Introduction
Brain stem death is the leading criterion for determining death in area of modern – high-quality scientific evidence based – medicine [1]. Despite the irreversible cessation of all central nervous system functions, a patient in a state of brain stem death can be kept alive by means of organ function support therapy, which enables organ removal and transplantation procedures to be carried out [2]. Organ donation currently represents the basis of clinical transplantology remaining the irreplaceable medical technology for numerous terminal organ failures, such as heart, kidney, liver or lung failure [3]. In the field of intensive care, a patient diagnosed with brain stem death becomes a potential organ donor, in accordance with strict biomedical and formal criteria [4]. The role of highly qualified nursing staff is therefore undergoing a significant transformation – no being longer focused on treatment, but also on optimally securing the vital functions of organs and tissues. It can be said that in this situation, the nurse acts as a guardian of organ quality, an advocate for patient dignity and a caregiver for the family [5].
What is particularly important the aforementioned, sophisticated cognitive service encompassing not only medical procedures, but also communicative and emotional elements, especially in the context of contact with the family of the donor [6]. Nursing staff play an exclusive role as crucial intermediaries between the medical team and the patient’s family, supporting them in understanding the diagnosis of brain death and making decisions regarding consent to donation [7]. In an era of developing medical technologies and growing transplant needs, it is necessary to deepen the knowledge and skills of nursing teams in the field of donation procedures [8]. Understanding the essence of nursing care severed for a brain-dead donor is crucial to ensuring high-quality medical services, effective organ allocation and maintaining high ethical standards [9].
Therefore, the aim of this study was to assess the complexity and leading determinants of an assistive, supportive, and enabling actions facilitating key members of the interdisciplinary medical team – highly qualified nursing staff, to perform one of the most difficult medical challenges – specialised care implemented in patients with confirmed brain stem death, qualified as an organ donor.
Material and methods
3.1. experimental tool – survey questionnaire
This study used a diagnostic survey method, with an original questionnaire as the primary research tool, consisting of 20 precisely defined and selected research questions. The questionnaire consisted of two parts. The first part was a personal data sheet (referring to gender, age, education and length of service), while the second part, which was substantive, referred to the essence of nursing care for patients with confirmed brain stem death [10].
3.2. Study protocol and study group
The first stage of the study protocol involved selecting the appropriate methods, techniques and research tools, followed by conducting a questionnaire survey of our own design among 96 nurses working at the Clinical Department of Anaesthesiology, Intensive Care and Pain Management at the Mazovian Specialist Hospital in Radom. The research was conducted between 26 March 2025 and 12 June 2025. The respondents were clearly informed about the anonymity and purpose of the research. The final stage was to verify the results obtained.
The assessed study group consisted mainly of women (90.6%), with male nurses accounted for 9.4% of individuals, 28.1% of respondents were aged 31–40 (21.9%), while 22.9% were aged 41–50. The subgroup of individuals aged 51 and over accounted for 27.1%. Individuals’ education referred to master’s degree plus specialisation was 46.9%, bachelor’s (27.1%), master’s degree (17.7%) and bachelor’s degree plus specialisation (7.3%). The study included individuals with over 20 years of nursing experience (33.3%), less than 5 years of nursing experience 26.0%), 5 - 10 years of nursing experience (22.9%) and 11 - 20 years of work experience (17.7%). In terms of nursing experience in the intensive care unit (ICU), the largest group consisted of respondents with less than 5 years of experience (37.5%). Respondents with more than 20 years of experience accounted for 27.1%, while 18.8% and 16.7% of participants declared experience in the range of 5–10 years and 11–20 years, respectively. Described socio-demographic characteristics of the study group – part one is presented in table 1 and in table 2.
Tab. 1
Socio-demographic characteristics of the study group – part one.
| Number of individuals included in the research protocol N % | |||
|---|---|---|---|
| Gender | Females | 87 | 90,6% |
| Males | 9 | 9,4% | |
| Age range | ≤ 30 | 27 | 28,1% |
| 31-40 | 21 | 21,9% | |
| 41-50 | 22 | 22,9% | |
| ≥ 51 | 26 | 27,1% | |
| Total number of individuals | 96 | 100% | |
Tab. 2
Socio-demographic characteristics of the study group – part two.
3.2. Statistical Analysis
The results of the study were presented in terms of qualitative data using frequency and percentage, and quantitative data using mean, standard deviation, median, and minimum and maximum values. Pearson’s chi-squared (x2) test was used to assess the statistical significance of the variables. StatSoftStatistica 13.1 PL tool was applied [11, 12].
Results
It was observed that 65.6% of nursing staff possessed experience of multiple care for deceased, qualified transplant donors, with isolated cases of such professional experience reported by 16.7% and no experience in 17.7%. Repeated care for deceased, qualified transplant donors was more often provided by those with longer work experience (p<0.0001), respondents with longer experience and practice in the ICU (p<0.0001), as well as respondents with a second degree and completed specialisation training, as shown in table 3.
Tab. 3
Individuals’ experience in the field of deceased donors care qualified for transplantation.
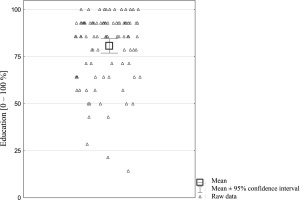
It was also observed that the nurses surveyed answered correctly approximately 80.7% of the questions analysed, which may suggest advanced level of knowledge concerning the nursing care of patients with brain stem death (organ donors). The lowest score achieved was 14.3% correct answers and the best was 100% (achieved by 13 respondents, 13.5% of the total). The respondents usually answered correctly on average 90-100% of the analysed issues, the aforementioned outcomes are presented in figure 1. Moreover, it was found that the vast majority of nursing professionals represented advanced level of knowledge on the caring for organ donors (76.0%). Selected subjects showed moderate level of knowledge (19.8%), and a few low levels of knowledge (4.2%). A highly advanced level of knowledge was demonstrated by nursing staff with long service (p<0.0001) and those with experience in caring for deceased donors (p<0.0001). A moderate level of knowledge was significantly more common among respondents with less than 5 years of overall nursing experience (p<0.0001), as well as those with less than 5 years of experience in the ICU (p<0.0001), and those with a bachelor’s degree without completed specialised training in nursing (p<0.0001), as shown in table 4.
Tab. 4
Respondents’ knowledge on nursing care of patients with brain death (organ donors).
The vast majority of respondents stated that the parameters necessary for caring for the deceased donor include the estimation of SpO2 (99.0%), body temperature (99.0%), and invasive blood pressure measurement (96.9%). Less frequently, respondents indicated parameters such as central venous pressure (55.2%), hourly diuresis (20.8%), and much less frequently intra-abdominal pressure (15.6%), intracranial pressure (12.5%), and non-invasive blood pressure measurement (7.3%). Central venous pressure (CVP) was significantly more often indicated by younger respondents (p<0.0001), with shorter overall and ICU experience (p<0.04 and p<0.0001), as well as respondents with first-degree education and without completed specialisation training (p<0.03), and those without experience in caring for organ donors (p<0.02). Similar relationships were found for ICP (intracranial pressure), IAP (intra-abdominal pressure) and hourly diuresis as vital signs necessary for the care of deceased donors (p<0.05). NIBP (non-invasive blood pressure) was significantly more often indicated by respondents with less than 5 years and 11-20 years of experience (0<0.02). IBP (invasive blood pressure) as a parameter necessary for assessment in the circumstances described was significantly more often indicated by respondents older than 30 years (p<0.05), as well as by respondents with longer overall professional experience (p<0.05), as well as by respondents with experience in caring for deceased patients – donors (p<0.0001), as shown in table 5, table 6 and table 7.
Tab. 5
Respondents’ knowledge on vital parameters necessary to determine in deceased donors, in relation to gender and age.
Tab. 6
Respondents’ knowledge on vital parameters necessary to determine in deceased donors, in relation to the level of education and professional experience
Tab. 7
Respondents’ knowledge on vital parameters necessary to determine in deceased donors, in relation to the nursing experience in the field of ICU as well as to professional experience in the course of care for deceased donors
Achieved results revealed that the majority of respondents indicated the need to administer warm infusion fluids (90.6%) to a patient with a temperature of 35.8°C, more often among older respondents (p<0.04), those with longer nursing experience and those practicing in the ICU (p<0.001 and p<0.01), as well as respondents with specialisation (p<0.03). Selected respondents stated that no action should be taken in this regard in order to maintain normothermia (9.4%), as shown in table 8. It was also observed that nurses most often emphasised the need to change the patient’s status in the documentation to an organ donor after confirmation of death (90.6%), statistically significantly more often by respondents with completed specialist training and Master’s degree (p<0.04), as well as in case of professionals with 5-10 years of nursing experience (p<0.03). Negative responses were less frequent (9.4%). The nature of the remaining correlations was statistically insignificant, p>0.05, as shown in table 9.
Tab. 8
Respondents’ knowledge concerning professional procedures undertaken by nurses to maintain normothermia in the organ donors, in relation to chosen variables.
Tab. 9
Nurses’ knowledge concerning patient’s status in medical records after death confirmation and classification as an organ donor by nurses, in relation to chosen variables.
It was found that the majority of respondents stated that in the event of cardiac arrest in a deceased donor, they would rule out the administration of atropine, indicating the need to use adrenaline (71.9%). Older respondents were significantly more likely to use adrenaline (p<0.0001), those with a specialisation in nursing and a master’s degree (p<0.002), as well as those with longer experience and experience in the ICU (p<0.0001), and those with experience in donors care (p<0.0001), as shown in table 10. In addition, it was observed that the majority of respondents indicated that nurses participated in lymph node procurement by assisting surgeons in the ward while ensuring an aseptic environment (88.5%), significantly more often by older respondents (p<0.0001), those with higher education (p<0.0001), those with longer overall work experience and in the ICU (p<0.0001), as shown in table 11.
Tab. 10
Individuals’ knowledge regarding the use of atropine or adrenaline in patients with confirmed brain stem death, in relation to chosen variables.
Tab. 11
Individuals’ knowledge regarding participation of nurses in the procedure of procurement lymph nodes from a deceased donor, in relation to chosen variables.
It was also observed that chest, height and weight measurements were often indicated by nurses implementing professional care for donors (89.6%). Knowledge in the mentioned area was significantly more common among older respondents (p<0.0001), those with higher levels of education in terms of undergraduate and postgraduate degrees (p<0.0001), as well as those with longer overall professional experience and experience in the ICU (p<0.0001), as shown in table 12.
Tab. 12
Individuals’ knowledge regarding anthropometric measurements performed by nurses on the deceased organ donor, in relation to selected variables.
Moreover, he vast majority of respondents indicated bronchial tree toilet (BTT) using a closed system as the appropriate method of infection prevention (90.6%). Knowledge in this area was significantly more common among older study participants (p<0.003), those with longer overall work experience and longer experience in the ICU (p<0.001 and p<0.0001), as well as those who had completed a specialisation in nursing (p<0.01) and experience in caring for deceased donors (p<0.0001), as shown in table 13.
Tab. 13
Nurses’ knowledge regarding BTT methods in an organ donor, in relation to selected variables.
Furthermore, it was found that most nurses declared that they communicated with and supported the donor’s family (84.4%) and that this was within their competence. Significantly more often, this knowledge was possessed by respondents over 30 years of age (p<0.0001), those who had completed a specialisation in nursing (p<0.0001), as well as those with longer overall work experience and experience in the ICU (p<0.0001), and those who had cared for deceased donors in the past, as shown in table 14. It is noteworthy that most respondents classified patients with brain stem death as ASA grade VI (76.0%). Grade V (9.4%) and grade III (8.3%) were indicated much less frequently. Classification into group VI was significantly more common among older respondents (p<0.0001), those with higher education than a bachelor’s degree without a specialisation in nursing (p<0.0001), and with longer overall and ICU work experience (p<0.0001 and p<0.001), as shown in table 15.
Tab. 14
Nurses’ knowledge on communication with the family of the deceased donor, in relation to selected variables.
Tab. 15
Nurses’ knowledge on classification of patients with confirmed brain stem death into the appropriate ASA group, in relation to selected variables.
It is particularly important that almost all respondents stated that medications prescribed by a medicine doctor should continue to be administered to the deceased donor (94.8%). Correct knowledge in this area was significantly more common among respondents over 30 years of age (p<0.003), those with a master’s degree and those who had completed a specialisation (p<0.003), as well as respondents with general work experience (p<0.001) and in the ICU (p<0.03) of more than 5 years, as well as respondents with at least some experience in caring for deceased donors, p<0.0001). Negative responses regarding the discontinuation of pharmacotherapy were rare (5.2%), as shown in table 16.
Tab. 16
Nurses’ knowledge on continuation or discontinuation of pharmacotherapy in the deceased donor, in relation to selected variables.
It was also found that the majority of nurses believed that despite the difficulties of caring for a deceased donor, the focus should be on saving other people (95.8%). Negative responses were rare (4.2%), as presented in table 17. Checking identification bands (97.9%), recording tests (97.9%) to avoid laboratory and identification errors was pointed out. Less frequently mentioned were placing the name on the test tubes (95.8%), collecting and storing the material (94.8%) and providing the date and time of collection (94.8%). Occasionally, there were responses suggesting that tests could be collected in any order (7.3%), and rarely indicated that there was no need to check the identification band (2.1%). It was shown that verification of the name and surname on the test tube was indicated significantly more often by respondents with less than 5 years and more than 20 years of experience in the profession (p<0.02), presented in tables 18–20.
Tab. 17
Respondents’ knowledge on nurses’ endeavour to save the health and lives of other patients while caring for a deceased donor, in relation to selected variables.
The data analysis showed that almost all respondents indicated the need to monitor hypothermia (99.0%) and electrolyte disturbances (99.0%) and to report them to a doctor if they occur, thus being aware of their occurrence. The risk hypotension (95.8%) and urinary retention (69.8%) was also emphasised. Hypovolaemia (25.0%), hypertension (21.9%), coagulopathies (19.8%) and hyperthermia (17.7%) were indicated less frequently. Knowledge in the analysed area, especially with regard to the observation of hypovolaemia, hypothermia, coagulopathy and pulse hypotension, was significantly more common among younger respondents with less overall work experience and less experience in the ICU, and those with no experience in caring for deceased organ donors, p<0.05, as shown in tables 21 – 23.
It was also found that most nurses recommended verification of gastric retention in the case of enteral feeding (92.7%). Negative responses were rare (7.3%), as shown in table 24.
Tab. 18
Respondents’ knowledge on professional procedures undertaken to eliminate laboratory and identification errors in organ donors, in relation in relation to gender and age.
Tab. 19
Respondents’ knowledge on professional procedures undertaken to eliminate laboratory and identification errors in organ donors, in relation to education and nursing experience.
Tab. 20
Respondents’ knowledge on professional procedures undertaken to eliminate laboratory and identification errors in organ donors, in relation to ICU experience and donor care experience.
Tab. 21
Respondents’ knowledge of pathophysiological changes that should be noted by nurses caring for organ donors, in relation in relation to gender and age.
Tab. 22
Respondents’ knowledge of pathophysiological changes that should be noted by nurses caring for organ donors, in relation to education and nursing experience.
Tab. 23
Respondents’ knowledge of pathophysiological changes that should be noted by nurses caring for organ donors, in relation to ICU experience and donor care experience.
Tab. 24
Respondents’ knowledge concerning the obligation to verify the gastric retention during enteral feeding in organ donors, in relation to ICU experience and donor care experience.
Discussion
Caring for a patient with confirmed brain stem death differs significantly from traditional nursing practice. A nurse faces the challenge of caring for a biologically dead patient whose vital functions are being artificially maintained in order to preserve organs for transplantation, which in turn causes clinical, psychological and aesthetic difficulties [9]. A common challenge is sudden haemodynamic instability in the donor, which may prevent organ retrieval. This requires high alertness, knowledge of procedures and quick reactions on the part of the nurse [13]. The nurse finds herself in a situation where she must reconcile the need to care for the patient with the fact that he no longer has a chance of returning to life. This can lead to moral dilemmas, e.g. – how to react in a situation where the family does not accept the situation; – how to maintain a balance between the technical side of the procedure and respect for the dignity of the donor; – whether a patient who is formally dead deserves the same care and attention as a living person [14]. Caring for an organ donor is emotionally draining because the patient looks alive, which makes it difficult to accept the fact of death, the nurse has to deal with the suffering of the family, there is a sense of paradox – caring for a body that has no chance of recovery, but is meant to save others [9,15]. Such experiences can lead to stress, burnout and even trauma. That is why it is important for nurses to have access to psychological support and supervision [16].
The challenges faced by nurses when caring for organ donors are multifaceted. They include clinical difficulties, psychological and moral burdens, as well as communication problems related to contact with the family [7,9]. They require nurses to have high professional competence, empathy and mental resilience. At the same time, they point to the need for systemic support to minimise the risk of burnout and ensure high quality care in the donation process [17].
The results of our own research showed that the vast majority of nurses (76%) have a high level of knowledge about caring for patients with confirmed brain stem death as potential organ donors. The result obtained indicates a high level of professional preparation and awareness in the field of critical care. These data may indicate a growing level of nursing competence in the context of intensive care and the positive effects of postgraduate education in the field of anaesthesiology nursing and intensive care [18].
Different results are presented by Tabisz A., who, in a study involving 142 nurses working in anaesthesiology and intensive care units, showed that only 54.2% of respondents had a high level of knowledge about the procedure for determining brain death and organ donation, while 33.1% had an average level and 12.7% had a low level. Both Tabisz [19] and Szydło et al. [20] pointed out that despite a generally positive attitude towards the idea of transplantation, there are still significant gaps in knowledge of clinical procedures and legal aspects.
It is also worth noting that similar differences have been observed in international studies. Other authors found that only a moderate proportion of nurses correctly understood the definition of brain stem death, and a significant proportion of respondents associated it with the decision to harvest organs, indicating an insufficient level of knowledge and a need for further education in this area. In a comparative context, the results of our own research show a higher level of substantive preparation among Polish nursing Staff [21,22].
In a survey conducted among anaesthesiologists from north-eastern Poland, more than half of the respondents admitted that they did not have sufficient knowledge about determining brain death, even though they had a positive attitude towards organ donation. This result indicates that the problem of knowledge deficits in clinical transplantology affects not only nurses, but also other professional groups in the healthcare system [20,23]. Other studies show that medical students’ knowledge of brain death is still unsatisfactory, confirming that systematic education in this area should be included at all stages of medical training. In the context of nursing, these findings may justify the introduction of compulsory training modules on brain stem death recognition and care for potential donors as part of postgraduate education [24,25].
The results of the study also confirm that age, professional experience and specialisation in anaesthetic nursing and intensive care are important determinants of the level of knowledge. Nurses with relatively long professional experience demonstrated a higher level of knowledge. This phenomenon may result from more frequent contact with patients in a state of profound neurological failure and a better understanding of the clinical, ethical and legal aspects of the organ donation process [26,27].
In summary, the results confirm the high level of knowledge among nurses regarding the care of patients with confirmed brain stem death. However, the presence of respondents with average and low levels of knowledge indicates the need to continue educational activities and expand continuing education in this area. Data from domestic and foreign literature confirm that regular training, practical education and institutional support are crucial to ensuring a high standard of care for patients who are potential organ donors [28,29].
Conclusions
The professionals included in the research protocol, who had a master’s degree and completed specialisation in nursing, with relatively long work experience and practical experience in the field of intensive care, were characterised by highly advanced knowledge in the field of care for deceased organ donors. The experience gained in caring for organ donors had a highly beneficial effect on the pool of professional knowledge and the ability to implement it in practice in the course of nursing care for patients with confirmed brain stem death.

 ENGLISH
ENGLISH