Introduction
Type 1 diabetes mellitus (T1DM) is one of the most common chronic diseases in childhood, with an ever-increasing prevalence worldwide [1]. Although late complications of the disease do not usually appear before reaching adulthood, it remains necessary to prevent them from an early age by balancing maintenance of strict glycaemic control and avoidance of episodes of hypoglycaemia. Treatment based on insulin replacement therapy depends on patients’ and caregivers’ compliance and poses a threat of misuse. As a result, patients may develop life-threatening conditions like diabetic ketoacidosis (DKA) and severe hypoglycaemia [2]. The aforementioned issues might be a result of coexisting mental disorders, which are more prevalent in children suffering from diabetes than in the rest of the paediatric population [3, 4]. Depression and anxiety disorders are the highest in prevalence, but T1DM minors are also at risk of eating disorders, substance misuse, and personality disorders [4]. Moreover, it is believed that T1DM increases the risk of suicidal thoughts or attempts [5,6].
Another factor crucial for satisfactory glycaemic control in adolescent patients is combining parental involvement and support with accurate self-management [7]. Finally, one cannot forget the health care professionals’ involvement in the therapeutic process, providing comprehensive diabetes education for the child and family combined with nutritional management and regular screening for complications [8]. Because acute glycaemic complications account for the majority of concerns in the management of T1DM in children and adolescents, special attention during this challenging time of development is required to prevent deteriorations resulting in the necessity for acute hospitalizations and intensive care unit treatment.
With the onset of the global COVID-19 pandemic, declared by the World Health Organization (WHO) on 11 March 2020, the Polish Government announced on 12 March 2020 the closure of educational institutions across the country and the implementation of online education. The schools did not reopen for many months, disrupting the social interactions and everyday lives of schoolchildren. To suppress the spread of the novel virus, social distancing and quarantine measures were applied, including travel restrictions, prohibition on gatherings, with consequent impairment of economic and social activity. The pandemic limited in-person access to health facilities and forced the implementation of online medical appointments. Starting on 25 March 2020 the national authorities tightened lockdown restrictions, allowing citizens to leave their homes only if absolutely necessary. Minors during this time were ordered to stay indoors unless accompanied by a legal guardian. Deployment of the nationwide lockdown particularly affected the at-risk population suffering from chronic conditions, which includes T1DM paediatric patients [9, 10]. This situation forced them to come face to face with another coping challenge caused by emotional distress, psychosocial disruptions, and uncertainty about the future [9, 11].
Aim of the study
The aim of this study is to assess how the COVID-19 pandemic influenced the incidence and causes of acute hospitalizations and emergency room visits in adolescents with established type 1 diabetes mellitus, as well as to characterize the admitted population.
Material and methods
The study was conducted as a retrospective evaluation of acute hospitalizations and emergency room visits of 39 T1DM patients diagnosed based on the Polish Diabetes Association criteria, which took place between 1.01.2018 and 31.12.2021. The inclusion criteria were ICD-10 code E.10, disease duration of more than one year, patients between 15 and 17 years of age, and acute deterioration of glycaemic control. Patients with infectious causes of deterioration and newly established diagnosis were excluded from our study. We also collected anthropometric data, as well as the following: the cause of admission, age at diagnosis, coexisting illnesses (thyroid dysfunction, coeliac disease, lipid disorders), insulin administration method, daily insulin dose, COVID-19 infection and vaccination status, acid-base balance parameters (pH, bicarbonate concentration), glucose blood level, HbA1c, evidence of ketonuria, and symptoms at admission. Data on psychosocial problems of the patients were obtained from the history taken during the admission to the hospital.
BMI percentile values were determined based on Palczewska BMI charts for the Polish population. The BMI Z-score was calculated using International Obesity Task Force (IOTF) reference charts.
Diabetic ketoacidosis (DKA) was defined as hyperglycaemia (blood glucose level >11 mmol/l) and venous blood pH level < 7.3 and/or bicarbonate concentration < 15 mmol/l. The severity of DKA was determined based on the ISPAD criteria: mild (pH < 7.30 or bicarbonate <15 mmol/l), moderate (pH < 7.20 or bicarbonate <10 mmol/l), and severe (pH < 7.10 or bicarbonate <5 mmol/l) [12]. Hypoglycaemia in patients with T1DM was defined as a measured plasma glucose concentration ≤ 70 mg/dl (3.9 mmol/l).
The population was subsequently divided into 4 groups based on the calendar year of hospitalization (2018, 2019, 2020, 2021), and into pre-pandemic (2018 and 2019) and pandemic (2020 and 2021) groups. Additionally, 6 patients hospitalized in 2021 formed another group based on their unique psychosocial causes for hospitalization. This group was analysed both as a part of the year 2021 group and separately.
Data processing and statistical analysis were performed using Statistica 13 PL software. Statistical significance was set at p < 0.05. Normality was assessed using the Kolmogorov–Smirnov and Lilliefors tests. Variables with a normal distribution were analysed using t-tests and ANOVA and reported as mean ± standard deviation (SD); those without normal distribution were analysed using the Mann–Whitney U test and Kruskal-Wallis ANOVA and reported as median with interquartile range (IQR). χ2 test was used to evaluate frequency data.
The study was conducted in accordance with the Declaration of Helsinki and approved by the Jagiellonian University Ethics Committee (approval number 1072.6120.130.2022). No consent obtained from participants or legal guardians was necessary because all the data were fully anonymized.
Results
The study included 39 patients (16 males, 41%) between 15 and 17 years of age. The numbers of patients for consecutive years were as follows: 2018 – 14, 2019 – 9, 2020 – 5, and 2021 – 11. The mean age of our patients was 16.1 ± 0.88 years, the mean age of diagnosis was 8.3 ±3.9 years, and the mean disease duration was 7.9 ±3.7 years. The mean BMI was 22.1 ±3.2 and the mean BMI Z-score was 0.59 ±0.9. The median blood glucose level at admission was 15.9 ±10.5 [mmol/l]. Coexisting chronic diseases were diagnosed in 24 patients (58.5%) – the most common were as follows: lipid disorders – 9 (23%), autoimmune thyroid disease – 5 (13%), and coeliac disease – 6 (15%). Patients were administered insulin through multiple daily injections (26, 67%) or with the help of an insulin pump with continuous subcutaneous infusion (11, 28%). DKA was diagnosed in 14 (36%) of the admitted patients.
Detailed population characteristics for all the study groups are presented in Tables I and II.
Table I
Detailed characteristics of pre-COVID-19 and COVID-19 populations of adolescents with type 1 diabetes
Table II
Detailed characteristic of the studied population of adolescents with type 1 diabetes divided by calendar year
Hospitalization incidence
There were no statistically significant differences between the number of hospitalized patients in the pre-COVID and COVID populations. Separate analysis of admissions in each year revealed a significant difference only been between the years 2018 and 2020 (14 vs. 5, p < 0.05).
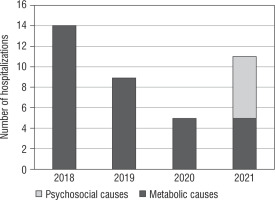
However, it is worth underlying that 6/11 patients (55%) hospitalized in 2021 were admitted due to unique psychosocial causes (attempted suicide with the use of insulin, inflicting self-harm, propranolol intake because of anxiety, and drug use). After excluding these hospitalizations, a significant decrease in the number of acute hospitalizations in the COVID period (p < 0.05) was observed (Fig. 1).
COVID vs. pre-COVID
There were no significant differences between the pre-COVID and COVID population, save for the proportion of patients with lipid disorders, which was higher in the pre-COVID group (35% vs. 6%, p < 0.05) (Table I).
DKA
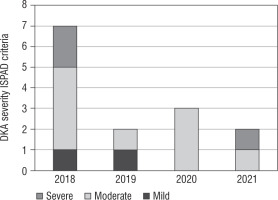
The incidence of DKA episodes did not statically differ between the pre-COVID and COVID populations, or between calendar years. Similarly, no significant difference was found between the proportion of DKA patients and all patients hospitalized in a given group (Table II).
No difference was found between pre-COVID DKA patients (from 2018 and 2019) and COVID DKA patients (2020 and 2021) in terms of biochemical and anthropometric measurements (Table III).
Table III
Clinical characteristics of patients with diabetes ketoacidosis
The incidence of DKA categorized by severity based on ISPAD criteria is shown in Figure 2.
Sex
Women displayed a lower concentration of HbA1c in comparison to men in the general study population (8.4% vs. 10.3%).
Psychosocial causes
The 6 patients comprising this group were all admitted in 2021. Their clinical characteristics are presented in Table IV. They were predominantly female (5/1), and all of them were treated with multiple daily injections of insulin. Four female patients displayed signs of self-harm, one female used amphetamine, and one male was severely intoxicated (blood alcohol content 2.12‰). They did not, however, present any significant differences with regards other parameters when compared to other patients admitted in 2021 or more generally in the COVID period.
Table IV
Characteristics of adolescents with type 1 diabetes and psychosocial disturbances
Discussion
We observed that during the COVID-19 pandemic the incidence of acute hospitalizations and emergency room visits did not increase compared to the time before the outbreak. Contrary to the predictions made early in the pandemic, forecasting a rise in deteriorations of the disease [13], we did not observe a statistically significant difference in the number of acute admissions in the years 2020 and 2021 (16) in comparison to 2018 and 2019 (23).
Our results are corroborated by recent papers that report no change in hospitalization frequency from 2019 to 2020. A paper by Choudhary et al. described a population in a large urban children’s hospital in Dallas, and a study by Rabbone et al. analysed a cross-sectional survey of all Italian paediatric diabetes centres [14,15], but only one study, conducted by Sarıkaya et al., showed an increase in the frequency of diabetes-related emergency admissions [16].
There were also no significant differences in glycaemic control parameters or in the incidence and severity of DKA between the pre-COVID and COVID populations in our study. This stands in opposition to some reports of an increased incidence of DKA during the pandemic [17, 18]. Additionally, although without statistical significance, we observed that the highest blood glucose level readings at admission were all recorded in the pre-COVID group, and the number of DKA incidents in the pre-pandemic population was nearly double that of the COVID group. This might point to a beneficial effect of the pandemic on acute hospitalization rates. However, it is worth pointing out that mild cases of DKA might have been underreported during the pandemic, due to restricted access or fear of reporting to healthcare facilities and consequent correction at home.
Although the trends in recently published research are inconsistent, the majority indicated no deterioration or even an improvement in the management of T1DM patients during the COVID-19 pandemic [13, 19–23]. It is believed that telemedicine visits, use of advanced diabetes technologies (CGM, FGM, hybrid close loop), and improved self-care, as well as parental involvement, significantly contributed to better glycaemic control [15, 24]. Considering that adolescence is a time of growing independence, which in turn increases the risk of poor disease control, the forced quarantine under parental supervision might provide a beneficial effect [13]. Moreover, introducing regular, balanced dietary customs, non-omission of insulin, and decreased school-related stress also seem to play an important role in proper diabetes management [21].
Much remains to be discussed about the influence of psychosocial factors on T1DM management. We observed that 6 out of 11 patients hospitalised in 2021 experienced diabetes deterioration as a result of emotional distress. This group consisted predominantly of females (5 females, 1 man), 4 of whom displayed signs of self-harm and one of whom attempted suicide with the use of insulin. This sex disproportion is in line with previous research, which reported that women were at a greater risk of mental health decline during the pandemic. It has been hypothesized that adolescent girls depend primarily on their social networks for support, which might have been greatly disrupted by the lockdown and implementation of on-line schooling [25]. As mentioned above, we also observed one suicide attempt episode, which according to the literature seems to be an emerging problem [17, 26]. In a study conducted by Alessi et al. it was described that up to 5.2% of T1DM patients reported suicidal thoughts during a one-month period of the pandemic [26]. In general, it has been assessed that T1DM is associated with a fivefold increase in the risk of anxiety during the pandemic, supposedly as a result of concerns about severe disease course, lack of insulin or medical supplies, and economic uncertainty [27]. The increased incidence of suicidal thoughts and distress caused by COVID poses a unique challenge for clinicians overseeing T1DM patients, because they are not only at a greater risk of developing mental health disorders, but also possess the means to commit suicide in the form of insulin overdose [26].
Although we did not find significant differences in the biochemical parameters of these patients compared to other COVID-period hospitalizations, it is worth noting that 3 of them were at risk of developing hypoglycaemia (propranolol intake, attempted suicide with insulin overdose, amphetamine use). However, pre-hospital interventions might have altered their blood glucose level at admission.
Finally, if not for the hospitalizations due to psychosocial causes, we would see a significant decrease in the number of hospitalizations in the COVID period in comparison to the pre-COVID period (10* vs. 23, p < 0.05). This leads us to believe that the pandemic might have contributed to a decrease in acute hospitalizations, but this was masked by a sharp increase in hospitalizations due to emotional distress.
Despite the large number of reports on the influence of the COVID-19 pandemic on the management of T1DM in children and adolescents, the amount of information on the changes in hospitalization frequencies is very scarce. According to a meta-analysis conducted by Wafa et al., out of 21 included studies, all used continuous or flash glucose monitoring (CGM/FGM) records, self-monitoring blood glucose, or hybrid close loop as measurement methods and reported outcomes including blood glucose level, HbA1c concentration, time-in-range (TIR), time-above-range (TAR), or time-below-range (TBR) values [19]. To the best of our knowledge, only 3 published studies concern the influence of the pandemic on hospitalization frequencies in youths with established T1DM [14–16]. However, the first such report, by Choudhary et al., included inpatient admissions and observations but excluded emergency department visits from the number of hospital admissions [14]. The second one evaluated patients under 15 years of age during the first 40 days of the pandemic [15]. The third one, by Sarıkaya et al., evaluated admissions to the emergency service related to diabetes [16], but neither of the aforementioned studies focused precisely on the adolescent population. In the context of the age of the studied population and a focus on the incidence of acute hospitalizations, our study remains unique.
We are also aware of the limitations of the study because our observations are limited to only one centre. Because we collected the data retrospectively, some of our patients lack a complete set of studied parameters. Secondly, the study was performed on a small sample of patients, and therefore many results did not reach statistical significance. Another limitation is that the time of observation was limited only to the point of admission to the hospital or to the emergency room and it did not provide us with more complex data on psychological functioning of our patients. Finally, we did not assess continuous glucose monitoring records, and consequently we were unable to evaluate time in range (TIR) values.
Conclusions
Excluding the hospitalizations due to psychosocial causes, we could see a significant decrease in the number of hospitalizations in the COVID period in comparison to the pre-COVID period. This leads us to believe that increased supervision during the pandemic might have prevented some of the episodes of severe disease decompensation, but this was masked by the sharp increase in hospitalizations due to emotional distress. Thus, ensuring patients’ psychological well-being should be an important factor in the treatment of T1DM, especially in the challenging time of global pandemic.
 POLSKI
POLSKI