patients who have been ill for over 10 years- 37,5% re-ported frequent difficulties in performing daily activities, while only 31,3% considered themselves fully independent.
Pearson’s chi-square test showed a statistically significant relationship between the duration of chronic disease and the occurrence of difficulties in performing daily activities (χ2 =18,7; p=0,004). This indicates that the longer a patient has been ill, the more frequently they report difficulties in daily functioning.
Tab. 3.
Assessment of the quality of nursing care according to the patients’ level of education
The majority of patients with primary education rated nursing care as good (54,5%), while 31,8% of this group considered it very good, and a few patients rated it as low (4,5%) or average (9,1%).
Among patients with secondary education, the most frequent ratings were very good (42,9%) and good (38,1%), with none of this group assessing the care as low. An average quality rating was indicated by 19,0% of patients.
Patients with higher education rated the care exclusively as good (66,7%) or average (33,3%). There were no assessments of “very good” or “low”.
In case of patients with vocational education, the most frequent assessments were very good and good (35,7% each), while low (7,1%) and average (21,3%) assessments were also recorded.
Statistical analysis using Pearsons’ chi-square test showed that the differences in the assessment of nursing care quality were not statistically significant depending on the education level (χ2 = 5,76; p = 0,763). This means that patient’s education did not have a significant impact on how they evaluated the quality of nursing care they received.
Tab. 4.
Subjective assessment of nursing care in patient’s opinion
| How does the patient assess the quality of nursing care? | Frequency | Percent |
|---|---|---|
| Very good | 21 | 35,0 |
| Good | 27 | 45,0 |
| Low | 2 | 3,3 |
| Average | 10 | 16,7 |
| Total | 60 | 100,0 |
The majority of patients assessed the quality of nursing care as good, with 45,0% of patients (n=27) selecting this option. Very good care was reported by 35,0% of patients (n=21), giving a total of 80% positive evaluations.
Average nursing care was assessed by 16,7% patients (n=10), while a low rating was given in only 3,3% of cases (n=2).
Obtained results indicate that most patients view nursing care positively, although a small proportion points to areas that need improvement.
Tab. 5.
Patients’ suggestions for improving nursing care
The most commonly expressed need by patients was for nurses to spend more time with them during their visits, reported by 45,0% of patients (n=27). The second most frequent need was easier access to the nurse, indicated by 30,0% of patients (n=18).
The organization of additional specialist consultations was expected by 18,3% of patients (n=11), while the smallest proportion of patients- 6,7% (n=4)- indicated a need for more information about their disease and treatment.
The results suggest that patient primarily expect nursing care to be more accessible, calm, and individualized.
Tab. 6.
Patients’ quality of life assessment according to WHOQOL-BREF domains
| N | Minimum | Max | imum | Mean | SD | ||
|---|---|---|---|---|---|---|---|
| Domain 1: Physical health | 60 | 4,0 | 15,0 | 8,483 | 2,3106 | ||
| Domain 2: Psychological | 60 | 5,0 | 14,0 | 9,250 | 1,7910 | ||
| Domain 3: Social | relationships | 60 | 3,0 | 10,0 | 5,917 | 1,7004 | |
| Domain 4: Environment | 60 | 5,0 | 14,0 | 9,300 | 1,8983 | ||
In the study assessing the quality of life of elderly patients with chronic diseases, the WHOQOL-BREf questionnaire was used, allowing for an analysis of the subjective perception of various aspects of life. This tool evaluates four main domains: physical health, psychological well-being, social relationships, and living environment. The results presented below reflect the level of patient satisfaction in each of the assessed domains.
In the domain of physical health (Domain 1), the mean score was 8,48 points (SD=2,31), with a range of 4 to 15 points, indicating a moderate level of assessment in this area.
The psychological well-being (Domain 2) received the lower mean score- 5,92 points (SD=1,70), within a range of 3 to 10 points, which may indicate a relatively low subjective assessment of psychological well-being among the patients.
Social relationships (Domain 3) were rated with a mean score of 9,25 points (SD=1,79), with results ranging from 5 to 14 points, indicating a relatively high quality of life in this area.
Living environment (Domain 4) achieved a mean score of 9,30 points (SD=1,90), with a range of 5 to 14 points, which may suggest positive assessment of living conditions and surroundings.
The ACDS (The Adherence in Chronic Diseases Scale) is a tool used to measure the degree to which patients with chronic diseases follow therapeutic recommendations. This questionnaire focuses on assessing how patients adhere to daily treatment instructions, including various aspects such as the regularity of medication intake, compliance with recommended diets, and other health-related advice.
The interpretation of ACDS scale results is based on the total score obtained by the patient in the questionnaire. The scale consists of 7 questions, each with 5 possible answers scored from 0 to 4. The final score ranges from 0 to 28 points.
Interpretation:
• 27–28 points– high adherence
The patient follows therapeutic recommendations very well, takes medications regularly, and com-plies with the doctor’s instructions.
• 21–26 points– moderate adherence
The patient mostly follows the recommendations but occasionally missed doses or errors in therapy may occur.
• <21 points– low adherence
The patient frequently doesn’t follow the recommendations, which may affect treatment effectiveness and disease control.
Tab. 7.
Level of adherence to therapeutic recommendations according to the ACDS scale
| ACDS scale (The Adherence in Chronic Diseases Scale) | Frequency | Percent |
|---|---|---|
| low adherence | 12 | 20,0 |
| moderate adherence | 32 | 53,3 |
| high adherence | 16 | 26,7 |
| Total | 60 | 100,0 |
Among the patients, the largest group consisted of those demonstrating moderate adherence- 53,3% (n=32). A high level of adherence to therapeutic recommendations was observed in 26,7% of patients (n=16), while low adherence was reported in 20,0% of cases (n=12). These results indicate that most patients follow medical recommendations to some extent; however, only about one in four adheres optimally, where one in five requires particular attention due to a low level of adherence.
Discussion
The goal of the conducted study was to explore the nature of nursing care provided to elderly people with chronic diseases and to assess its impact on their quality of life and functional status. The gained results show that seniors have extensive nursing needs and require comprehensive care. Nursing activities are diverse and primarily focuses on the prevention of complications as well as ensuring patient safety and comfort. Data analysis revealed that the most frequently performed nursing activity was the administration of medications, followed by health monitoring and assistance with personal hygiene. Less frequently mentioned were wound care, health education, and dietary consultations. These findings are supported by observations of other authors, who emphasize that nursing interventions mainly concentrate on the prevention of complications and the improvement of patients’ quality of life [15, 16, 17, 18].
The present study demonstrated a statistically significant relationship between the duration of chronic diseases and difficulties in daily functioning. Patients with a shorter history of disease (up to 5 years) were more independent, where those with a disease duration of more than 10 years reported difficulties more frequently. This suggests that the progression of the disease affects the patient’s level of independence. The association between disease duration and self-sufficiency highlights the need to personalize medical support depending on the stage of the condition. Therefore, when planning nursing interventions, it seems essential to take into account not only the physical and psychological limitations of the older patient, but also their living environment, social support, and family involvement. Indeed, in light of the findings of the present study, an essential element of nursing care is the assessment of the patient’s independence and their ability to perform basic activities of daily living. Such an assessment, as noted by other authors as well, makes it possible to plan the scope of necessary assistance and to define therapeutic and rehabilitative goals [16, 17, 18]. Personalized support provided by nurses, addressing both the physical and emotional aspects of health, appears to be particularly important also in the context of palliative and long-term care. Therefore, specialized medical care, including nursing interventions, should promote new models of care consistent within the personal development and needs of elderly struggling with chronic diseases [17, 19, 20, 21].
In the present study, patients assessed the quality of care highly regardless of their educational background, which suggests its broad acceptance. The majority of patients assessed nursing care as good or very good, which together accounted for 80% of positive evaluations. Average or low ratings appeared only in a few cases. This indicated a high level of satisfaction with care, particularly when it is tailored to the individual needs of patients.
Despite relatively favourable assessments in terms of living environment and psychophysical condition, the low level of social relationships and the moderate adherence to medical recommendations reveal areas requiring further support and education. The obtained results are consistent with previous research [22] and highlight the need for continued efforts aimed at improving quality of life and the effectiveness of nursing care in this group of patients [23].
According to the results of the ACDS obtained in the present study, only 26,7% of patients demonstrated high adherence to therapeutic recommendations, while the majority (over 50%) presented a moderate level. Quality of life was assessed the highest in the environmental domain, and the lowest in the area of social relationships. Physical and psychological condition received average ratings. The respondents primarily indicated the need for: i) longer visits, ii) easier access to the nurse, and iii) a bigger number of specialist consultations. It is widely known that healthy lifestyle choices delay disability in older patients, and thus the immediate need to implement social and community support. A healthy lifestyle should be encouraged and reinforced, especially at the primary care level [24]. Current studies have shown that health education and dietary consultations were rarely provided, and patients’ expectations of nursing staff included the need to extend the time spent with patients during visits. The need for frequent and longer nursing visits postulated by seniors is probably related to their socio-existence conditions. It should be emphasized here that most of the respondents are people living alone, and it cannot be ruled out that the extended nursing visit time they postulated would also include health education. Similar to other studies [4, 8, 11, 16], the current findings confirm that educational and rehabilitative activities, as well as an individualized approach, are essential for improving the quality of life of older adults. Therefore, elderly people suffering from chronic diseases should be a specific target group for health promotion and disease prevention programs [24].
Summary
The conducted study proves that elderly patients with chronic diseases are characterized by a high demand for comprehensive nursing care. Seniors primarily point to the need for more frequent nursing visits and longer time devoted during these visits, which reflects their actual health and care needs. Along with the prolongation of the duration of chronic disease, a clear exacerbation in the patient’s level of independence is observed. The longer they suffer, the more they report difficulties in daily activities, which indicates the progressive nature of the disease and the growing care needs. Most of the surveyed patients positively assess the quality of the nursing care they receive, which confirms the effectiveness and professionalism of the nursing staff. It is important that the high assessment of the care’s quality does not depend on the patient’s level of education. The moderate level of therapeutic adherence among patients suggests the need to further support them in systematically following medical recommendations. Only every fourth patients adhere to the recommendations exemplary, which may affect the effectiveness of therapy and health conditions in the long term. The study results also suggest that the quality of life of patients with chronic diseases is influenced by many factors, among which social relationships were rated the lowest. Although the physical and environmental condition was assessed relatively well, the collected data indicate the need for greater social support and activation of the elderly.
In conclusion, elderly people who suffer from chronic diseases have high nursing needs requiring comprehensive care. Therefore, there is a need for further actions aimed at improving the quality of life and the effectiveness of nursing care in this group of patients.

 POLSKI
POLSKI