Introduction
Urinary incontinence (UI) is one of the more common problems in women occurring at different ages, especially older women, which causes not only physical problems, but also psychological, social, economic, and poor quality of life for these women[1].
Urinary incontinence paves the way for a range of health problems, from the discomfort of constant wetting to social isolation and depression in women[2].
UI is defined as the involuntary loss of urine. The condition can occur in both sexes, but is more common in women. There are many known risk factors for incontinence. For women, multiple pregnancies, previous vaginal births and menopause are known risk factors for incontinence. To diagnose urinary incontinence, there are three steps, including a patient interview, physical examination and laboratory tests. Treatment options for incontinence include conservative, medical and surgical treatments, and all guidelines recommend trying conservative treatment before medical or invasive surgical treatment. Conservative therapies include behavioral therapy and physical therapy[3].
The most common form of incontinence is stress urinary incontinence, characterized by uncontrollable urine leakage during coughing, sneezing, laughing and exercise. Its severity can vary from popping single drops during significant exertion to urine leakage while walking or even at rest. Urgency urinary incontinence is caused by an uncontrollable contraction of the bladder, most often in the course of overactive bladder or urge incontinence due to lowering of the bladder (cystocele), while mixed forms of incontinence are the co-occurrence of symptoms of stress incontinence and overactive bladder[4].
We distinguish between two forms of overactive bladder - the so-called dry form, when pushing and frequent urination are not accompanied by urinary leakage, and the so-called wet overactive bladder, when one of the complaints is urinary leakage in the mechanism of urgency4.
Urinary incontinence is common in postmenopausal women. In order to deal with this problem, it is necessary to improve screening for it [5].
Despite the aggravation of the ailment, it often happens that women, due to an embarrassing feeling of shame, do not seek any counseling and suffer for many years, trying to combat the unpleasant effects of the condition on their own. The problem of incontinence affects sexual, professional, social or family life and can be associated with a deterioration in the quality of life for these women.
Over the past five years, women’s awareness of the problem in question has been intensively raised through numerous information campaigns, including media coverage. It is important to provide holistic strategies for the prevention and treatment of urinary incontinence in women, especially in the rural population.
The purpose of this study was to assess the prevalence of urinary incontinence symptoms in co-women living in rural and metropolitan areas, and to determine the relationship between place of residence and urinary incontinence and reporting of this problem to a physician.
Material and methods
The study involved 492 women reporting to their primary care physician from a rural environment in the towns of Niebylec and Dębowiec in Subcarpathian province and the city of Kraków. Prior to the study, the patients gave their voluntary consent to participate in the study.
The study was carried out between April and September 2017, using a diagnostic survey method with a survey questionnaire of our own design, which was not validated. It took into account basic data such as age, education, residence, weight and height, and obstetric history. All women who attended an appointment with their POZ (National Health Care) physician on a given day (three times a week) were asked to complete the questionnaire.
The questionnaire was anonymous, completed by the patients, and included questions about the symptoms of incontinence and reporting the problem to the POZ physician and undertaking possible treatment with a physiotherapist or specialist. The questions concerned the presence of a given incontinence symptom or whether it had ever occurred in a given patient.
Patient selection for the study was based on the fact that all women who agreed to participate in the study and correctly filled out the questionnaire and answered all the questions in it were included in the study group.
The percentage of refusals to complete the questionnaire was high at 25%.
Spearman’s rank correlation coefficient, Student’s t-test, Pearson’s correlation coefficient and non-parametric tests of significance of differences (Mann Whitney U, Kruskal Wallis), as well as the Chi2 test and Fisher’s test for self-reported variables were used for detailed analysis. The significance level was taken for alpha = 0.05.
The work was approved by the Bioethics Committee at the Krakow Academy by Resolution No. 23/2017 dated 22.06.2017 on the issuance of opinion No. KBKA /23/0/2017.
Results
The study group consisted of: 49% women living in a rural environment of Podkarpackie province and 51% of a large city of Małopolska province. The largest percentages were those with higher education (35%) and secondary education (33%). Women with vocational and primary education accounted for 26% and 6%, respectively. The most represented group was women over 50 years of age - 59%. The 35-50 age bracket included 28%, and under 35 years of age 13% of the respondents. In the study group, the largest percentage were women with a BMI (Body Mass Index) indicating overweight, 46% from the city and 32% from the countryside, respectively. Obesity was found in 35% of respondents from the city and 15% from rural areas. The data presented are illustrated in Table 1.
Table 1
Sociodemographic data, past births by place of residence of women.
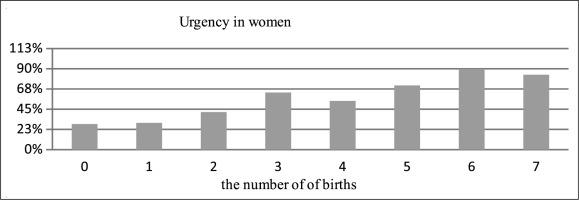
Episodes of urge incontinence were reported by 30% of women giving birth only once, more than 60% of women after 3 deliveries and as many as 70% after 5 deliveries. Urge incontinence affected as many as 90% of women after 6 deliveries (Fig. 1).
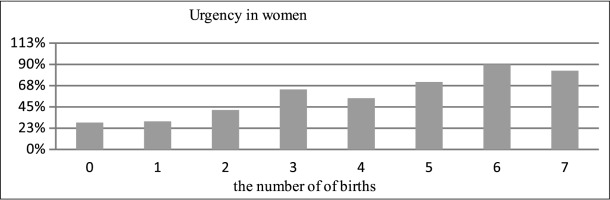
A similar relationship is found in the appearance of uncontrolled urinary leakage, these are patients with all types of UI. In women who gave birth at least twice, more than 20% showed urinary urgency. 30% of women after four deliveries and 70% after six deliveries admitted to having this problem (Fig. 2).
Considering the type of delivery, equally 48% of women giving birth by natural force and 48% after cesarean section reported incidents of urgency.
In the study, statistically significant differences were observed between the group of women living in the city and women in the countryside in the occurrence of urinary urgency (p>0.001), the occurrence of pooping after sneezing, coughing (p>0.001) and in using the toilet at night (p>0.001) at a significance level of less than 0.05. Women living in the countryside (51%) were more likely to experience urinary urgency than women living in the city (31%). In contrast, women living in the city were more likely to report post-voiding after either sneezing or coughing, i.e., symptoms of stage I stress urinary incontinence. Women living in rural areas, on the other hand, are more likely to use the toilet at night while urinating.
In the questionnaire survey, no differences were observed between groups of women living in urban and rural areas in the incidence of pushing and urinating, uncontrolled urination, and the incidence of urinating while running, dancing and exercising. The results presented are illustrated in Table 2.
Table 2
Place of residence and prevalence of urinary incontinence.
In addition, it was also analyzed which women are more likely to report the problem to a doctor and then more likely to undergo treatment depending on where they live. The problem presented is in Table 3.
Table 3
Place of residence, and reporting the incontinence problem to the GP, suggesting or undertaking treatment.
| REPORT THE PROBLEM TO YOUR FAMILY DOCTOR | PROPOSING TREATMENT | UNDERTAKING TREATMENT | ||
|---|---|---|---|---|
| PLACE OF RESIDENCE | VILLAGE (N=240) | 16,20% | 13,30% | 11,70% |
| CITY (N=252) | 68,30% | 11,90% | 1,60% | |
The coefficients indicate that there is a significant relationship between place of residence and reporting the incontinence problem to the family doctor (χ2 (1) =135.72, p<0.001). The value of the phi statistic indicates a strong relationship φ= 0.52, p< 0.001. Women living in the city were more likely to report the problem to a doctor.
In contrast, there is no relationship between the suggestion of treatment and place of residence, while the fact of living in a rural area positively influences the initiation of treatment for ailments (χ2 (1) = 20.54, p<0.001). The value of the phi statistic indicates a moderate relationship φ = -0.20, p< 0.001 between place of residence and taking treatment.
It was also investigated whether there was a correlation between the level of education and women taking treatment. The data presented are illustrated in Table 4.
Table 4
Education of respondents and their uptake of incontinence treatment.
| EDUCATION | UNDERTAKING TREATMENT |
|---|---|
| PRIMARY (N=30) | 30,00% |
| PROFESSIONAL (N=130) | 6,20% |
| MEDIUM (N=162) | 5,60% |
| HIGHER (N=170) | 3,50% |
The level of education influences the uptake of treatment for urinary incontinence. Those with primary education are more likely than others to declare that they have decided to treat the ailment (χ2 (3) = 29.95, p<0.001). The value of the contingency coefficient indicates a moderate strength of the association between education and taking treatment (0.24, p< 0.001).
Discussion
One of the risk factors for urinary incontinence is past childbirth.
Kokabi and Yazdanpanah showed a twofold higher risk of postpartum stress urinary incontinence in first-born women giving birth by natural means compared to patients giving birth for the first time by cesarean section. They cite instrumental delivery and episiotomy, or perineal incision during labor, as factors determining this risk[6].
Our own results conducted among women in rural and urban settings confirmed that the number of deliveries significantly affects the incidence of urgent pushing among the surveyed respondents. 30% of women who had given birth only once admitted to this episode, over 60% were women after three deliveries, 70% after five deliveries, while up to 90% of women after six deliveries admitted to the occurrence of urgency. A similar relationship emerges with the onset of uncontrolled urinary leakage.
Similarly, Gyhagen et al. showed that both pregnancy and natural childbirth were associated with an increased risk of urinary incontinence in the later period - 20 years after delivery. Natural childbirth resulted in an increase in urinary incontinence of up to 43% compared to the non-birth group. Caesarean section compared to natural childbirth was associated with a 30% reduction in urinary incontinence and a 35-52% reduction in more severe degrees of incontinence regardless of age[7].
All women should be increasingly aware that this incontinence problem can be effectively treated - both pharmacologically, physiotherapeutically and surgically. Therefore, it is very helpful to educate women about the treatment options for incontinence, as well as widespread preventive campaigns dedicated to the prevention of UI among women even before childbirth and in the second group before menopause.
The level of education significantly affects taking treatment for incontinence. Proprietary results show that people with primary education are more likely than others, such as those with higher education, to declare that they have decided to treat the ailment. It is worth noting that this may be due to the fact that these women are more likely to have urinary urgency, and therefore the ailment is already bothersome enough for them to report the problem to a doctor.
UI is one of the more common problems in women, especially older women.
A study by Murukesu et al. found that urinary incontinence is common among older women living in the community. However, its impact on quality of life was higher among older women in rural populations. In the study, older women living in rural areas faced greater limitations in role, social and physical aspects of daily life due to incontinence. This suggests that specially tailored strategies for preventing and treating incontinence may be co-founded, especially in older women living in rural areas.
The prevalence of incontinence was 16% and 23% among older women living in urban and rural areas, respectively.
Among older women in rural settings, the prevalence of incontinence in the large-scale study conducted (23%) is considered high compared to a smaller earlier study (3%) that was conducted in a single US state with fewer participants. The prevalence of incontinence in the conducted study is between the 10% reported in India, 40% in Spain and 36% in the United States among rural populations[7].
The study by Najafi et al. showed that the prevalence of urinary incontinence among the subjects was 24.9%, and stress incontinence was the most common type of incontinence (40.2% of all elderly patients). Very similar to previous studies, age, body mass index (BMI), constipation, history of cesarean section, hypertension and use of angiotensin receptor blockers were found to be factors that increased the likelihood of urinary incontinence in the study population[8].
Studies conducted by Resshaya et al. presents very similarly, that the prevalence of urinary incontinence was 16% and 23% among older women living in urban and rural areas, respectively.
UI is more prevalent and has a more profound impact on the quality of health of older women in rural settings. Risk factors for incontinence were ethnicity and chronic constipation among older urban and rural women, respectively. It is important to provide holistic strategies to prevent and treat urinary incontinence in older women, especially in rural populations[9].
Analysis of our own results showed that women with urgency were far more likely to seek information about incontinence treatment than the other respondents, while women living in urban areas were more likely to report incontinence to a doctor.
It seems that women who live in the city are more likely to use the health care system, and therefore may have a better relationship with their doctor, and thus are more likely to seek treatment for the ailment.
In the self-reported study, women living in rural areas were significantly more likely to be multiparous and had 40% higher education and 30% secondary education. Women from the city had a significantly higher BMI (46% overweight, 35% obese) while half of the women from the countryside were of right body weight, with 32% admitting to being overweight and 15% obese.
Research conducted by Chen et al. present that the prevalence of incontinence was 14.84% (414/2790). Among women with incontinence, 61.1% (253/414) had stress urinary incontinence (SUI), 21.5% (89/414) had urgency urinary incontinence (UUI), and 17.1% (72/414) had mixed urinary incontinence (MUI).
Conclusions of the study indicated that women who were older, lived in rural areas and had a history of gynecological diseases, hypertension or cardiovascular disease were more likely to suffer from incontinence[10].
The study, conducted by Połocką - Molińską et al., found that the prevalence of urinary incontinence in the general population was reported by 132 women (30%). Seventy-four of the 132 women had stress urinary incontinence (56%), 45 women had urinary urge (34%), and the remaining 13 women had mixed incontinence (10%). The prevalence in admitted women was reported by 38 of 108 women (35%). Twenty-four of the 38 women had stress urinary incontinence (63%), 10 women had urgency urinary incontinence (26%), and the remaining four women had mixed urinary incontinence (11%)[4].
A study conducted by Abdullah Alasmi et al. depicts those 86 (30.1%) women experienced symptoms of urinary incontinence. The women had mostly MUI. Correlations between UI and age, education level, employment status, presence of chronic diseases, chronic constipation, difficult birth history and menopausal status were significant. The overall mean score of women with incontinence on the Quality of Life with Urinary Incontinence Questionnaire was 73.62 ± 24.36, and the most affected quality-of-life domain was social perplexity. The present study found that UI is common in Turkish women and worsens their quality of life[11].
Conclusions
The number of past births affects the problem of urinary incontinence.
Women living in rural areas are more likely to have urgency urinary incontinence while women from the city are more likely to suffer from stress urinary incontinence. In fact, a smaller percentage of these women may have sought help and not made appointments with their POZ and a larger percentage of women did not agree to complete the questionnaires, as evidenced by the percentage of refusals to participate in the survey. Therefore, it is important to provide holistic strategies for preventing and treating urinary incontinence in women, especially in the rural population.
Women living in urban areas are more likely to report the problem to a doctor, while there is no correlation between the proposed treatment and place of residence.
The level of education influences the uptake of incontinence treatment. Persons with primary education are more likely than others to declare that they have decided to treat the ailment. It may be that people with non-primary education did not report an incontinence problem and did not want to fill out the questionnaire, or there was an incontinence problem but they did not want to comment on it.
Recommendations for nursing practice
It is recommended that women receive regular primary care and specialist consultations with gynaecologist, combined with education on the problem of urinary incontinence. As urinary incontinence is twice as common among women after natural childbirth, and the percentage of women affected increases with age, and symptoms most often appear during the menopausal period, education on prevention and treatment of urinary incontinence is recommended for all women. In spite of the increasing severity of the problem, it is often the case that women do not seek any specialist advice due to embarrassment and suffer for many years, trying to manage the unpleasant effects of incontinence on their own, especially when the problem affects every sphere of a woman’s life - sexual, professional, social or family.

 POLSKI
POLSKI